Abstract
Minute prostatic adenocarcinomas are considered to be of insufficient virulence. Given recent suggestions of TMPRSS2–ERG gene fusion association with aggressive prostatic adenocarcinoma, we evaluated the incidence of TMPRSS2–ERG fusion in minute prostatic adenocarcinomas. A total of 45 consecutive prostatectomies with minute adenocarcinoma were used for tissue microarray construction. A total of 63 consecutive non-minimal, Gleason Score 6 tumors, from a separate PSA Era prostatectomy tissue microarray, were used for comparison. FISH was carried out using ERG break-apart probes. Tumors were assessed for fusion by deletion (Edel) or split (Esplit), duplicated fusions and low-level copy number gain in normal ERG gene locus. Minute adenocarcinomas: Fusion was evaluable in 32/45 tumors (71%). Fifteen out of 32 (47%) tumors were positive for fusion. Six (19%) were of the Edel class and 7 (22%) were classified as combined Edel+Esplit. Non-minute adenocarcinomas (pT2): Fusion was identified in 20/30 tumors (67%). Four (13%) were of Edel class and 5 (17%) were combined Edel+Esplit. Duplicated fusions were encountered in 5 (16%) tumors. Non-minute adenocarcinomas (pT3): Fusion was identified in 19/33 (58%). Fusion was due to a deletion in 6 (18%) tumors. Seven tumors (21%) were classified as combined Edel+Esplit. One tumor showed Esplit alone. Duplicated fusions were encountered in 3 (9%) cases. The incidence of duplicated fusions was higher in non-minute adenocarcinomas (13 vs 0%; P=0.03). A trend for higher incidence of low-level copy number gain in normal ERG gene locus without fusion was noted in non-minute adenocarcinomas (10 vs 0%; P=0.07). We found a TMPRSS2–ERG fusion rate of 47% in minute adenocarcinomas. The latter is not significantly different from that of grade matched non-minute adenocarcinomas. The incidence of duplicated fusion was higher in non-minute adenocarcinomas. Our finding of comparable rate of TMPRSS2–ERG fusion in minute adenocarcinomas may argue against its value as a marker of aggressive prostate carcinoma phenotype.
Similar content being viewed by others
Main
A recurrent fusion between the androgen-regulated gene TMPRSS2 (21q22.3) and the ETS transcription factor family member ERG (21q22.2), initially described by Tomlins et al,1, 2 seems to be a common occurrence in prostate carcinoma. TMPRSS2–ERG fusion rates of 15–80% have been reported in prostatic adenocarcinoma by various groups,2, 3, 4, 5, 6, 7 making it the most common rearrangement identified in human cancer to date. The fusion can be the result of a small deletion on chromosome 21 (seen in approximately two thirds of cases) or can occur through a translocation.5 In either type of rearrangement, ERG is brought under the control of an androgen-regulated promoter and overexpression of the protein ensues. Studies addressing the clinical significance of TMPRSS2–ERG fusion as a prognostic marker have so far led to conflicting conclusions.8, 9, 10, 11, 12, 13 Some of the earlier studies have pointed to a subset of TMPRSS2–ERG fusions as being markers of aggressive outcome.8, 9, 10
Although the incidence of TMPRSS2–ERG fusion has been extensively studied in various prostatic adenocarcinoma cohorts,8, 9, 10, 11, 12, 13 to date, no study has assessed the incidence of TMPRSS2–ERG in the unique group of minute (minimal) adenocarcinomas of prostate. Minute prostatic adenocarcinoma is defined as a tumor fulfilling all the following criteria: (i) total volume of 0.5 cm3 or less; (ii) Gleason Score <7; (iii) tumor is organ confined on radical prostatectomy with no evidence of surgical margin, seminal vesicle or lymph node involvement.14 Defined as such, it is estimated that around 5% of all prostate adenocarcinoma undergoing radical prostatectomy represent minute prostatic adenocarcinomas. Such tumors are considered to be clinically ‘insignificant’ tumors lacking the virulence for significant morbidity or mortality.15, 16
The aim of this study was to assess the incidence of TMPRSS2–ERG fusion in a group of minute prostatic adenocarcinomas and to compare such incidence with that of a Gleason score-matched (<7) non-minute prostatic adenocarcinomas of stage pT2N0M0 or pT3N0M0.
Materials and methods
This study is approved by our Institutional Review Board.
Patient Cohort and Tissue Microarray Construction
Minute prostatic adenocarcinoma group
We retrieved all radical prostatectomy specimens for prostatectomies carried out at the Johns Hopkins Hospitals between January 2002 and June 2003, and diagnosed with prostatic adenocarcinoma tumors meeting the above criteria of minute prostatic adenocarcinomas. H&E sections and paraffin blocks were obtained and the diagnosis of minute prostatic adenocarcinomas was confirmed by three urologic pathologists involved in this study (GJN, RA and ML). A total of 45 consecutive minute prostatic adenocarcinoma radical prostatectomy specimens with available archival material were included for tissue microarray construction. In three patients, two separate minute prostatic adenocarcinoma foci were sampled in the tissue microarray. Tumor and paired benign tissue were represented by up to three 1-mm spots using the method previously described by Kononen et al.17
Non-minute prostatic adenocarcinoma group
Sixty-three consecutive radical prostatectomy specimens from a separate tissue microarray set constructed from 742 parent population-based PSA Era prostatectomies carried out at the Johns Hopkins hospital (1993–2000) were used as our non-minute prostatic adenocarcinoma group.13 All 63 tumors were of GS<7. They included 30 pT2 and 33 pT3 tumors.
Clinicopathological data
All pertinent clinicopathological data were retrieved from electronic medical records to include patient's age, ethnicity, preoperative PSA, percentages of tumor involvement at biopsies and detailed prostatectomy pathologic findings. The latter included prostate weight, tumor volume, tumor grade, stage and location of tumor.
Evaluation of TMPRSS2–ERG Fusion Status with Interphase ERG Break Apart FISH Assay
FISH analysis was carried out using dual-color interphase break-apart probes for the 5′ and 3′ regions of ERG gene. Briefly, 4 μm paraffin-embedded tissue microarray sections were baked at 56°C for 2 h then dewaxed and rehydrated using xylene and graded ethanol, respectively. Tissue microarray sections were pretreated using Paraffin Pretreatment Reagent Kit III (Abbott Molecular, IL). BAC FISH probes used were Spectrum Green d-UTP direct-labeled BAC RP11-95I21 for 5′ ERG, and Spectrum Orange d-UTP direct-labeled BAC RP11-476D17 for 3′ ERG (Nick transKit, Vysis, Abbott Park, IL). Tissue microarrays and BAC FISH probes were co-denatured at 94°C for 5 min and hybridized overnight at 37°C in a humid chamber (StatSpin ThermoBrite, IRIS, MA).
FISH interpretation was carried out by two urologic pathologists (RA and GJN). Tissue microarray sections were scored using a × 100 oil immersion lens on an Olympus BX-70 fluorescence microscope (Olympus, Center Valley, PA) equipped with appropriate filters. For photomicrographs, images were captured using a Nikon E400 fluorescence microscope equipped with a Nikon DXM1200 camera (Nikon Instruments, Melville, NY) and the SPOT Advanced digital imaging software (Diagnostic Instruments, Sterling Heights, MI). In each case, a minimum of 50 cells were scored for the presence/absence of TMPRSS2–ERG gene fusion through deletion or split. Digitally scanned adjacent H&E sections were available for side-by-side comparison with the FISH image to localize tumor cells. Gleason grade was confirmed for each tissue microarray spot. Paired benign prostatic epithelium was also scored as a negative control.
Each tissue microarray spot was analyzed for TMPRSS2–ERG fusion as previously described by Attard et al10 with the following minor modifications: (i) class negative for fusion (N): a nucleus with two pairs of juxtaposed red and green signals forming yellow signals, indicating the absence of ERG rearrangement. (ii) class ERG signal split (Esplit): a nucleus with one juxtaposed red–green signal pair of the non-rearranged ERG allele and additional separate single red and single green signal of rearranged ERG allele (break apart) reflecting a TMPRSS2–ERG fusion through split. (iii) class ERG deletion (Edel): a nucleus with one juxtaposed red–green signal pair for the non-rearranged allele and a single red signal of a rearranged allele, indicating deletion of the telomeric (green) ERG probe region (fusion through deletion). Any case with one of the above ERG signal abnormalities in ≥10% of the nuclei was scored as a fusion case and classified accordingly. Tumors with a subpopulation of cells with different types of fusions meeting the above cutoff were assigned more than one fusion class.
In addition, the presence of multiple copies of the particular TMPRSS2–ERG fusion as well as the presence of a low-level copy number gain of a normal ERG (>2 copies) was simultaneously assessed in all evaluated nuclei.
A tissue microarray spot was deemed technically inadequate for scoring if lack of diagnostic tissue, weak probe signal or presence of overlapping nuclei prevented accurate FISH assessment.
Statistical Analysis
Demographic, clinicopathological and TMPRSS2–ERG data were analyzed using the Stata 9.2 software package (StataCorp; college Station TX). Equality of population means among groups was tested using Kruskal–Wallis test for non-parametric and one-way analysis of variance by ranks.
Results
Patient Demographics and Clinical Findings
Patient demographics and clinical data are summarized in Tables 1 and 2. There was no significant difference in mean patient age between minute and non-minute prostatic adenocarcinoma patients. As expected, a higher preoperative serum PSA was present in non-minute prostatic adenocarcinoma patients (P=0.002), similarly, higher incidence of biochemical recurrence was encountered in non-minute prostatic adenocarcinoma patients (P=0.001).
TMPRSS2–ERG FISH Analysis
None of the examined paired, benign, prostate gland tissue spots from 43 minute prostatic adenocarcinoma cases (80 spots) and 63 non-minute prostatic adenocarcinomas showed the evidence of TMPRSS2–ERG fusion using our FISH assay.
Minute prostatic adenocarcinoma group
TMPRSS2–ERG fusion was evaluable by FISH in 32 of 45 (71%) samples represented on the tissue microarray.
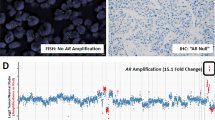
Fifteen (47%) tumors were positive for the TMPRSS2–ERG fusion (Figures 1 and 2; Table 3). Out of the minute prostatic adenocarcinoma tumors that were positive for fusion, 6 (19%) were of the Edel class and seven (22%) were classified as combined Edel+Esplit due to the presence of two subpopulations of cells showing the two fusion classes. None of our minute prostatic adenocarcinomas showed Esplit alone. Duplicated fusion (2Edel or 2Esplit) was not encountered in this group.
(a) Tissue microarray spot showing a focus of minute prostate adenocarcinoma (hematoxylin–eosin stain: × 200). (b and c) FISH break apart assay for TMPRSS2–ERG. TMPRSS2–ERG fusion through ERG split (Esplit), with one juxtaposed red–green (yellow) signal in each nucleus and the second pair of red and green signals split apart and separated spatially in different regions of the nucleus (original magnification: × 1000).
(a) Tissue microarray spot showing a focus of minute prostate adenocarcinoma (hematoxylin–eosin stain: × 100). (b and c) FISH break apart assay for TMPRSS2–ERG. TMPRSS2–ERG fusion through deletion (Edel), with one juxtaposed red–green (yellow) signal in each nucleus and absence of the second green signal (original magnification: × 1000).
Two minute prostatic adenocarcinomas (6%) showed low-level copy number gain of non-rearranged ERG allele associated with a single copy TMPRSS2–ERG fusion. Low-level copy number gain of a normal ERG without ERG fusion was not observed in any minute prostatic adenocarcinoma cases.
In two of the three minute prostatic adenocarcinomas cases containing more than one distinct focus of cancer on the radical prostatectomy specimens that were sampled on the tissue microarray, TMPRSS2–ERG fusion (Edel) was present in one, but not in the other, focus of prostatic adenocarcinoma.
Non-minute prostatic adenocarcinomas (pT2)
TMPRSS2–ERG fusion was identified in 20/30 (67%) pT2 non-minute prostatic adenocarcinomas. The fusion was due to a deletion in 4/30 (13%) cases. Five additional tumors (17%) were classified as combined Edel+Esplit because of the presence of two subpopulations of cells showing the two fusion classes. None of pT2 non-minute prostatic adenocarcinomas showed Esplit alone.
Duplicated fusion (2Edel or 2Esplit) was encountered in 5 (16%) cases in this group.
Six (20%) pT2 non-minute prostatic adenocarcinomas showed low-level copy number gain of non-rearranged ERG allele associated with a single copy TMPRSS2–ERG fusion. In addition, low-level copy number gain of non-rearranged ERG without ERG fusion was also observed in 3/30 (10%) of pT2 non-minute prostatic adenocarcinomas.
Non-minute prostatic adenocarcinomas (pT3)
TMPRSS2–ERG fusion was identified in 19/33 (58%) pT3 non-minute prostatic adenocarcinomas. The fusion was due to a deletion in 6/33 (18%) cases. Seven additional tumors (21%) were classified as combined Edel+Esplit because of the presence of two subpopulations of cells showing the two fusion classes. One pT3 non-minute prostatic adenocarcinomas showed Esplit alone.
Duplicated fusion (2Edel or 2Esplit) was encountered in three (9%) cases in this group.
Two (6%) pT3 non-minute prostatic adenocarcinomas showed low-level copy number gain of non-rearranged ERG allele associated with a single copy TMPRSS2–ERG fusion. In additional, low-level copy number gain of a normal ERG without ERG fusion was also observed in 3/33 (9%) of pT3 non-minute prostatic adenocarcinomas.
Comparison of TMPRSS2–ERG Fusion Incidence Between Minute Prostatic Adenocarcinomas and Non-Minute Prostatic Adenocarcinomas
Detailed comparative analysis of the different groups is shown in Table 3. Although the overall frequency of TMPRSS2–ERG fusion was slightly lower in minute prostatic adenocarcinomas compared with non-minute prostatic adenocarcinomas (47 vs 62%), the difference was not statistically significant (P=non-significant). The incidence of duplicated fusion was higher in non-minute prostatic adenocarcinoma group (13 vs 0%; P=0.03). In addition, a trend for higher incidence of low-level copy number gain of a normal ERG without fusion in non-minute prostatic adenocarcinomas (10 vs 0%; P=0.07) was noted. We observed no statistically significant difference between minute prostatic adenocarcinomas and non-minute prostatic adenocarcinoma cases in term of the incidence of class Esplit, Edel, combined Espli+Edel or the presence of low-level copy number gain of a normal ERG with fusion.
Similar results were obtained when the minute prostatic adenocarcinomas were compared to the subset of stage pT2 non-minute prostatic adenocarcinomas. TMPRSS2–ERG fusion incidence was slightly lower in minute prostatic adenocarcinomas cases (47 vs 67%), the difference was again not statistically significant (P=non-significant). The incidence of duplicated fusion was higher in the non-minute prostatic adenocarcinoma pT2 group (16 vs 0%; P=0.01). The trend for higher incidence of low-level copy number gain of a normal ERG without fusion remained in non-minute prostatic adenocarcinoma pT2 tumors (10 vs 0%; P=0.06). We observed no statistically significant difference between minute prostatic adenocarcinomas and non-minute prostatic adenocarcinoma pT2 cases in term of the incidence of the remaining fusion classes.
Relationship of Presence of Fusion and Fusion Class to Biochemical Recurrence
As expected, none of minute prostatic adenocarcinoma patients developed evidence of biochemical recurrence. In non-minute prostatic adenocarcinoma patients, no statistically significant correlation was detected between biochemical recurrence and the presence of fusion (P: non-significant). Similarly, we found no association between biochemical recurrence and fusion class, the presence of duplicated fusion nor the presence of low-level increased gene copy number of non-rearranged ERG allele (P=non-significant).
Discussion
Presently, an accurate prediction of the presence of minute prostatic adenocarcinoma in a prostatectomy specimen cannot be achieved preoperatively. Patients diagnosed with a single small focus of prostatic adenocarcinoma on needle biopsy, especially when the focus is less than one high-power field, are thought to be more likely to harbor a minute prostatic adenocarcinoma on radical prostatectomy.14 Given that minute prostatic adenocarcinomas are generally considered to be clinically ‘insignificant’ tumors,15, 16 the need for radical prostatectomy in such patients is frequently brought into question. Finding markers that will help better identify such subset of patients is of great interest. TMPRSS2–ERG fusion is a common genetic alteration in prostatic adenocarcinoma. In this study, we aimed at evaluating the incidence of this fusion in a unique set of minute prostatic adenocarcinoma specimens in comparison with non-minute prostatic adenocarcinomas to assess any potential role of the presence of TMPRSS2–ERG fusion, or type of fusion class, in differentiating the two groups of patients.
To date, with the exception of a rare study, most large cohort studies have found the incidence of TMRSS2–ERG rearrangement in non-minute prostatic adenocarcinoma tumors to be in the 40–60% range.2, 3, 5, 9, 12, 18 In our PSA Era cohort of Gleason 6 non-minute prostatic adenocarcinoma tumors, we found a 62% rearrangement rate similar to the rates reported in surgical cohort studies assessing ERG gene alterations by similar FISH break-apart assay.5
In this study, fusions in minute prostatic adenocarcinoma and non-minute prostatic adenocarcinoma tumors were more likely to be the result of deletion either homogeneously throughout a given tumor or in association with subpopulation of tumor cells harboring a split event. The preponderance of deletion events is in line with prior observations.5, 18, 19 Intronic loss of genomic DNA between ERG and TMPRSS2, on chromosome 21q22.2–3, seems to be the main mechanism of gene fusion.
Although, we observed a slightly lower TMPRSS2–ERG fusion rate of 47% in our minute prostatic adenocarcinomas, the difference was not statistically significant compared with non-minute prostatic adenocarcinoma groups. Our latter finding was not totally unexpected given the fact that the presence of fusion has been previously documented in up to 20% of high-grade PIN.4, 20 The occurrence of fusion at the prostatic adenocarcinoma precursor stage suggests that it is a relatively early pathogenic event in prostatic adenocarcinoma oncogenesis. In fact, our finding regarding a high incidence of fusion events in our minute prostatic adenocarcinoma cohort of presumably early prostatic tumors can be seen as additional indirect evidence in support of the early role of TMPRSS2–ERG fusion in prostatic adenocarcinoma pathogenesis.
Earlier studies have shown the presence of TMPRSS2–ERG rearrangement to be homogeneous in a given tumor focus,5 but heterogeneous in the context of multiple cancer foci within the same prostate.21 In this regard, we find our observation regarding incongruous fusion status in two of the three minute prostatic adenocarcinoma tumors to be intriguing and in support of earlier observations in larger volume, more advanced tumors. The variability of fusion status in separate minute prostatic adenocarcinoma tumor foci in the same radical prostatectomy specimen would support the previous suggestion by Clark et al22 that TMPRSS2–ERG gene fusions may be arising independently in different regions of a single prostate.
Our ERG gene copy number findings of a significantly higher rate of duplicated ERG fusions and a trend toward higher rate of low-level copy number gain of a normal ERG in non-minute prostatic adenocarcinomas compared with minute prostatic adenocarcinomas are in line with previously shown association between abnormalities in ploidy status and prostatic adenocarcinoma tumor progression.23, 24, 25 Our low-level, increased ERG gene copy number suggests that gain of ERG copy number is potentially acquired during tumor progression.
Although earlier studies have linked the presence of TMPRSS2–ERG fusion, or the presence of a subset of TMPRSS2–ERG fusion class, with a more aggressive prostatic adenocarcinoma biological behavior,5, 8, 9, 11, 26 recent large cohort studies failed to reveal a prognostic role for the presence of fusion.12, 27, 28 Our finding of a high incidence of TMPRSS2–ERG fusions in minute prostatic adenocarcinomas that is comparable with that of non-minute prostatic adenocarcinomas would further lend support to a lack of association between the presence of fusion and aggressive behavior given the established lack of clinical significance of minute prostatic adenocarcinoma tumors.
In summary, this is the first study documenting the presence of ERG rearrangement in minute prostatic adenocarcinomas with a rate comparable with that of a more advanced stage, clinically significant tumors. Our findings can be seen as a indirect evidence supporting ERG fusion occurrence as an early event in prostate cancer pathogenesis. Findings of this study could also be interpreted as an additional indirect evidence supporting the lack of association between TMPRSS2–ERG and aggressive outcome, bringing into question its value as a marker of aggressive prostatic adenocarcinoma phenotype.
References
Tomlins SA, Rhodes DR, Perner S, et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 2005;310:644–648.
Mehra R, Tomlins SA, Shen R, et al. Comprehensive assessment of TMPRSS2 and ETS family gene aberrations in clinically localized prostate cancer. Mod Pathol 2007;20:538–544.
Wang J, Cai Y, Yu W, et al. Pleiotropic biological activities of alternatively spliced TMPRSS2–ERG fusion gene transcripts. Cancer Res 2008;68:8516–8524.
Cerveira N, Ribeiro FR, Peixoto A, et al. TMPRSS2–ERG gene fusion causing ERG overexpression precedes chromosome copy number changes in prostate carcinomas and paired HGPIN lesions. Neoplasia 2006;8:826–832.
Perner S, Mosquera JM, Demichelis F, et al. TMPRSS2–ERG fusion prostate cancer: an early molecular event associated with invasion. Am J Surg Pathol 2007;31:882–888.
Rajput AB, Miller MA, De Luca A, et al. Frequency of the TMPRSS2–ERG gene fusion is increased in moderate to poorly differentiated prostate cancers. J Clin Pathol 2007;60:1238–1243.
Lapointe J, Kim YH, Miller MA, et al. A variant TMPRSS2 isoform and ERG fusion product in prostate cancer with implications for molecular diagnosis. Mod Pathol 2007;20:467–473.
Demichelis F, Fall K, Perner S, et al. TMPRSS2–ERG gene fusion associated with lethal prostate cancer in a watchful waiting cohort. Oncogene 2007;26:4596–4599.
Nam RK, Sugar L, Wang Z, et al. Expression of TMPRSS2–ERG gene fusion in prostate cancer cells is an important prognostic factor for cancer progression. Cancer Biol Ther 2007;6:40–45.
Attard G, Clark J, Ambroisine L, et al., Transatlantic Prostate Group. Duplication of the fusion of TMPRSS2 to ERG sequences identifies fatal human prostate cancer. Oncogene 2008;27:253–263.
Cheville JC, Karnes RJ, Therneau TM, et al. Gene panel model predictive of outcome in men at high-risk of systemic progression and death from prostate cancer after radical retropubic prostatectomy. J Clin Oncol 2008;26:3930–3936.
Gopalan A, Leversha MA, Satagopan JM, et al. TMPRSS2–ERG gene fusion is not associated with outcome in patients treated by prostatectomy. Cancer Res 2009;69:1400–1406.
Lotan TL, Toubaji A, Albadine R, et al. TMPRSS2–ERG gene fusions are infrequent in prostatic ductal adenocarcinomas. Mod Pathol 2009;22:359–365.
Truskinovsky AM, Sanderson H, Epstein JI . Characterization of minute adenocarcinomas of prostate at radical prostatectomy. Urology 2004;64:733–737.
Furusato B, Rosner IL, Osborn D, et al. Do patients with low volume prostate cancer have prostate specific antigen recurrence following radical prostatectomy? J Clin Pathol 2008;61:1038–1040.
Harnden P, Naylor B, Shelley MD, et al. The clinical management of patients with a small volume of prostatic cancer on biopsy: What are the risks of progression? A systematic review and meta-analysis. Cancer 2008;112:971–981.
Kononen J, Bubendorf L, Kallioniemi A, et al. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 1998;4:844–847.
Tu JJ, Rohan S, Kao J, et al. Gene fusions between TMPRSS2 and ETS family genes in prostate cancer: frequency and transcript variant analysis by RT–PCR and FISH on paraffin-embedded tissues. Mod Pathol 2007;20:921–928.
Yoshimoto M, Joshua AM, Chilton-Macneill S, et al. Three-color FISH analysis of TMPRSS2–ERG fusions in prostate cancer indicates that genomic microdeletion of chromosome 21 is associated with rearrangement. Neoplasia 2006;8:465–469.
Mosquera JM, Perner S, Genega EM, et al. Characterization of TMPRSS2–ERG fusion high-grade prostatic intraepithelial neoplasia and potential clinical implications. Clin Cancer Res 2008;14:3380–3385.
Furusato B, Gao CL, Ravindranath L, et al. Mapping of TMPRSS2–ERG fusions in the context of multi-focal prostate cancer. Mod Pathol 2008;21:67–75.
Clark J, Merson S, Jhavar S, et al. Diversity of TMPRSS2–ERG fusion transcripts in the human prostate. Oncogene 2007;26:2667–2673.
Epstein JI, Amin M, Boccon-Gibod L, et al. Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand J Urol Nephrol Suppl 2005;216:34–63.
Brown JA, Slezak JM, Lieber MM, et al. Fluorescence in situ hybridization aneuploidy as a predictor of clinical disease recurrence and prostate-specific antigen level 3 years after radical prostatectomy. Mayo Clin Proc 1999;74:1214–1220.
Lau WK, Blute ML, Bostwick DG, et al. Prognostic factors for survival of patients with pathological Gleason score 7 prostate cancer: differences in outcome between primary Gleason grades 3 and 4. J Urol 2001;166:1692–1697.
Attard G, Clark J, Ambroisine L, et al., Transatlantic Prostate Group. Duplication of the fusion of TMPRSS2 to ERG sequences identifies fatal human prostate cancer. Oncogene 2008;27:253–263.
Saramaki OR, Harjula AE, Martikainen PM, et al. TMPRSS2:ERG fusion identifies a subgroup of prostate cancers with a favorable prognosis. Clin Cancer Res 2008;14:3395–3400.
Toubaji A, Albadine R, Meeker AK, et al. Chromosome 21 copy number but not TMPRSS2–ERG fusion predicts outcome in prostatic adenocarcinoma: a large case–control radical prostatectomy cohort analysis. Mod Pathol 2009;22 (suppl 1):189A.
Acknowledgements
This study was supported, in part, by grants from the Patrick C Walsh Prostate Cancer Foundation, David Koch Prostate Cancer Foundation and by the Johns Hopkins University SPORE in Prostate Cancer NCI–NIH grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the 2009 United States and Canadian (USCAP) annual meeting in Boston, USA.
Disclosure/conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Albadine, R., Latour, M., Toubaji, A. et al. TMPRSS2–ERG gene fusion status in minute (minimal) prostatic adenocarcinoma. Mod Pathol 22, 1415–1422 (2009). https://doi.org/10.1038/modpathol.2009.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2009.121
Keywords
This article is cited by
-
Assessing the order of critical alterations in prostate cancer development and progression by IHC: further evidence that PTEN loss occurs subsequent to ERG gene fusion
Prostate Cancer and Prostatic Diseases (2013)
-
ERG immunohistochemistry is not predictive for PSA recurrence, local recurrence or overall survival after radical prostatectomy for prostate cancer
Modern Pathology (2012)
-
ERG–TMPRSS2 rearrangement is shared by concurrent prostatic adenocarcinoma and prostatic small cell carcinoma and absent in small cell carcinoma of the urinary bladder: evidence supporting monoclonal origin
Modern Pathology (2011)
-
Antibody EPR3864 is specific for ERG genomic fusions in prostate cancer: implications for pathological practice
Modern Pathology (2011)
-
Increased gene copy number of ERG on chromosome 21 but not TMPRSS2–ERG fusion predicts outcome in prostatic adenocarcinomas
Modern Pathology (2011)