Abstract
Somatic mutations of mitochondrial DNA (mtDNA) are associated with various types of human cancer. To elucidate their role in gastric carcinogenesis, we analyzed mutations in the displacement loop region of mtDNA in 24 paraffin-embedded gastric intraepithelial neoplasias (formerly dysplasia) from a high gastric cancer risk area in northern Italy. Helicobacter pylori infection was assessed by histological examination (Giemsa staining). Gastritis was classified according to the guidelines of the Updated Sydney System. The mtDNA displacement loop region was amplified and sequenced from gastric intraepithelial neoplasia samples and adjacent non-neoplastic gastric mucosa. The gastric intraepithelial neoplasias were divided into two groups by their association with H. pylori gastritis. Group A with lesions arising on a background of H. pylori-positive gastritis contained 7 patients, and group B with lesions associated with H. pylori-negative gastritis contained 17 patients. Group A had a larger proportion of high-grade lesions than group B and showed a foveolar phenotype (type II dysplasia). Group B had a larger proportion of cases with mtDNA displacement loop region mutations than group A (P=0.004, Fisher's exact test) and exhibited an intestinal phenotype. No evidence of heteroplasmic variants in the mtDNA displacement loop, suggestive of mutations, was detected in gastric biopsies from 25 H. pylori-negative subjects and 60 cancer-unaffected H. pylori-positive patients. These results provide further evidence for the morphologic and mtDNA biomolecular differences of gastric intraepithelial neoplasias, and suggest the existence of two distinct pathways to gastric cancer—corpus-dominant H. pylori gastritis and the atrophy–metaplasia pathway.
Similar content being viewed by others
Main
As in all eukaryotes, the genetic information of human cells is separated into two interdependent genomes. First, the nucleus contains the diploid genome of approximately six billion base pairs (bp), a small fraction of which codes for 35–70 000 genes.1 Second, within each cell, there are up to 1000 mitochondria, each harboring a few copies of compact double-stranded circular mitochondrial DNA (mtDNA). The human mtDNA molecule spans 16 569 bp and contains 37 genes, of which 13 encode enzymes of the oxidative phosphorylation system, 22 encode tRNAs, and 2 encode the 2 types of rRNAs.1, 2 Based on their guanine (G) content, the two complementary strands of mtDNA are designated heavy (H) and light (L) strands. The guanine-rich H-strand encodes 28 of the 37 genes, with the remaining genes encoded by the L-strand.2 A non-coding control region spanning nucleotide positions (np) 16024 to np 576 contains three well-characterized hypervariable regions (HVRI: np 16024 to np 16365; HVRII: np 73 to np 340; and HVRIII: np 438 to np 576) and includes the origin of replication of one strand, a displacement loop (D-loop) region, and both origins of transcription. mtDNA replication and transcription are linked because RNA transcripts initiated at the L-strand promoter function as primers for mtDNA replication at the H-strand origin.3, 4, 5, 6, 7
mtDNA is believed to be more susceptible to DNA damage than nuclear DNA and consequently acquires mutations at a higher rate. Several possible factors may account for enhanced susceptibility to damage, including exposure to high levels of reactive oxygen species (ROS) during oxidative phosphorylation, lack of protective histones, and deficient DNA repair.8 It is as yet unclear how an mtDNA variant genome expands and replaces the wild-type mtDNA. Sometimes, more than one mtDNA variants occur within a single cell, tissue, or organism, a condition termed heteroplasmy, as opposed to homoplasmy, which indicates the presence of one single mtDNA species.9
mtDNA is frequently mutated in different types of cancer, including 16–51% of gastric carcinomas.10, 11, 12, 13, 14, 15, 16, 17, 18, 19 mtDNA mutations may be associated with altered expression and activity of respiratory chain subunits and glycolytic enzymes, decreased oxidation of NADH-linked substrates, and altered mtDNA content.11 This suggests a potential role of mtDNA in carcinogenesis. Although alterations may occur throughout the mtDNA sequence, a number of studies suggest that the D-loop, the regulatory region, is a hot spot for mutations that might alter the rate of DNA replication by modifying the binding affinity of important trans-acting factors.20, 21
Gastric cancers have been classified histologically into intestinal and diffuse types based on the glandular formations described by Laurèn,22 and these two types correspond to the differentiated and undifferentiated types described by Nakamura et al.23 Recently, a new classification of gastric carcinomas based on mucin expression was proposed.24, 25 Gastric carcinomas were classified as of gastric or intestinal phenotype on the basis of mucin expression by surface mucous cells, glandular mucous cells, and intestinal columnar and goblet cells. The differentiated (intestinal)-type tumor was thought to display a predominantly intestinal phenotype because it is preceded by a precancerous stage characterized by the sequential steps of atrophic gastritis, intestinal metaplasia, intraepithelial neoplasia (GIN) (formerly dysplasia), and intramucosal carcinoma.25, 26 However, it has become clear through mucin histochemical or immunohistochemical studies that some differentiated (intestinal)-type adenocarcinomas arise from gastric mucosa without intestinal metaplasia and display gastric phenotypes.24 Parallelly, GIN has been recently classified as intestinal (or adenomatous, because it resembles colonic adenoma, or type I), the most frequent type, or the rarer foveolar (or gastric type or type II).25, 26, 27, 28, 29, 30 GINs of intestinal phenotype are formed by dysplastic intestinal-type epithelium that comprises a mixture of goblet cells with intestinal mucin, whereas GINs of foveolar phenotype are entirely formed by dysplastic foveolar-type epithelium.25, 26, 27, 28, 29, 30
Helicobacter pylori infection causes chronic gastritis and is associated with the development of peptic ulcer disease, gastric carcinoma, and MALT lymphoma.31, 32 Investigations of gastritis in patients with advanced and early carcinomas and in relatives of gastric carcinoma patients have shown that these subjects often have a corpus-dominant gastritis.33, 34, 35, 36 In contrast, patients with H. pylori gastritis and duodenal ulcer, who almost never develop gastric cancer, have an antrum-dominant gastritis.33, 34, 35, 36
Specimens from patients with advanced cancer are not ideal for histogenetic studies, as tumor growth may obliterate areas that could be relevant for classification (eg, intestinal metaplasia, corpus-predominant gastritis, and gastric atrophy).31 Therefore, to obtain information on the histogenesis of gastric carcinoma, we studied the phenotypes of 24 GINs and evaluated the features of gastritis using the Updated Sydney System.37 Mutations in the D-loop region of mtDNA were also analyzed and their implications for gastric carcinogenesis discussed.
Materials and methods
Patients and Lesions
Pathology files were searched for patients who underwent gastric resection in which ‘adenoma’ or ‘dysplasia’ or ‘borderline lesion’ was reported in the diagnosis. Gastric biopsies from 25 H. pylori-negative normal subjects and 60 cancer-unaffected H. pylori-positive patients were also studied. In these cases, four mucosal biopsies were obtained from each patient: two from the antrum and two from the corpus. All cases were retrospectively identified in Cremona, a high-risk area for gastric cancer in northern Italy, between 1980 and 2000. Information from chart reviews and clinicians was obtained to determine demographic data and tumor sites. To our knowledge, these patients did not receive eradication therapy before gastrectomy.
Histopathological Assessment of GIN
By definition, the histological diagnosis of GIN was restricted to the cases that showed both altered glandular architecture and abnormalities in cytology and differentiation, but it lacked any (even doubtful) infiltrating feature. GINs synchronous to advanced gastric carcinomas were excluded from this study. In addition, several cases that showed infiltrating adenocarcinoma adjacent to dysplastic epithelium were excluded because it was not possible to distinguish histologically between GIN and intraepithelial growth of adenocarcinoma. Finally, seven cases were excluded because the slides and blocks could not be retrieved from the files.
GIN was categorized as either high or low grade according to both the Vienna38 and WHO39 classifications. Briefly, low-grade lesions showed elongated, hyperchromatic, and crowded nuclei with mild pseudostratification. Cribriform architecture, marked glandular crowding, full-thickness nuclear stratification, and/or severe cytologic atypia were criteria for high-grade GIN. GINs were also classified as intestinal type (formed by intestinal-type epithelium containing goblet and Paneth cells) or foveolar type (lined entirely by gastric mucous cells showing vesicular nuclei with increased nuclear/cytoplasmic ratio, prominent nucleoli, nuclear stratification, and numerous mitoses).30 Usually, the histological diagnosis of GIN does not include the so-called tubule neck dysplasia, which is believed to represent the precancerous lesion of diffuse-type gastric cancer.29 This lesion is not readily recognizable and constitutes a controversial entity.29 Thus, the histological diagnosis of GIN was restricted to conventional cases showing intestinal or foveolar phenotype.29, 30 The final study population therefore consisted of 24 GINs (from 24 patients).
Assessment of Gastritis and H. pylori Infection
Longitudinal sections for histology were systematically obtained from the primary gastric cancer specimen and from the cancer-unaffected gastric mucosa of the antrum and corpus along the lesser curvature and the anterior or posterior wall along the greater curvature. The extensive sampling protocol allowed characterization of the gastritis phenotype, also decreasing the likelihood of false-negative H. pylori cases. We further examined non-neoplastic mucosa adjacent to GIN, defined as GIN periphery. Surgically resected material for histology was fixed in 10% formalin and embedded in paraffin. Four-micrometer sections were stained with hematoxylin–eosin for histological examination and with Giemsa stain for H. pylori identification under high-power view (× 10 ocular and × 40 objective). Gastritis was analyzed in accordance with the Updated Sydney System,37 with the exception of H. pylori density, and was simply noted as present or absent. In particular, we evaluated medians of gastritis score on a scale from 0 to 3 for the following four items: (1) neutrophil activity; (2) degree of chronic inflammation; (3) degree of glandular atrophy; and (4) degree of intestinal metaplasia.37 Acute gastritis was further subclassified into acute epithelial and interstitial gastritis. The former, that is, acute foveolitis, was defined as present when at least one of the following three histopathological criteria were fulfilled: (1) an aggregate of more than 5 neutrophils within a pit; (2) more than 10 neutrophils infiltrating a pit circumferentially; and/or (3) an inflammatory exudate with more than 5 neutrophils in the lumen.40 Intestinal metaplasia was evaluated by alcian blue–PAS stain.
In three cases of GIN, gastric mucosa specimens were also obtained in the operating room for immediate fixation in 3% phosphate-buffered glutaraldehyde (pH 7.4) and post-fixed in 1% osmium tetroxide. Semi-thin araldite-embedded sections were stained with Giemsa's reagent for fine analysis.
Grouping of Lesions by H. pylori Infection
GINs were divided into two groups by their association with H. pylori gastritis. Group A with lesions arising in a background of H. pylori-positive gastritis contained 7 patients, and group B with lesions associated with H. pylori-negative gastritis contained 17 patients.
Analysis of the mtDNA D-Loop
mtDNA was extracted from 24 samples of paraffin-embedded GIN and adjacent non-neoplastic gastric tissue containing normal-appearing mucosa and/or focal areas of intestinal metaplasia. Furthermore, to verify the occurrence of heteroplasmies in normal gastric mucosa or due to the possible mutagenic role of H. pylori infection and/or inflammatory processes, mtDNA was extracted from paraffin-embedded gastric biopsies from 25 H. pylori-negative normal subjects and 60 cancer-unaffected H. pylori-positive gastritis patients of the same geographic area. Three to five 10-μm-thick sections were deparaffinized and manually microdissected under a dissecting microscope to separate neoplastic from non-neoplastic tissue using a hematoxylin- and eosin-stained step section as a guide. Total DNA was extracted using the QIAamp Tissue kit (Qiagen, Hilden, Germany) with standard protocols. Over 1200 bp of mtDNA, including the D-loop region, were amplified by nested PCR using primers L15990-H617. Four overlapped nested PCRs were performed using primers L15990-H16434, L16431-H162, L039-H407, and L361-H617 (Table 1). The total volume of the external PCR mixtures was 20 μl, including 1 μl of the primers L15990-H617 (20 pmol/μl), 2 μl of 10 × PCR buffer, 2 μl of dNTPs (2 nmol/l), 0.3 μl of Taq polymerase (5 U/μl) (Eurotaq; Euroclone Life Sciences Division, UK), and 100 ng of extracted DNA. PCRs were carried out using a GeneAmp PCR System 2700 (Applied Biosystems, CA, USA). PCR conditions included initial denaturation at 94°C for 5 min followed by 30 cycles of 94°C for 30 s, 57°C for 45 s, and 72°C for 30 s. Final extension was at 72°C for 7 min. The total volume of the internal PCR mixture was 40 μl, including 1 μl of each primer (20 pmol/μl), 4 μl of 10 × PCR buffer, 4 μl of dNTPs (2 nmol/l), 0.3 μl of Taq polymerase (5 U/μl) (Eurotaq; Euroclone Life Sciences Division), and 4 μl of the external PCR product. PCR conditions for all nested segments were as for external PCR, except for annealing temperature and number of cycles, which were 58°C and 20, respectively. Amplified fragments were visualized after electrophoresis on ethidium bromide-stained 2.0% agarose gels.
PCR products were purified with an instant PCR product purification kit (Millipore Corporation, MA, USA) and directly sequenced using the ABI-PRISM Big Dye™ Terminator version 3.0 Cycle Sequencing Ready Reaction kit (Applied Biosystems). Sequencing products were purified using DyeEx Spin kits (Qiagen) and visualized on an ABI-PRISM 310 Genetic Analyzer (Applied Biosystems).
Taking the mtDNA D-loop from the Anderson sequence2 as reference, a comparison was made between the sequences of GINs and those of adjacent non-neoplastic tissue. When the mtDNA D-loop sequence from a GIN sample differed from that obtained from a matched non-neoplastic gastric tissue, the alteration was regarded as a somatic mutation. Heteroplasmies in the mtDNA sequences amplified from gastric biopsies of 60 cancer-unaffected H. pylori-positive gastritis patients and 25 H. pylori-negative normal subjects were also regarded as evidence of somatic mtDNA mutations. The obtained mtDNA sequences were compared to those in the mtDNA databank (http://www.mitomap.org/). Mutations were always independently confirmed on replicate DNA samples from the same case and using forward and reverse primers for sequencing.
Statistical Analysis
Statistical analysis was performed using STATA software (version 8.0; STATA Corporation, College Station, TX, USA). For categorical data, the two groups were compared with the use of the Fisher exact test. P<0.05 indicated statistical significance.
Results
This study included 12 solitary GINs, 8 GINs synchronous to early gastric carcinomas, and 4 GINs associated with gastric ulcers, all from surgical resection specimens. The main clinicopathologic findings of the 24 patients with GIN are summarized in Table 2. The series of GIN cases included 17 male and 7 female patients, with a median age of 70 years (range: 50–83 years). Eleven of the 24 GINs were situated in the antrum and 13 in the body. No patient had familial adenomatous polyposis.
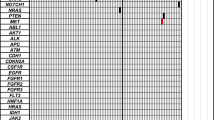
After nucleotide sequencing of the mtDNA D-loop, we detected nucleotide changes in GIN cases by comparison with the sequence from the adjacent non-neoplastic gastric tissue. The nucleotide variants were compared to those in the mtDNA databank (http://www.mitomap.org/) to verify those already described as tumor-associated mutations. We found that 15/24 (62%) GINs harbored mtDNA D-loop variants not detectable in adjacent non-neoplastic mucosa (Table 3). The variants manifested in 14/15 cases as heteroplasmies, being associated with the sequence present in matched gastric mucosa. The absence of such mutations in the adjacent mucosa was also confirmed in the cases in which focal areas of intestinal metaplasia were histologically detected in the adjacent non-neoplastic mucosa. No evidence of heteroplasmic mtDNA sequence variants was found in the biopsy specimens of the 25 H. pylori-negative subjects and of the 60 cancer-unaffected H. pylori-positive gastritis patients.
The mtDNA D-loop mutations detected in GINs included a G>A transition at np 16004; an A>C transversion at np 16013; a T>G transversion at np 16045; a C>T transition at np 16380; a C>T transition at np 16495 (two cases); an A>G transition at np 16510; an A>G transition at np 16515; a T>G transversion at np 10; a 1-bp insertion at np 12 (12.1 insA); an A>G transition at np 13; a C>G transversion at np 552; a C>G transversion at np 572; a T>G transversion at np 579; and a previously described C>T transition at np 559. Notably, 6/15 mutations (40%) were transversions. Only the A>C mutation at np 16013 was homoplasmic. Mutations were dispersed across the D-loop region, with no evidence of hot spots, except for the heteroplasmic transition at np 16495, detected in two cases.
The main clinicopathologic findings of groups A and B are summarized in Table 4. There were no significant differences between the two groups in age, sex or gastric location.
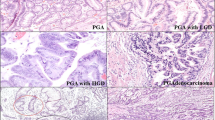
In the seven patients with H. pylori infection (group A), GINs showed foveolar phenotype (Figures 1 and 2) and presented as high-grade lesions (P=0.004). By contrast, in the 17 H. pylori-negative cases (group B), GINs presented as low-grade lesions (P=0.004), resembled colonic adenomas, and exhibited an intestinal phenotype (Figure 3). The D-loop mutations were significantly associated with group B (P=0.004). Four GINs that were associated with gastric ulcer occurred in atrophic/metaplastic mucosa (group B) (Table 2).
Group A GIN. (a) Foci of high-grade intraepithelial neoplasia with gastric phenotype. A prominent lymphoid follicle with germinal center is present in the deep mucosa. H&E, × 100. (b) Higher magnification of panel a. High-grade GIN is characterized by cribriform architecture, marked glandular crowding, full-thickness nuclear stratification, and open nuclei with prominent nucleoli. Note the intraglandular necrotic debris and/or neutrophils in areas of GIN. H&E, × 800.
Group A patients. GIN periphery. (a) Neutrophil aggregates infiltrating the mucous neck epithelium circumferentially. Bizarre mitotic figure is present in the neck region. Semi-thin section: Giemsa stain, × 800. (b) Aggregates of more than five neutrophils within the mucous neck epithelium. H&E, × 200.
The histology of GIN periphery is compared in Table 5. Grades for neutrophilic activity were more advanced in group A than in group B patients (P=0.04). In particular, acute foveolitis was more frequently present in group A (P=0.01). Representative photomicrographs of acute foveolitis at the GIN periphery are shown in Figure 2. Grades for chronic inflammatory infiltrate and glandular atrophy were not different between the two groups. However, the scores for intestinal metaplasia for antral and corporal mucosa tended to be higher in group B than in group A patients.
As an extended gastric resection was performed in our GIN cases, we could assess both corporal and antral mucosa in these cases. The comparison of the background mucosa of the cases is shown in Table 6. The score for neutrophil infiltration tended to be higher in group A than in group B (P=0.04). In addition, acute foveolitis in the antrum (P<0.01) or corpus (P<0.001) was more frequently present in group A than in group B (Figure 2). These data suggest the diagnosis of pan-gastritis (corpus-dominant gastritis) in group A patients. The degree of chronic inflammatory infiltrates, atrophy, and intestinal metaplasia was not different between the two groups at any sites of the stomach.
Discussion
Our data show that the GIN groups A and B are characterized by morphologic differences. Group A GINs presented as high-degree lesions (P=0.004) and were characterized by gastric phenotype (type II dysplasia).27, 28, 29 Group B GINs showed intestinal phenotype and presented mainly as low-grade lesions (P<0.004).
H. pylori was not morphologically detectable in group B patients. Furthermore, H. pylori was not found in metaplastic gastric mucosa, where inflammatory changes diminish. Therefore, it is possible that the high incidence of atrophic gastritis in group B might reflect a ‘burned out’ mucosa as a response to long-lasting severe H. pylori gastritis.41 Instead, group A patients did not reach complete atrophic gastritis before surgery, and showed an active corpus-dominant gastritis (so-called gastritis of the carcinoma phenotype).33, 34, 35, 36, 41 On the other hand, H. pylori gastritis is characterized by acute foveolitis of the proliferative zone, which is found in any stage of gastritis as long as infection persists. Because acute foveolitis targets specifically the proliferative zone of pits, the proliferating epithelial cells are under severe and persistent mutagenic pressure.26 Thus, it is possible that the histogenesis of GINs in group A patients is related to active H. pylori gastritis, as also suggested by the high incidence of acute foveolitis in the antral and corporal mucosa.
Our results indicate that 15 (62.5%) of the 24 tested GINs exhibit somatic point mutations in the mtDNA D-loop region, mostly present as heteroplasmies, probably due to the presence of stromal and inflammatory cells carrying the wild-type mtDNA D-loop sequence. The tumor-associated variants were not found in matched adjacent non-neoplastic gastric tissue and most likely represent somatic mutations associated with GIN development.42 Furthermore, the association between mutations and cancer is strengthened by the fact that no heteroplasmic mtDNA sequence variants were found in biopsy specimens of H. pylori-negative subjects and of H. pylori-positive cancer-unaffected patients from the same high-risk area. However, as our study was retrospective and was performed only in paraffin-embedded gastric tissues, it is possible that the homoplasmic somatic mutations present in gastric tissues independently of tumor development, which would have been highlighted while analyzing DNA from blood samples, escaped detection.
A significant fraction of the detected mtDNA mutations consisted of transversions, which could be related to alkyl adducts or oxidative damage.42 ROS are produced as part of the inflammatory reaction stimulated by H. pylori.43 However, we were unable to find any relationship between H. pylori-positive GINs and mtDNA mutations. On the other hand, similar mtDNA alterations have been observed in colorectal carcinoma,44, 45 which seems to develop irrespective of H. pylori infection. Thus, our findings would exclude the responsibility of H. pylori-mediated damage in the induction of the observed mtDNA transversions.
Instead, we found a significative correlation between group B GINs and mtDNA D-loop mutations (P=0.004). Group B lesions would therefore appear as distinct neoplasms in which mtDNA somatic mutations could play a role. The detected mutations target the D-loop, a structurally and functionally important region that, although non-coding, is responsible for the regulation of mtDNA replication and transcription. Although the significance of mutations in the D-loop region has not yet been elucidated and some authors hypothesized that they may simply be markers of clonal growth, rather than true functional alterations,46, 47 such mutations could affect mtDNA function and mitochondrial energy supply, enhancing the production of ROS, which could contribute to genetic injury, mutagenesis, and cancer.11, 19, 20, 48, 49, 50, 51, 52, 53, 54 The inverse association between group A GINs and mtDNA mutations must be interpreted with caution because we cannot rule out the possibility that the dense inflammatory cellular infiltrate associated with H. pylori infection might cause false-negative sequencing results by diluting mtDNA sequences originating from cancer cells.
The current study provides additional evidence highlighting the morphologic and biomolecular differences of GINs. The two GIN groups proposed according to the histological assessment of H. pylori infection (present/absent) have a significant correlation with some of the additional parameters studied, namely grade of dysplasia, foveolar/intestinal phenotype, acute foveolitis, and mtDNA D-loop mutations. Furthermore, our data suggest the presence of at least two histogenetic pathways of gastric carcinoma. To a certain extent, this parallels the situation in the large intestine where alternative route exists.55 The first pathway corresponds to the classic sequence of atrophy–metaplasia–GIN–carcinoma with intestinal phenotype.14 The second is strictly associated with acute foveolitis and corresponds to the alternative sequence hypothesis of corpus-dominant gastritis—foveolar-type GIN—carcinoma with gastric phenotype, in which the relationship between inflammation and cancer has been recently developed.15, 16, 17, 18
References
Hasegawa M, Horai S . Time of the deepest root for polymorphism in human mitochondrial DNA. J Mol Evol 1991;32:37–42.
Anderson S, Bankier AT, Barrell BG, et al. Sequence and organization of the human mitochondrial genome. Nature 1981;290:457–465.
Clayton DA . Replication of animal mitochondrial DNA. Cell 1982;28:693–705.
Clayton DA . Transcription of the mammalian mitochondrial genome. Annu Rev Biochem 1984;53:573–594.
Attardi G, Chomyn A, King MP, et al. Regulation of mitochondrial gene expression in mammalian cells. Biochem Soc Trans 1989;18:509–513.
Chang DD, Clayton DA . Precise identification of individual promoters for transcription of each strand of human mitochondrial DNA. Cell 1984;36:635–643.
Bogenhagen DF, Applegate EF, Yoza BK . Identification of promoter for transcription of the heavy strand of human mtDNA: in vitro transcription and deletion mutagenesis. Cell 1984;36:1105–1113.
Croteau DL, Bohr VA . Repair of oxidative damage to nuclear and mitochondrial DNA in mammalian cells. Proc Natl Acad Sci USA 1997;272:25409–25412.
Lightowlers RN, Chinnery PF, Turnbull DM, et al. Mammalian mitochondrial genetics: heredity, heteroplasmy and disease. Trends Genet 1997;13:450–455.
Carew JS, Huang P . Mitochondrial defects in cancer. Mol Cancer 2002;1:9–21.
Mambo E, Chatterjee A, Xing M, et al. Tumor-specific changes in mtDNA content in human cancer. Int J Cancer 2005;116:920–924.
Tamura G, Nishizuka S, Maesawa C, et al. Mutations in mitochondrial control region DNA in gastric tumours of Japanese patients. Eur J Cancer 1999;35:316–319.
Habano W, Sugai T, Nakamura SI, et al. Microsatellite instability and mutation of mitochondrial and nuclear DNA in gastric carcinoma. Gastroenterology 2000;118:835–841.
Maximo V, Soares P, Seruca R, et al. Microsatellite instability, mitochondrial DNA large deletions, and mitochondrial DNA mutations in gastric carcinoma. Genes Chromosomes Cancer 2001;32:136–143.
Hiyama T, Tanaka S, Shima H, et al. Somatic mutation of mitochondrial DNA in Helicobacter pylori-associated chronic gastritis in patients with and without gastric cancer. Int J Mol Med 2003;12:169–174.
Ling X-L, Fang D-C, Wang R-Q, et al. Mitochondrial microsatellite instability in gastric cancer and its precancerous lesions. World J Gastroenterol 2004;10:800–803.
Wu C-W, Yin P-H, Hung W-Y, et al. Mitochondrial DNA mutations and mitochondrial DNA depletion in gastric cancer. Genes Chromosomes Cancer 2005;44:19–28.
Zhao Y-B, Yang H-Y, Zhang X-W, et al. Mutation in the D-loop region of mitochondrial DNA in gastric cancer and its significance. World J Gastroenterol 2005;11:3304–3306.
Lee H-C, Yin P-H, Lin J-C, et al. Mitochondrial genome instability and mtDNA depletion in human cancers. Ann N Y Acad Sci 2005;1042:109–122.
Wang Y, Liu VWS, Ngan HYS, et al. Frequent occurrence of mitochondrial microsatellite instability in the D-loop region of human cancers. Ann N Y Acad Sci 2005;1042:123–129.
Fliss MS, Usadel H, Otá V, et al. Facile detection of mitochondrial DNA mutations in tumors and body fluids. Science 2000;287:2017–2019.
Laurèn P . The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 1965;64:31–49.
Nakamura K, Sugano H, Takagi K . Carcinoma of the stomach in incipient phase: its histogenesis and histological appearances. GANN 1968;59:251–258.
Endoh Y, Tamura G, Motoyama T, et al. Well-differentiated adenocarcinoma mimicking complete-type intestinal metaplasia in the stomach. Hum Pathol 1999;30:826–832.
Endoh Y, Sakata K, Tamura G, et al. Cellular phenotypes of differentiated-type adenocarcinomas and precancerous lesions of the stomach are dependent on the genetic pathways. J Pathol 2000;191:257–263.
Correa P . Helicobacter pylori and gastric carcinogenesis. Am J Surg Pathol 1995;19 (Suppl 1):S37–S43.
Cuello C, Correa P, Zarama P, et al. Histopathology of gastric dysplasias: correlations with gastric juice chemistry. Am J Surg Pathol 1979;3:491–500.
Jass JR . A classification of gastric dysplasia. Histopathology 1983;7:181–193.
Misdraji J, Lauwers GY . Gastric epithelial dysplasia. Semin Diagn Pathol 2002;19:20–30.
Abraham SC, Montgomery EA, Singh VK, et al. Gastric adenomas. Intestinal-type and gastric-type adenomas differ in the risk of adenocarcinoma and presence of background mucosal pathology. Am J Surg Pathol 2002;26:1276–1285.
Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 2001;345:784–789.
Peek Jr RM, Blaser MJ . Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer 2002;2:28–37.
Stolte M, Meining A . Helicobacter pylori gastritis of the gastric carcinoma phenotype: is histology capable of identifying high-risk gastritis? J Gastroenterol 2000;35:98–101.
Sepulveda A, Peterson LE, Shelton J, et al. Histologic patterns of gastritis in H. pylori-infected individuals with a family history of gastric cancer. Am J Gastroenterol 2002;97:1365–1370.
Meining A, Stolte M, Hatz R, et al. Differing degree and distribution of gastritis in Helicobacter pylori-associated diseases. Virchows Arch 1997;431:11–15.
Miehlke S, Hackelsberger A, Meining A, et al. Severe expression of corpus gastritis is characteristic in gastric cancer patients infected with Helicobacter pylori. Br J Cancer 1998;78:263–266.
Dixon MF, Genta RM, Yardley JH, et al. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 1996;20:1161–1181.
Schlemper RJ, Riddle RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut 2000;47:251–255.
Stanley RH, Aaltonen LA, (eds) Pathology and Genetics of Tumours of the Digestive System. World Health Organization Classification of Tumours. IARC Press: Lyon, 2000.
Yu E, Lee HK, Kim HR, et al. Acute inflammation of the proliferative zone of gastric mucosa in Helicobacter pylori gastritis. Pathol Res Pract 1999;195:689–697.
Meining A, Riedl B, Stolte M . Features of gastritis predisposing to gastric adenoma and early gastric cancer. J Clin Pathol 2002;55:770–773.
Penta JS, Johnson FM, Wachsman JT, et al. Mitochondrial DNA in human malignancy. Mutat Res 2001;488:119–133.
Baik SC, Youn HS, Chung MH, et al. Increased oxidative damage in Helicobacter pylori-infected human gastric mucosa. Cancer Res 1996;56:1279–1282.
Lièvre A, Chapusot C, Bouvier A-M, et al. Clinical value of mitochondrial mutations in colorectal cancer. J Clin Oncol 2005;23:3517–3525.
Chatterjee A, Mambo E, Sidransky D . Mitochondrial DNA mutations in human cancer. Oncogene 2006;25:4663–4674.
Parsons TJ, Muniec DS, Sullivan K, et al. A high observed substitution rate in the human mitochondrial DNA control region. Nat Genet 1997;15:363–368.
Tully LA, Parsons TJ, Steighner RJ, et al. A sensitive denaturing gradient-gel electrophoresis assay reveals a high frequency of heteroplasmy in hypervariable region 1 of the human mtDNA control region. Am J Hum Genet 2000;67:432–443.
Simonnet H, Alazard N, Pfeiffer K, et al. Low mitochondrial respiratory chain content correlates with tumor aggressiveness in renal cell carcinoma. Carcinogenesis 2002;23:759–768.
Loft S, Moller P . Oxidative DNA damage and human cancer: need for cohort studies. Antioxid Redox Signal 2006;8:1021–1031.
Desler C, Munch-Petersen B, Stevnsner T, et al. Mitochondria as determinant of nucleotide pools and chromosomal stability. Mutat Res 2007;17:13–17.
Verma M, Kumar D . Application of mitochondrial genome information in cancer epidemiology. Clin Chim Acta 2007;383:41–50.
Modica-Napolitano JS, Kulaviec M, Singh KK . Mitochondria and human cancer. Curr Mol Med 2007;7:121–131.
Baysal BE . Role of mitochondrial mutations in cancer. Endocr Pathol 2006;17:203–212.
Lee HC, Hsu LS, Yin PH, et al. Heteroplasmic mutation of mitochondrial DNA D-loop and 4977-bp deletion in human cancer cells during mitochondrial DNA depletion. Mitochondrion 2007;7:157–163.
Jass JR, Whitehall VL, Young J, et al. Emerging concepts in colorectal neoplasia. Gastroenterology 2002;123:862–876.
Acknowledgements
This research was supported by grants from the Italian Ministry of University and Research (MURST) to the Department of Human Pathology, University Hospital, Messina; Department of Clinical and Experimental Medicine, Gastroenterology Unit, University ‘Federico II,’ Naples; and Department of Oncology and Neuroscience of the University ‘G d’Annunzio’ of Chieti-Pescara.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Rigoli, L., Di Bella, C., Verginelli, F. et al. Histological heterogeneity and somatic mtDNA mutations in gastric intraepithelial neoplasia. Mod Pathol 21, 733–741 (2008). https://doi.org/10.1038/modpathol.2008.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2008.58
Keywords
This article is cited by
-
Paragangliomas arise through an autonomous vasculo-angio-neurogenic program inhibited by imatinib
Acta Neuropathologica (2018)
-
Arsenic trioxide promotes mitochondrial DNA mutation and cell apoptosis in primary APL cells and NB4 cell line
Science China Life Sciences (2010)