Abstract
Objective:
To characterize in-hospital outcomes of premature infants diagnosed with severe bronchopulmonary dysplasia (BPD).
Study Design:
Retrospective cohort study including premature infants with severe BPD discharged from 348 Pediatrix Medical Group neonatal intensive care units from 1997 to 2015.
Results:
There were 10 752 infants with severe BPD, and 549/10 752 (5%) died before discharge. Infants who died were more likely to be male, small for gestational age, have received more medical interventions and more frequently diagnosed with surgical necrotizing enterocolitis, culture-proven sepsis and pulmonary hypertension following 36 weeks of postmenstrual age compared with survivors. Approximately 70% of infants with severe BPD were discharged by 44 weeks of postmenstrual age, and 86% were discharged by 48 weeks of postmenstrual age.
Conclusions:
A majority of infants diagnosed with severe BPD were discharged home by 44 weeks of postmenstrual age. These results may inform discussions with families regarding the expected hospital course of infants diagnosed with severe BPD.
Similar content being viewed by others
Introduction
Bronchopulmonary dysplasia (BPD) is the most common and severe pulmonary complication of prematurity.1 The incidence of BPD may be increasing because of improvement in the survival of infants at earlier gestational ages (GAs).2 The severity of BPD is correlated with long-term health outcomes. A consensus from the National Institutes of Health in 2001 proposed the classification of BPD into mild, moderate and severe categories based on the level of respiratory support at 36 weeks of postmenstrual age (PMA).3 Compared with infants with mild or moderate BPD, infants with severe BPD are more likely to be rehospitalized following discharge for pulmonary causes, receive medications such as diuretics and bronchodilators and have more severe neurodevelopmental impairment at the 18- to 22-month follow-up visit.4, 5, 6, 7
Although infants with severe BPD have a longer initial hospitalization than their peers without BPD, antecedents, comorbidities and in-patient resource use in this population are not well defined. In an effort to describe the clinical course of infants with severe BPD, we identified medical interventions and in-hospital clinical outcomes in infants born at <30 weeks of GA diagnosed with severe BPD. We hypothesized that infants with severe BPD who died during primary hospitalization were more likely to be born at earlier GAs and require more medical interventions than those infants who survived to discharge.
Methods
Data source and study population
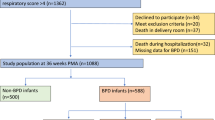
We obtained data from the Pediatrix Medical Group Clinical Data Warehouse that prospectively captures clinical information entered into an electronic health record by clinicians at 348 neonatal intensive care units.8 We extracted information on prenatal characteristics, demographics, exposure to medications and interventions while in the hospital, as well as in-hospital clinical outcomes and level of respiratory support at the time of death or discharge. We included all inborn infants at <30 weeks of GA discharged between 1997 and 2015 and diagnosed with severe BPD. We excluded infants discharged before 36 weeks of PMA and those with missing data on mortality.
Definitions
We defined severe BPD as those infants receiving positive pressure (defined as nasal continuous positive airway pressure, high-flow nasal cannula (HFNC) (>1 l min−1), nasal intermittent positive pressure ventilation, conventional ventilation or high-frequency ventilation) at 36 weeks of PMA. We did not include infants receiving supplemental oxygen ⩾30% via low-flow nasal cannula (⩽1 l min−1) in our definition as we wanted to identify the most severe cases of BPD and the actual oxygen concentration delivered via low-flow nasal cannula varies depending on the size of the nares, the amount of mouth breathing and the infant’s tidal volume and inspiratory time.9, 10 Furthermore, data from the Pediatrix Medical Group Clinical Data Warehouse includes a single measurement of oxygen requirement for a given day, and this would not conform to the current NICHD (National Institute of Child Health and Human Development) definition of severe BPD. We defined small for gestational age as <10th percentile for age at birth as described by Olsen et al.11 We identified exposures to medical interventions including the use of diuretics (acetazolamide, amiloride, bumetanide, chlorothiazide, diazoxide, ethacrynic acid, furosemide, hydrocholorothiazide, metolazone and spironolactone), sildenafil, stimulants (aminophylline, doxapram, caffeine and theophylline), steroids (dexamethasone, prednisolone and prednisone), inhaled medications (budesonide, albuterol and levalbuterol) and inhaled nitric oxide. We examined the incidence of in-hospital outcomes including sepsis, defined as bacteremia with an organism not typically considered a contaminant, intraventricular hemorrhage grade III or IV, surgical necrotizing enterocolitis, pulmonary hypertension as a diagnosis by the clinician, gastrostomy tube placement and tracheostomy before and following diagnosis of severe BPD.
In order to show the evolving clinical course throughout hospitalization, we reviewed the level of respiratory support in 4-week intervals for those infants who remained hospitalized following the diagnosis of severe BPD. We also included the number of infants who had died, had been discharged or remained in-hospital at each of the 4-week intervals following diagnosis of BPD.
Statistical analysis
The unit of observation for this study was the infant. We used standard summary statistics, including medians (interquartile ranges) and counts (percentages), to describe categorical study variables. We compared distributions of study variables across categories using Wilcoxon rank sum, χ2 and Fisher’s exact tests where appropriate. All analyses were performed using Stata SE 14.2 (StataCorp, College Station, TX, USA) and assumed a significance limit of α=0.05. The study was approved by the Duke University Health System Institutional Review Board without the need for written informed consent as the data were collected without identifiers.
Results
We identified 10 752 infants diagnosed with severe BPD at 36 weeks of PMA. The number of infants with severe BPD who died before discharge was 549/10 752 (5%). At the time of diagnosis, 2525/10 752 (23%) were receiving mechanical ventilation, and 8227/10 752 (77%) were receiving HFNC, continuous positive airway pressure or nasal intermittent positive-press ventilation. The median GA and birth weight of the cohort were 26 weeks (interquartile range: 25 to 27) and 755 g (628 to 920), respectively. Median GA and birth weight were lower in the infants who died compared with those who survived to discharge, GA 25 weeks (24 to 27) vs 26 weeks (25 to 27), P=0.003, and birth weight 650 g (560 to 810) vs 760 g (630 to 925), P<0.001. Infants who died were more likely male and small for gestational age (Table 1). Infants who died were more likely to be exposed to diuretics, inhaled medications, sildenafil, stimulants, steroids and inhaled nitric oxide before 36 weeks of PMA (Table 2). No statistically significant difference was found in the exposure to surfactant or supplemental oxygen between the two groups.
Several events were diagnosed more frequently before 36 weeks of PMA in infants who died compared with those who survived, including intraventricular hemorrhage, surgical necrotizing enterocolitis, pulmonary hypertension and culture-proven sepsis (Table 3). Diagnosis of surgical necrotizing enterocolitis, pulmonary hypertension and culture-proven sepsis after 36 weeks of PMA occurred more frequently in infants who died compared with those who survived. Infants who died were more likely to receive mechanical ventilation after diagnosis than the group who survived to discharge (97% vs 39%, P<0.001) and received more days on the ventilator until death or discharge, median number of days 31 (11 to 64) vs 0 (0 to 4). Following diagnosis, 1019 infants (10%) who survived received a g-tube compared with 77 infants (14%) who died (P=0.002), and 302 infants (3%) who survived received a tracheostomy compared with 64 infants (12%) who died (P<0.001). In all, 57% of infants discharged from the hospital received supplemental oxygen, and 3% received mechanical ventilation at the time of discharge (Supplementary Table 1).
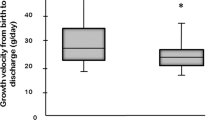
An increasing proportion of infants remaining hospitalized received mechanical ventilation (Figure 1). Whereas 24% of infants received some form of mechanical ventilation at 36 weeks of PMA, this number increased to 48% in those infants remaining hospitalized at 56 weeks of PMA. Of the infants with severe BPD, 70% were discharged by 44 weeks of PMA and 86% were discharged by 48 weeks of PMA (Table 4). The time period with the largest number of deaths occurred between 36 and 40 weeks of PMA. Of the 2525 infants receiving mechanical ventilation at 36 weeks of PMA, 1860 (74%) were discharged home before 52 weeks of PMA, 336 (13%) died and 329 (13%) remained hospitalized at 52 weeks of PMA. Of the 8117 infants receiving HFNC or continuous positive airway pressure at 36 weeks of PMA, 7907 (96%) were discharged before 52 weeks of PMA, 108 (1%) died and 212 (3%) remained hospitalized at 52 weeks of PMA.
Respiratory support over time in hospitalized premature infants with severe bronchopulmonary dysplasia (BPD). CPAP, continuous positive airway pressure; CV, conventional mechanical ventilation; HFNC, high-flow nasal cannula; HFV, high-frequency ventilation; NIPPV, nasal intermittent positive pressure ventilation.
Discussion
We found that the majority of infants diagnosed with severe BPD at 36 weeks of PMA survive until discharge and that most are discharged by 44 weeks of PMA. An important caveat is that mortality in this study does include infants who died before the diagnosis of BPD at 36 weeks of PMA. Although all of the infants included in our study received positive pressure at the time of diagnosis, the proportion of infants receiving some form of positive pressure decreased at 40 weeks of PMA, and actually increased thereafter. For example, after 44 weeks of PMA, an increasingly higher percentage of infants remaining hospitalized received mechanical ventilation, likely reflecting that the most critically ill infants had a longer duration of primary hospitalization. These results suggest that at the estimated date of delivery, approximately two-thirds of infants with severe BPD will remain hospitalized and a relatively small percentage of these hospitalized infants will receive mechanical ventilation. This information may help inform discussions with families regarding the expected hospital course of infants diagnosed with severe BPD.
We found that about half of infants diagnosed with severe BPD were exposed to postnatal dexamethasone, prednisone or prednisolone. Approximately 40% of infants in our cohort received these steroids before 36 weeks of PMA and those who subsequently died were more likely to receive steroids (49% vs 37%). The proposed benefits of steroids in the infant include enhancement of endogenous surfactant and antioxidant production, amelioration of the inflammatory process contributing to the development of BPD and reduction of pulmonary edema and bronchospasm, all of which may reduce the incidence of BPD. The most recent American Academy of Pediatrics guidelines on the use of postnatal steroids in premature infants at risk for BPD advise clinicians to, while consulting the infant’s parents, balance the risks of using a short course of low-dose corticosteroids against the risks of evolving pulmonary disease and prolonged mechanical ventilation.12
We found that a lower percentage of infants who died (79%) were exposed to stimulant therapy before 36 weeks of PMA compared with those infants who survived (93%). Although this finding is surprising, we speculate that some of the infants who received prolonged mechanical ventilation may not have been started on stimulant therapy as extubation was not anticipated and central apnea cannot occur while on mechanical ventilation. Several studies have found that early administration of caffeine in premature infants is associated with an increase in survival without BPD.13, 14, 15 The early use of caffeine should be strongly considered in infants at high risk for BPD regardless of respiratory support.
Premature infants with a diagnosis of BPD were found to require a high number of primary care provider office visits and prescription medications in the first year of life.16 Approximately 3% of infants in our study who were discharged home received mechanical ventilation, with approximately the same number receiving tracheostomy. More than half of infants with severe BPD discharged home received supplemental oxygen. Previous investigators found that premature infants with BPD who were discharged home with supplemental oxygen were more likely to receive respiratory medications, supplemental oxygen and more frequent physician visits at 36 months of life compared with infants with BPD who were discharged home without supplemental oxygen.17 Approximately 1 in 10 infants in our study who survived to discharge received a gastrostomy tube during primary hospitalization. Infants with BPD who receive gastrostomy tubes were found to have longer primary hospitalizations, are more likely to receive ventilatory support and supplemental oxygen at the time of discharge and are more likely to be rehospitalized in the first 2 years of life compared with infants with BPD who do not receive gastrostomy tubes.18
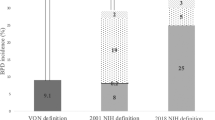
There are several limitations to our study. As the purpose of our study was to determine in-hospital outcomes in premature infants diagnosed with severe BPD, we did not include infants who died before 36 weeks of PMA or infants who were transferred to other facilities outside the network. Our definition of severe BPD was based on the use of positive pressure at 36 weeks of PMA. The inclusion of HFNC (considered >1 l min−1 via nasal cannula) in our definition of positive pressure ventilation does not directly measure distending pressure because the measured component is liter flow.19, 20 HFNC is an increasingly common modality used in neonatal intensive care units worldwide because of its perceived benefits in ease of use compared with nasal continuous positive airway pressure.21, 22 We included HFNC as positive pressure ventilation because we believe that the intent by the clinician was to provide positive pressure ventilation, even though the exact distending pressure is unmeasured. Although infants receiving low-flow nasal cannula (considered <1 l min−1) with a fraction of inspired oxygen ⩾0.3 at 36 weeks of PMA would be considered to have severe BPD based on the 2001 National Institutes of Health consensus, we did not include these infants in our definition of BPD as the oxygen concentration that an infant receives via nasal cannula is not precise.23 This is because of the entrainment of room air through the mouth and nose that may result in the delivery of a lower fraction of inspired oxygen than what is recorded. A further limitation is that the diagnosis of pulmonary hypertension was based on documentation by clinicians and no echocardiogram images or reports were reviewed for this study.
In summary, we describe the in-hospital outcomes of premature infants born <30 weeks of GA who were subsequently diagnosed with severe BPD. A majority were discharged home by 44 weeks of PMA and a small percentage of these infants died. The infants receiving prolonged mechanical ventilation were more likely to remain hospitalized, and of those infants who died, nearly all (>90%) died while receiving mechanical ventilation. Although the incidence of severe BPD is relatively rare compared with the number of premature infants born each year worldwide, the substantial health-care resources and familial stress associated with an increased morbidity and mortality, including prolonged hospitalization, demand further efforts to prevent and more effectively treat infants with severe BPD. Further studies using large sample sizes in collaboration with multiple clinical sites will be required to determine long-term pulmonary and neurodevelopmental outcomes in these infants and develop potential therapies to prevent and treat BPD.
References
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 2015; 314 (10): 1039–1051.
Parker RA, Lindstrom DP, Cotton RB . Improved survival accounts for most, but not all, of the increase in bronchopulmonary dysplasia. Pediatrics 1992; 90 (5): 663–668.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163 (7): 1723–1729.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005; 116 (6): 1353–1360.
Laughon M, O'Shea MT, Allred EN, Bose C, Kuban K, Van Marter LJ et al. Chronic lung disease and developmental delay at 2 years of age in children born before 28 weeks' gestation. Pediatrics 2009; 124 (2): 637–648.
Van Marter LJ, Kuban KC, Allred E, Bose C, Dammann O, O'Shea M et al. Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch Dis Child Fetal Neonatal Ed 2011; 96 (1): F20–F29.
Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum Dev 2012; 88 (7): 509–515.
Spitzer AR, Ellsbury D, Clark RH . The Pediatrix BabySteps(R) Data Warehouse - a unique national resource for improving outcomes for neonates. Indian J Pediatr 2015; 82 (71): 669.
Benaron DA, Benitz WE . Maximizing the stability of oxygen delivered via nasal cannula. Arch Pediatr Adolesc Med 1994; 148 (3): 294–300.
Vain NE, Prudent LM, Stevens DP, Weeter MM, Maisels MJ . Regulation of oxygen concentration delivered to infants via nasal cannulas. Am J Dis Child 1989; 143 (12): 1458–1460.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS . New intrauterine growth curves based on United States data. Pediatrics 2010; 125 (2): e214–e224.
Watterberg KL, American Academy of Pediatrics. Committee on Fetus and Newborn. Policy statement—postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Pediatrics 2010; 126 (4): 800–808.
Lodha A, Seshia M, McMillan DD, Barrington K, Yang J, Lee SK et al. Association of early caffeine administration and neonatal outcomes in very preterm neonates. JAMA Pediatr 2015; 169 (1): 33–38.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006; 354 (20): 2112–2121.
Taha D, Kirkby S, Nawab U, Dysart KC, Genen L, Greenspan JS et al. Early caffeine therapy for prevention of bronchopulmonary dysplasia in preterm infants. J Matern Fetal Neonatal Med 2014; 27 (16): 1698–1702.
Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ . Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol 2008; 28 (10): 696–701.
Lodha A, Ediger K, Rabi Y, Lodha S, Tang S, Bhandari A et al. Does chronic oxygen dependency in preterm infants with bronchopulmonary dysplasia at NICU discharge predict respiratory outcomes at 3 years of age? J Perinatol 2015; 35 (7): 530–536.
McGrath-Morrow SA, Hayashi M, Aherrera AD, Collaco JM . Respiratory outcomes of children with BPD and gastrostomy tubes during the first 2 years of life. Pediatr Pulmonol 2014; 49 (6): 537–543.
McQueen M, Rojas J, Sun SC, Tero R, Ives K, Bednarek F et al. Safety and long term outcomes with high flow nasal cannula therapy in neonatology: a large retrospective cohort study. J Pulm Respir Med 2014; 4 (6): 216.
Manley BJ, Owen LS . High-flow nasal cannula: mechanisms, evidence and recommendations. Semin Fetal Neonatal Med 2016; 21 (3): 139–145.
Nath P, Ponnusamy V, Willis K, Bissett L, Clarke P . Current practices of high and low flow oxygen therapy and humidification in UK neonatal units. Pediatr Int 2010; 52 (6): 893–894.
Manley BJ, Owen L, Doyle LW, Davis PG . High-flow nasal cannulae and nasal continuous positive airway pressure use in non-tertiary special care nurseries in Australia and New Zealand. J Paediatr Child Health 2012; 48 (1): 16–21.
Walsh M, Engle W, Laptook A, Kazzi SN, Buchter S, Rasmussen M et al. Oxygen delivery through nasal cannulae to preterm infants: can practice be improved? Pediatrics 2005; 116 (4): 857–861.
Acknowledgements
This project was completed, in part, by grants from the National Institutes of Health (1R21HD080606-01A1) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (1R25HD076475).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
CPH receives salary support for research from the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR001117); PBS receives salary support for research from the National Institutes of Health (NIH-1R21HD080606-01A1) and the National Institute for Child Health and Human Development (HHSN275201000003I); SP-W receives salary support for research from the Gerber Foundation and the National Institute of Allergy and Infectious Diseases (R01 AI1000067-01; principal investigator (PI) De Paris); MML is supported by the US government for his work in pediatric and neonatal clinical pharmacology by Eunice Kennedy Shriver National Institute of Child Health and Human Development (Contract HHSN267200700051C; PI Benjamin), the Food and Drug Administration Office of Orphan Product Development (R01 FD005101; PI Laughon) and the National Heart, Lung and Blood Institute (R34 HL124038; PI Laughon).
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Jackson, W., Hornik, C., Messina, J. et al. In-hospital outcomes of premature infants with severe bronchopulmonary dysplasia. J Perinatol 37, 853–856 (2017). https://doi.org/10.1038/jp.2017.49
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.49
This article is cited by
-
Risk factors that affect the degree of bronchopulmonary dysplasia in very preterm infants: a 5-year retrospective study
BMC Pediatrics (2022)
-
Early Career Investigator Spotlight: Wesley M. Jackson
Pediatric Research (2022)
-
Safety of sildenafil in extremely premature infants: a phase I trial
Journal of Perinatology (2022)
-
A comparison of newer classifications of bronchopulmonary dysplasia: findings from the Children’s Hospitals Neonatal Consortium Severe BPD Group
Journal of Perinatology (2022)
-
Safety of sildenafil in premature infants with severe bronchopulmonary dysplasia (SILDI-SAFE): a multicenter, randomized, placebo-controlled, sequential dose-escalating, double-masked, safety study
BMC Pediatrics (2020)