Abstract
Objective:
The aim of this study was to identify the best sedation/analgesia protocol for laser photocoagulation (PC) of retinopathy of prematurity (ROP).
Study Design:
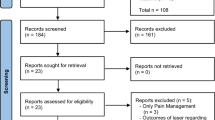
This multicenter observational study included five hospitals, each using a specific sedation/analgesia protocol: local anesthesia with oxybuprocaine hydrochloride (Group L); intravenous pentazocine (Group P); intravenous fentanyl (Group F); air, oxygen and sevoflurane (AOS) inhalation (Group I). The groups were compared for pain responses, vital signs and adverse events.
Results:
Heart rates and systemic blood pressures were elevated by PC in Groups L and P and Groups L, P and F, respectively. Moreover, poor analgesic efficacy was recognized in Groups L, P and F. In contrast, Group I experienced hypothermia, enteral feeding intolerance and apnea more frequently.
Conclusion:
From the viewpoint of sedation/pain relief, AOS anesthesia should be the best protocol. However, considering all the various factors together, the most reasonable one can be varied based on the patient’s condition and hospital.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Haigh PM, Chiswick ML, O'Donoghue EP . Retinopathy of prematurity: systemic complications associated with different anaesthetic techniques at treatment. Br J Ophthalmol 1997; 81 (4): 283–287.
Chen SD, Sundaram V, Wilkinson A, Patel CK . Variation in anaesthesia for the laser treatment of retinopathy of prematurity—a survey of ophthalmologists in the UK. Eye (Lond) 2007; 21 (8): 1033–1036.
Anand KJ, Carr DB . The neuroanatomy, neurophysiology, and neurochemistry of pain, stress, and analgesia in newborns and children. Pediatr Clin N Am 1989; 36 (4): 795–822.
Giannakoulopoulos X, Sepulveda W, Kourtis P, Glover V, Fisk NM . Fetal plasma cortisol and beta-endorphin response to intrauterine needling. Lancet 1994; 344 (8915): 77–81.
Taddio A, Goldbach M, Ipp M, Stevens B, Koren G . Effect of neonatal circumcision on pain responses during vaccination in boys. Lancet 1995; 345 (8945): 291–292.
Taddio A, Katz J, Ilersich AL, Koren G . Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet 1997; 349 (9052): 599–603.
Laudenbach V, Calo G, Guerrini R, Lamboley G, Benoist JF, Evrard P et al. Nociceptin/orphanin FQ exacerbates excitotoxic white-matter lesions in the murine neonatal brain. J Clin Invest 2001; 107 (4): 457–466.
Loepke AW, Soriano SG . An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg 2008; 106 (6): 1681–1707.
Mellon RD, Simone AF, Rappaport BA . Use of anesthetic agents in neonates and young children. Anesth Analg 2007; 104 (3): 509–520.
Zhu C, Gao J, Karlsson N, Li Q, Zhang Y, Huang Z et al. Isoflurane anesthesia induced persistent, progressive memory impairment, caused a loss of neural stem cells, and reduced neurogenesis in young, but not adult, rodents. J Cereb Blood Flow Metab 2010; 30 (5): 1017–1030.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123 (7): 991–999.
Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C . The development of a tool to assess neonatal pain. Neonatal Netw 1993; 12 (6): 59–66.
Parulekar MV, Chen SD, Patel CK . Sub-tenon's local anaesthesia for the treatment of retinopathy of prematurity with diode laser. Eye (Lond) 2008; 22 (3): 375–379.
Woodhead DD, Lambert DK, Molloy DA, Schmutz N, Righter E, Baer VL et al. Avoiding endotracheal intubation of neonates undergoing laser surgery for retinopathy of prematurity. J Perinatol 2007; 27 (4): 209–213.
Kirwan C, O'Keefe M, Prendergast M, Twomey A, Murphy J . Morphine analgesia as an alternative to general anaesthesia during laser treatment of retinopathy of prematurity. Acta Ophthalmol Scand 2007; 85 (6): 644–647.
Batton DG, Barrington KJ, Wallman C . Prevention and management of pain in the neonate: an update. Pediatrics 2006; 118 (5): 2231–2241.
Dilli D, Ilarslan NE, Kabatas EU, Zenciroglu A, Simsek Y, Okumus N . Oral sucrose and non-nutritive sucking goes some way to reducing pain during retinopathy of prematurity eye examinations. Acta Paediatr 2014; 103 (2): e76–e79.
Schulenburg WE, Bloom PA . Current problems in the management of ROP. Acta Ophthalmol Scand Suppl 1995; 214: 14–16.
Acknowledgements
We are grateful to Dr Tetsuo Hattori, Dr Reina Hyodo and Dr Yoshihiro Tanahashi for collecting the data. The authors have not received any financial support for the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Sato, Y., Oshiro, M., Takemoto, K. et al. Multicenter observational study comparing sedation/analgesia protocols for laser photocoagulation treatment of retinopathy of prematurity. J Perinatol 35, 965–969 (2015). https://doi.org/10.1038/jp.2015.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.112
This article is cited by
-
Safety profile of anesthetic modalities during laser treatment for retinopathy of prematurity: a systematic review
Journal of Perinatology (2023)
-
Retinopathy of prematurity treatment: Asian perspectives
Eye (2020)
-
Low dose fentanyl infusion versus 24% oral sucrose for pain management during laser treatment for retinopathy of prematurity—an open label randomized clinical trial
European Journal of Pediatrics (2020)