Abstract
Objective
To study the efficacy of intranasal fentanyl as an adjunct for pain management during screening for retinopathy of prematurity (ROP) in preterm infants.
Study design
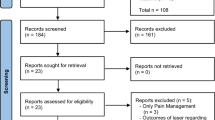
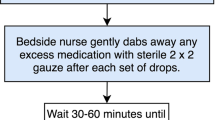
In this single center, double blinded, randomized controlled trial, preterm neonates between 30 and 34 weeks postmenstrual age received either intranasal fentanyl (2 mcg/kg) or intranasal normal saline through a mucosal atomization device 5 min prior to the first ROP-screening examination. Both the groups received standard pain relief strategies (oral sucrose, 0.5% proparacaine eye drops and physical containment). The primary outcome was premature infant pain profile-revised (PIPP-R) score during the screening.
Results
A total of 111 infants were enrolled. PIPP-R score during the retinal examination was significantly lower in the fentanyl group (8.3 versus 11.5, mean difference: 3.2 (2.46–4.06), P < 0.001). There was no significant difference in the incidence of adverse effects.
Conclusion
Intranasal fentanyl significantly reduced the pain associated with retinal examination without increasing the risk of respiratory depression. Large RCTs are required to verify the efficacy and safety of intranasal fentanyl for acute procedural pain in neonates.
Clinical Trial Registration
CTRI/2017/12/011016.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kirchner L, Jeitler V, Pollak A, Mullner-Eidenbock A, Weinzettel R, Kraschl R, et al. Must screening examinations for retinopathy of prematurity necessarily be painful? Retina. 2009;29:586–91.
Cohen AM, Cook N, Harris MC, Ying GS, Binenbaum G. The pain response to mydriatic eyedrops in preterm infants. J Perinatol. 2013;33:462–5.
Vinall J, Grunau RE. Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr Res 2014;75:584–7.
Valeri BO, Holsti L, Linhares MB. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31:355–62.
Walker SM. Long-term effects of neonatal pain. Semin Fetal Neonatal Med. 2019;24:101005.
Pillai Riddell RR, Racine NM, Gennis HG, Turcotte K, Uman LS, Horton RE, et al. Non-pharmacological management of infant and young child procedural pain. Cochrane Database Syst Rev. 2015;2:Cd006275.
Shah PS, Herbozo C, Aliwalas LL, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2012;12:Cd004950.
Johnston C, Campbell-Yeo M, Disher T, Benoit B, Fernandes A, Streiner D, et al. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst Rev. 2017;2:Cd008435.
Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2016;7:Cd001069.
Ohlsson A, Shah PS. Paracetamol (acetaminophen) for prevention or treatment of pain in newborns. Cochrane Database Syst Rev. 2016;10:Cd011219.
Dempsey E, McCreery K. Local anaesthetic eye drops for prevention of pain in preterm infants undergoing screening for retinopathy of prematurity. Cochrane Database Syst Rev. 2011;7:Cd007645.
Francis K. What is best practice for providing pain relief during retinopathy of prematurity eye examinations? Adv Neonatal Care. 2016;16:220–8.
Disher T, Cameron C, Mitra S, Cathcart K, Campbell-Yeo M. Pain-Relieving Interventions for Retinopathy of Prematurity: A Meta-analysis. Pediatrics. 2018;142:pii: e20180401.
Hall RW, Anand KJ. Pain management in newborns. Clin Perinatol 2014;41:895–924.
Hartley C, Moultrie F, Hoskin A, Green G, Monk V, Bell JL, et al. Analgesic efficacy and safety of morphine in the Procedural Pain in Premature Infants (Poppi) study: randomised placebo-controlled trial. Lancet (Lond, Engl). 2018;392:2595–605.
McNair C, Graydon B, Taddio A. A cohort study of intranasal fentanyl for procedural pain management in neonates. Paediatr Child Health. 2018;23:e170–e5.
Ku LC, Simmons C, Smith PB, Greenberg RG, Fisher K, Hornik CD, et al. Intranasal midazolam and fentanyl for procedural sedation and analgesia in infants in the neonatal intensive care unit. J Neonatal Perinatal Med. 2019;12:143–8.
Thigpen JC, Odle BL, Harirforoosh S. Opioids: a review of pharmacokinetics and pharmacodynamics in neonates, infants, and children. Eur J Drug Metab Pharmacokinet. 2019;44:591–609.
Orge FH, Lee TJ, Walsh M, Gordon K. Comparison of fentanyl and morphine in laser surgery for retinopathy of prematurity. J AAPOS 2013;17:135–9.
Honavar SG. Do we need India-specific retinopathy of prematurity screening guidelines? Indian J Ophthalmol. 2019;67:711–6.
Stevens BJ, Gibbins S, Yamada J, Dionne K, Lee G, Johnston C, et al. The premature infant pain profile-revised (PIPP-R): initial validation and feasibility. Clin J Pain. 2014;30:238–43.
Ballantyne M, Stevens B, McAllister M, Dionne K, Jack A. Validation of the premature infant pain profile in the clinical setting. Clin J Pain. 1999;15:297–303.
Slater R, Hartley C, Moultrie F, Adams E, Juszczak E, Rogers R, et al. A blinded randomised placebo-controlled trial investigating the efficacy of morphine analgesia for procedural pain in infants: trial protocol. Wellcome Open Res. 2016;1:7.
Sethi A, Sankar MJ, Kulkarni S, Thukral A, Chandra P, Agarwal R. Low dose fentanyl infusion versus 24% oral sucrose for pain management during laser treatment for retinopathy of prematurity-an open label randomized clinical trial. Eur J Pediatr. 2019;179:285–92.
Frey TM, Florin TA, Caruso M, Zhang N, Zhang Y, Mittiga MR. Effect of Intranasal ketamine vs fentanyl on pain reduction for extremity injuries in children: the PRIME randomized clinical trial. JAMA Pediatr. 2019;173:140–6.
Murphy A, O’Sullivan R, Wakai A, Grant TS, Barrett MJ, Cronin J, et al. Intranasal fentanyl for the management of acute pain in children. Cochrane Database Syst Rev. 2014:Cd009942.
Harlos MS, Stenekes S, Lambert D, Hohl C, Chochinov HM. Intranasal fentanyl in the palliative care of newborns and infants. J Pain Symptom Manag. 2013;46:265–74.
Norman E, Kindblom JM, Rane A, Berg AC, Schubert U, Hallberg B, et al. Individual variations in fentanyl pharmacokinetics and pharmacodynamics in preterm infants. Acta paediatr (Oslo, Nor: 1992). 2019;108:1441–6.
Voller S, Flint RB, Andriessen P, Allegaert K, Zimmermann LJI, Liem KD, et al. Rapidly maturing fentanyl clearance in preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2019;104:598–603.
Pacifici GM. Clinical pharmacology of fentanyl in preterm infants. A review. Pediatr Neonatol. 2015;56:143–8.
Cole J, Shepherd M, Young P. Intranasal fentanyl in 1–3-year-olds: a prospective study of the effectiveness of intranasal fentanyl as acute analgesia. Emerg Med Australas. 2009;21:395–400.
Borland M, Jacobs I, King B, O’Brien D. A randomised controlled trial comparing intranasal fentanyl to intravenous morphine for managing acute pain in children in the emergency department. Ann Emerg Med. 2007;49:335–40.
Wolfe TR, Braude DA. Intranasal medication delivery for children: a brief review and update. Pediatrics 2010;126:532–7.
Mitchell AJ, Green A, Jeffs DA, Roberson PK. Physiologic effects of retinopathy of prematurity screening examinations. Adv Neonatal Care. 2011;11:291–7.
Stevens B, Johnston C, Taddio A, Gibbins S, Yamada J. The premature infant pain profile: evaluation 13 years after development. Clin J Pain. 2010;26:813–30.
Acknowledgements
None of the authors received any grant for producing the manuscript.
Author information
Authors and Affiliations
Contributions
HB and MS conceptualized and designed the study. MS recorded the study data and drafted the first manuscript. LS and NK conducted the literature search and critically reviewed the manuscript. PA and AD supervised the conduct of the study and critically reviewed the manuscript. All authors approved the submission of this version of manuscript and take full responsibility for the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sindhur, M., Balasubramanian, H., Srinivasan, L. et al. Intranasal fentanyl for pain management during screening for retinopathy of prematurity in preterm infants: a randomized controlled trial. J Perinatol 40, 881–887 (2020). https://doi.org/10.1038/s41372-020-0608-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0608-2