Abstract
Objective:
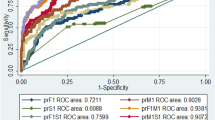
The development and evaluation of a labor risk model consisting of a combination of antepartum risk factors and intrapartum fetal heart rate (FHR) characteristics that can reliably identify those infants at risk for adverse neonatal outcome in labor.
Study design:
A nested case–control study of term singleton deliveries at the nine hospitals between March 2007 and December 2009. Eligibility criteria included: gestational age ⩾37.0 weeks; singleton pregnancy; documented continuous FHR monitoring for ⩾2 h before delivery; assessment of FHR tracing at least every 20 min; and, available maternal and neonatal outcomes. Adverse neonatal outcome was defined as nonanomalous infants admitted to the newborn intensive care unit with either a 5 minute Apgar score <7 or an umbilical artery pH<7.1. Initial risk score was determined using data available at 1 h after admission. Patients with an initial risk score between 7 and 15 were considered high risk. Intrapartum risk scores were then created for these patients using FHR tracing data and labor characteristics.
Result:
A total of 51 244 patients were identified meeting study criteria. Of the antepartum variables evaluated (n=31), 10 were associated with an adverse outcome. The high-risk group made up 28% of the population and accounted for 59.8% of the adverse outcomes. Intrapartum characteristics were then evaluated in this high-risk group. Intrapartum evaluation identified the highest risk group with a C/S rate of 40% and adverse outcome rate of 11.3%.
Conclusion:
Incorporation of maternal and antepartum risk factors with FHR analysis can improve the ability to identify the fetus at risk in labor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Chen HY, Chauhan SP, Ananth CV, Vintzileos AM, Abuhamad AZ . Electronic fetal heart rate monitoring and its relationship to neonatal and infant mortality in the United States. Am J Obstet Gynecol 2011; 204: 491.e1–10.
Locatelli A, Incerti M, Ghidini A, Greco M, Villa E, Paterlini G . Factors associated with umbilical artery acidemia in term infants with low Apgar scores at 5 min. Eur J Obstet Gynecol Reprod Biol 2008; 139 (2): 146–150.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 116. Management of intrapartum fetal heart rate tracings. Obstet Gynecol 2010; 116: 1232–1240.
Alfrevic Z, Devane D, Gyte GML . Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev 2006; ((Issue 3))Art. No. CD006066.
Macones GA, Hankins GD, Spong CY, Hauth J, Moore T . The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 2008; 112: 661–666.
Horne BD, May HT, Muhlestein JB, Ronnow BS, Lappé DL, Renlund DG et al. Exceptional mortality prediction by risk scores from common laboratory tests. Am J Med 2009; 122: 550–558.
Nelson KB, Elenberg JH . Antecedents of cerebral palsy: multivariate analysis of risk. N Engl J Med 1986; 315: 81–86.
Badawi N, Kurinczuk JJ, Keogh JM, Alessandri LM, O’Sullivan F, Burton PR et al. Antepartm risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ 1998; 317: 1549–1553.
Quilligan EJ, Paul RH . Fetal monitoring: is it worth it? Obstet Gynecol 1975; 45: 96–100.
Grimes DH, Piepert JF . Electronic fetal monitoring as a public health program: the arithmetic of failure. Obstet Gynecol 2010; 116: 1397–1400.
Jackson M, Holmgren CM, Esplin MS, Henry E, Varner MW . Frequency of fetal heart rate categories and short-term neonatal outcome. Obstet Gynecol 2011; 118: 803–808.
Garite TJ, Dildy GA, McNamara H, Nageotte MP, Boehm FH, Dellinger EH et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol 2000; 183: 1049–1058.
Westerhuis MEMH, Visser GHA, Moons KGM, van Beek E, Benders MJ, Bijvoet SM et al. Cardiotocography plus ST analtsis of fetal electrocardiogram compared with cardiotocography only for intrapartum monitoring. Obstet Gynecol 2010; 115: 1173–1180.
Maisonneuve E, Audibert F, Guilbaud L, Lathelize J, Jousse M, Pierre F et al. Risk factors for severe neonatal acidosis. Obstet Gynecol 2011; 118: 818–823.
Low JA, Simpson LL, Tonni G, Chamberlain S . Limitations in the clinical prediction of intrapartum fetal asphyxia. Am J Obstet Gynecol 1995; 172: 801–804.
Herbst A, Wolner-Hanssen P, Ingemarsson I . Risk factors for academia at birth. Obstet Gynecol 1997; 90: 125–130.
Heinonen S, Saarikoski S . Reproductive risk factors of fetal asphyxia at delivery: a population based analysis. J Clin Epidemiol 2001; 54: 407–410.
Acknowledgements
This study was supported by grants funded by Deseret Foundation, Salt Lake City, UT, USA, grant 576.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This study was presented at the 31st Annual Meeting of the Society for Maternal-Fetal Medicine, San Francisco, CA, USA, February 2011.
Rights and permissions
About this article
Cite this article
Holmgren, C., Esplin, M., Jackson, M. et al. A risk stratification model to predict adverse neonatal outcome in labor. J Perinatol 33, 914–918 (2013). https://doi.org/10.1038/jp.2013.64
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.64