Abstract
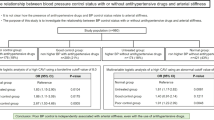
The aim of this study was to evaluate any possible association of homocysteine with arterial stiffness indices in patients with essential arterial hypertension (AH), isolated office hypertension (IOH) and normotensive controls. The final cohort comprised 231 normotensives (NTs, 119 males), 480 patients with IOH (196 males) and 1188 patients with essential AH (713 males). All patients were screened for plasma homocysteine levels and lipidaemic profile and underwent aortic compliance and wave reflection assessment by using carotid-femoral pulse wave velocity (PWVc-f) and aortic augmentation index corrected for heart rate (AIx) accordingly. In the total population, stepwise multiple linear regression analysis showed that homocysteine levels remained a significant determinant of PWV (beta (SE): 0.056 (0.007), P<0.001) and AIx (beta (SE): 0.236 (0.052), P<0.001) independently of the traditional factors affecting arterial stiffness and wave reflection. When the three groups were examined separately, homocysteine levels remained an independent determinant of PWFc-f in all groups (NT: beta (SE): 0.070 (0.022), P=0.002; IOH: beta (SE): 0.109 (0.015), P<0.001; AH: beta (SE): 0.040 (0.009), P<0.001). However, homocysteine levels remained an independent determinant of AIx only in the IOH and AH, but not in the NT group (IOH: beta (SE): 0.302 (0.124), P=0.015; AH: beta (SE): 0.183 (0.057), P=0.001; NT: beta (SE): 0.308 (0.240), P=0.200). This study points to an independent relationship between circulating homocysteine levels, aortic compliance and wave reflection.
Similar content being viewed by others
Introduction
Increased levels of plasma homocysteine have been considered as an independent risk factor for cardiovascular disease.1, 2 Specifically, high plasma homocysteine levels are related to increased risk for myocardial infarction, stroke, heart failure and occlusive peripheral arterial disease.3, 4, 5, 6, 7 Furthermore, hyperhomocysteinaemia is associated with increased carotid intima-media thickness,8 extracranial carotid artery stenosis9 and more advanced atherosclerotic changes in coronary arteries.10 Among the possible mechanisms that these effects are exerted on are increased smooth muscle cell proliferation,11 endothelial dysfunction,12 increased collagen synthesis and deterioration of elastic material of the arterial wall.13
With regard to the relationship between homocysteine levels and hypertension, a synergistic effect of these two parameters on cardiovascular risk10, 14 and an independent relationship between high homocysteine levels and isolated systolic hypertension are reported,15 which was attributed to arterial stiffening. Associations of homocysteine with cardiovascular risk and with alterations in vascular properties have led to studies of its association with arterial stiffness. Thus, there are reports of a significant association between plasma homocysteine pulse pressure16 and arterial pulse wave velocity (PWV);17, 18 however, results are controversial as there are no reports of such associations.19
On account of this controversy in the earlier reports, the purpose of this study was to assess the relationship between plasma homocysteine levels, arterial stiffness and wave reflection indices in patients with arterial hypertension (AH), isolated office hypertension (IOH) and normotensive controls (NC).
Materials and methods
Study population
This retrospective study comprised 2150 patients who visited our outpatient clinic from 2005 to 2008. The study protocol has been approved by the Ethics Committee of Hippokration Hospital. Patients with acute and chronic inflammatory disease, endocrine disorders, chronic obstructive pulmonary disease, malignancy, renal insufficiency (serum creatinine >1.3 mgdl−1), heart failure, recent (<6 months) cerebrovascular event, coronary artery disease, history of stable/unstable angina or past myocardial infraction, ventricular arrhythmia, sinus bradycardia (<55 b.p.m.), sinus tachycardia (>100 b.p.m.) or atrioventricular conduction defects, known diabetes mellitus (earlier antidiabetic treatment) and any condition preventing technically adequate ambulatory blood pressure (BP) monitoring were excluded from the study.
Thus, the final cohort comprised 1899 patients, of which 231 were normotensives (NT), 1188 presented with essential AH and 480 with IOH.
All participants were subjected to the following procedures: physical examination, medical history, repeated clinical BP measurement and blood sampling for laboratory examinations. Patients with borderline office BP and patients reporting normal BP levels outside the clinic were subjected to 24-h ambulatory BP monitoring.
BP measurements
The evaluation of BP was made according to the 2003 European Society of Hypertension/European Society of Cardiology guidelines for adults.20 BP was measured three times with 1 min intervals and with the subject resting comfortably, back supported in the sitting position after a 10–15 min relax period. A mercury sphygmomanometer was used for all measurements with a medium- or a large-size cuff, according to the subject's arm circumference.
Furthermore, 40% of patients underwent ambulatory BP monitoring for 24 h on the non-dominant arm using a Spacelabs 90207 device (SpaceLabs Inc., Redmond, WA, USA). Technical details have been reported earlier.21
Anthropometric and biochemical measurements
For each subject, weight, height and waist to hip (W/H) ratio were measured, and body mass index was also calculated. Waist circumference was measured at the midpoint between the bottom of the rib cage and above the top of the iliac crest from patients at minimal respiration to the nearest 0.1 cm.
All subjects underwent full laboratory evaluation (lipidaemic profile, liver and kidney function indices). The blood samples were collected from the antecubital vein between 8 a.m. and 10 a.m., in a sitting position, after 12 h of fasting and alcohol absence. The biochemical evaluation was carried out in the same laboratory that followed the criteria of the World Health Organization Lipid Reference Laboratories.
Plasma total homocysteine levels were determined using the homocysteine microplate enzyme immunoassay assay (Bio-Rad Laboratories, Oslo, Norway)22 (cut-off points: 4–25 μmol/l).
Measurements of arterial properties
Haemodynamic measurements were conducted in the morning, in a quiet environment, at stable temperature. Subjects were requested to abstain from caffeine, smoking and alcohol for at least 12 h before arterial properties assessment was performed. Systolic BP, diastolic BP and heart rate were measured twice in both arms with automatic mercury (Omron M4-I, CE 0197, Netherlands).
Aortic wave reflection assessment
We used a validated, commercially available system (SphygmoCor; AtCor Medical, Sydney, Australia), which uses the principle of applanation tonometry and appropriate acquisition and analysis software for non-invasive recording and analysis of the arterial pulse. First, from the radial artery recordings, the ensemble-averaged radial pressure waveform is obtained. Then, this is calibrated according to sphygmomanometric systolic and diastolic BP measured in the brachial artery (as there is practically negligible pressure pulse amplification between the brachial and the radial artery; subsequently, the mean radial pressure is calculated by digital integration of the waveform). Thereafter, from the radial artery pressure waveform, the central (aortic) arterial pressure waveform is derived.
Augmentation indices of the central waveform were measured as indices of wave reflection. Augmentation index was defined as augmented pressure divided by pulse pressure and expressed as a percentage. Augmentation index is a composite measure of the magnitude of wave reflection and arterial stiffness, which affects the timing of wave reflection.23 Larger values of augmentation index indicate increased wave reflection from the periphery and/or earlier return of the reflected wave as a result of increased PWV (because of increased arterial stiffness), and vice versa. To take into account the potential effect of heart rate on augmentation index, all values were automatically corrected for heart rate by the sphygmocor software augmentation index corrected for heart rate (AIx).
Aortic stiffness assessment
The pulse travels at a higher velocity in a stiff aorta and vice versa. Carotid-femoral pulse wave velocity (PWVc-f) is a well-established index of arterial elastic properties and a prognosticator of cardiovascular risk. PWVc-f was calculated from measurements of pulse transit time and the distance travelled between two recording sites (PWV=distance (m)/transit time (s)) using a validated non-invasive device (Complior; Dupont Medical, Pantin, France), which allows online pulse wave recording and automatic calculation of PWV.24 Two different pulse waves were obtained simultaneously at two sites (at the base of the neck for the common carotid and over the right-femoral artery) with two transducers. The distance was defined as (distance from the suprasternic notch to femoral artery)—(distance from the carotid artery to the suprasternic notch).
Statistical analysis
Data are presented as mean±SEM except if differently indicated. Comparisons between the baseline characteristics of the three study groups (NC, IOH and AH) were performed after analysis of variance. Nominal data were compared by the χ2-test. The determinants of PWV and augmentation index in the total population were identified by using Pearson's and Spearman's correlation coefficients for parametric and non-parametric variables accordingly. The independent determinants of PWVc-f and AIx in the total population were identified by using stepwise multiple linear regression analysis (dependent variables: PWVc-f or AIx; independent variables tested: age, gender, mean BP, body mass index, W/H, smoking status, total cholesterol, high-density lipoprotein, triglycerides, height, heart rate and homocysteine levels). The independent determinants of PWVc-f and AIx revealed by this analysis were used in two multiple linear regression models to assess the independent effect of the homocysteine levels on PWVc-f (model 1) and AIx (model 2) separately for each study group (NC, IOH and AH). Significance was assumed at a two-tailed probability value of <0.05.
Statistical analysis was performed using SPSS package for Windows version 13.0 (SPSS, Chicago, IL, USA).
Results
The baseline characteristics of the study population according to the office and ambulatory BPs are presented in Table 1. In the total population, both PWVc-f and AIx presented significant linear relations with age, male gender, smoking, peripheral systolic and diastolic BP, W/H ratio, smoking intensity assessed by pack years, total cholesterol, high-density lipoprotein and triglyceride levels (Table 2). PWVc-f was additionally correlated with body mass index and heart rate, which was not seen with AIx, whereas the latter was significantly associated with height (Table 2).
Finally, both PWVc-f and AIx were positively associated with the plasma homocysteine levels as shown in Table 2. In a stepwise multiple regression analysis, the plasma homocysteine levels remained a significant determinant of PWVc-f independent of the age, the mean BP, the W/H ratio and the high-density lipoprotein levels as shown in Table 3. In accordance, the stepwise multiple linear regression analysis also revealed an important association between homocysteine levels and AIx independent of other traditional factors affecting wave reflection, such as age, gender, smoking status, height, mean BP, body mass index, W/H ratio, heart rate and triglyceride levels (Table 3). These findings argue for a potential role of homocysteine in the remodelling of the arterial wall leading to arterial stiffness and enhanced wave reflection to the aorta.
When the three study groups were examined separately, homocysteine levels remained a significant independent determinant of PWVc-f in all groups as shown in Table 4. However, AIx was independently associated with the homocysteine levels in the groups of IOH and AH, but not in the NT group as shown in Table 4.
Discussion
The first finding of this study was that homocysteine is an independent determinant of large artery stiffness and wave reflections in the whole study cohort. This finding argues for a potential role of homocysteine in the remodelling of the arterial wall leading to arterial stiffness and enhanced wave reflection to the aorta. Earlier data suggest that homocysteine levels are associated with aortic stiffness in patients with type II diabetes mellitus.25 In another study,26 which involved health subjects, such an association between Hcy levels and arterial stiffness indices was not indicated, pointing to a clear controversy. The different results in the literature can be explained by the fact that hyperhomocysteinaemia may interact with other cardiovascular risk factors, namely, not only age and hypertension, but also smoking or diabetes mellitus.
The possible mechanisms of the relationship between Hcy and arterial stiffness are not yet fully well established. However, it is known that elevated Hcy levels induce oxidative injury to vascular endothelial cells and impair the production of nitric oxide, a strong relaxing factor by the endothelium.27, 28 Increased Hcy levels also enhance platelet adhesion to endothelial cells,29 promote proliferation of vascular smooth muscle cells30 and are associated with higher levels of prothrombotic factors, such as β-thromboglobulin, tissue plasminogen activator and factor VIIc.31 In addition, oral folate supplementation is seen to improve the arterial endothelium-dependent vascular function of the brachial artery in healthy subjects with mildly elevated levels of Hcy.32 Furthermore, patients with coronary artery disease and elevated Hcy, who were administered folate and vitamin B12, improved vascular endothelial function, as assessed by brachial artery flow-mediated dilatation.33
The second important finding of this study was that Hcy was an independent determinant of PWVc-f in healthy subjects as well as patients with isolate office hypertension and essential hypertension. It has been earlier analysed that serum Hcy levels enhance endothelial dysfunction. PWV is a known marker of arterial distensibility and endothelial function.34 Although investigators have reported a significant association between plasma Hcy with pulse pressure16 and arterial PWV in healthy subjects and patients with essential hypertension,17 no such reports exist for patients with IOH. To our knowledge, this is the first study reporting such an association in white coat hypertensive patients. Patients with IOH are reported to present with impaired arterial distensibility, compared with NTs, which entails a greater than normal cardiovascular risk.35 According to this study, Hcy levels pose an additive burden to the cardiovascular profile of patients with IOH, leading to large artery stiffening independently of other factors.
Finally, this study revealed an independent relationship of Hcy with AIx in patients with essential hypertension and IOH, but not with NTs. AIx is a measure of the contribution made by the reflected pressure wave to the ascending aortic pressure waveform,36 and thus provides a measure of systemic arterial stiffness.37 Therefore, these data show that Hcy levels are associated with systemic arterial stiffness. The fact that this relation was not noted in NT subjects may be explained by the fact that AIx is a marker mainly of small artery stiffness, and thus it can be assumed that Hcy does not affect the arterial wall of small arteries in subjects with the lack of additional risk factors. Furthermore, a number of factors such as gender, heart rate, height, smoking and lipidaemic profile are known to affect AIx values,38, 39 which was also confirmed by the present study results. It is possible that these factors affect small artery stiffness to a greater extent in NT patients than does Hcy. Finally, the small number of participants in the NTs group may have affected the results by underestimating the effect of Hcy on AIx.
There are some limitations in this study. First, patients with masked hypertension were not included, which could have led to interesting comparisons. Second, AIx measurement was made using the methodology from reconstructed waveforms using a transfer function, which has been criticized and may, therefore, not detect changes in stiffness in the small arteries. However, this is a large study cohort that leads to strong and valid conclusions.
In conclusion, in hypertensive patients, patients with IOH and NT subjects, there is a strong and positive correlation of increased Hcy levels with PWV. These results suggest that the evaluation of aortic distensibility and Hcy levels can help in cardiovascular risk assessment both in hypertensive subjects and patients with IOH as well as in NT subjects. The contribution of arterial stiffness and plasma Hcy measurements in risk assessment and risk reduction strategies in such populations needs to be confirmed by large prospective interventional and observational studies.

References
Boushey C, Beresford S, Omenn G, Motulsky A . A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA 1995; 274: 1049–1057.
Nygard O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE . Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med 1997; 337: 230–236.
Vollset SE, Refsum H, Tverdal A, Nygard O, Nordrehaug JE, Tell GS et al. Plasma total homocysteine and cardiovascular and non-cardiovascular mortality: the Hordaland Homocytseine Study. Am J Clin Nutr 2001; 74: 130–136.
Bots ML, Launer LJ, Lindemans J, Hoes AW, Hofman A, Witteman JC et al. Homocysteine and short-term risk of myocardial infraction and stroke in the elderly: the Rotterdam Study. Arch Intern Med 1999; 159: 38–44.
Bostom AG, Rosenberg IH, Silbershatz H, Jacques PF, Selhub J, D'Agostino RB et al. Nonfasting plasma total homocysteine levels and stroke incidence in elderly persons: the Framingham Study. Ann Intern Med 1999; 131: 352–355.
Vasan RS, Beiser A, D'Agostino RB, Levy D, Selhub J, Jacques PF et al. Plasma homocysteine and risk for congestive heart failure in adults without prior myocardial infraction. JAMA 2003; 289: 1251–1257.
Van de Bosch MA, Bloemenkamp DG, Mali WP, Kemmeren JM, Tanis BC, Algra A et al. Hyperhomocystenemia and risk for peripheral arterial occlusive disease in young women. J Vasc Surg 2003; 38: 772–778.
Malinow MR, Nieto FJ, Szklo M, Chambless LE, Bond G . Carotid artery intimalmedial wall thickening and plasma homocysteine in asymptomatic adults. Circulation 1993; 87: 1107–1113.
Selhub J, Jacques PF, Bostorn AG, D'Agostino RB, Wilson PWF, Belanger AJ et al. Association between plasma homocysteine concentrations and extra-cranial carotid artery stenosis. N Engl J Med 1995; 32: 218–220.
Montalescot G, Ankri A, Chadefaux-Vekenman B, Blacher J, Philippe F, Drobinski G et al. Plasma homocysteine and the extent of atherosclerosis in patients with coronary artery disease. Int J Cardiol 1997; 60: 295–300.
Welch GN, Loscalzo J . Homocysteine and atherotrombosis. N Engl J Med 1998; 338: 1042–1050.
Tawakol A, Omland T, Gerhard M, Wu JT, Greager MA . Hyperhomocysteinemia is associated with impaired endothelium-dependant vasodilatation in humans. Circulation 1997; 95: 1119–1121.
Charpiot P, Bescond A, Augier T, Chareyre C, Fraterno M, Rolland PH et al. Hyperhomocysteinemia induces elastolysis in minipig arteries: structural consequences, arterial site specificity and effect of captoril–hydroclorothiaszide. Matrix Biol 1998; 17: 559–574.
Graham IM, Daly LE, Refsum HM, Robinson K, Brattstorm LE, Ueland PM et al. Plasma homocysteine as a risk factor for vascular disease: the European Concerted Action Project. JAMA 1997; 227: 1775–1781.
Sutton-Tyrrell K, Bostorm A, Selbhub J, Zeigler-Johnson C . High homocysteine levels are independently related to isolated systolic hypertension in older adults. Circulation 1997; 96: 1745–1749.
Davis KR, Pearson H, Moat S, Bonham JR, Donnelly R . Acute hyperhomocysteinemia affects pulse pressure but not microvascular vasodilator function. Br J Clin Pharmacol 2001; 52: 327–332.
Blacher J, Demuth K, Guerin AP, Safar ME, Moatti N, London GM . Influence of biochemical alterations on arterial stiffness in patients with end-stage renal disease. Atheroscler Thromb Vasc Biol 1998; 18: 535–541.
Bortolotto LA, Safar ME, Billaud E, Lacroix C, Asmar R, London GM et al. Plasma homocysteine, arterial stiffness, and renal function in hypertensive patients. Hypertension 1999; 34: 837–842.
Nakhai-Pour HR, Grobbee DE, Bots ML, Muller M, van der Schouw YT . Circulating homocysteine and large arterial stiffness and thickness in a population-based sample of middle-aged and elderly men. J Hum Hypertens 2007; 21: 942–948.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. 2007 ESH-ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Cuspidi C, Meani S, Fusi V, Severgnini B, Valerio C, Catini E et al. Metabolic syndrome and target organ damage in untreated essential hypertensives. J Hypertens 2004; 22: 1991–1998.
Donnelly JG, Pronovost C . Evaluation of the Abbott IMx fluorescence polarization immunoassay and the Bio-Rad enzyme immunoassay for homocysteine: comparison with high-performance liquid chromatography. Ann Clin Biochem 2000; 37: 194–198.
Pannier BM, Avolio PA, Hoeks A, Mancia G, Takazawa K . Methods and devices for measuring arterial compliance in humans. Am J Hyperetns 2002; 15: 743–753.
O'Rourke MF, Staessen JA, Vlachopoulos CH, Duprez D, Plante GE . Clinical applications of arterial stiffness; definitions and reference values. Am J Hypertens 2002; 15: 426–444.
Anan F, Masaki T, Umeno Y, Yonemochi H, Eshima N, Saikawa T et al. Correlations between homocysteine levels and atherosclerosis in Japanese type 2 diabetic patients. Metab Clin Exp 2007; 56: 1390–1395.
De Bree A, Mennen LI, Zureik M, Ducros V, Guilland JC, Nicolas JP et al. Homocyctseine is not associated with arterial thickness and stiffness in healthy middle-aged French volunteers. Int J Cardiol 2006; 113: 332–340.
Cohen JA, Jeffers BW, Stabler S, Schrier RW, Estascio R . Increasing homocysteine levels and diabetic autonomic neuropathy. Auton Neurosci 2001; 87: 268–273.
Spoelstra-De Man AM, Smulders YM, Dekker JM, Heine RJ, Bouter LM, Nijpels G et al. Homocysteine levels are not associated with cardiovascular autonomic function in elderly Caucasian subjects without and with type 2 diabetes mellitus: Hoom study. J Intern Med 2005; 258: 536–543.
Mantysaari M, Kuikka J, Mustonen J, Tahvanainen K, Vanninen E, Länsimies E et al. Noninvasive detection of cardiac sympathetic nervous dysfunction in diabetic patients using [123I] metaiodobenzylguanidine. Diabetes 1992; 41: 1069–1075.
Schenll O, Muhr D, Weiss M, Kirsch CM, Haslbeck M, Tatsch K et al. Three years follow-up on scintigraphically assessed cardiac sympathetic denervation in patients with long-term insulin-dependent (type 1) diabetes mellitus. J Diabetes Complications 1997; 11: 307–313.
Weir DG, Scott JM . The biochemical basis of neuropathy in cobalamin deficiency. Bailliere's Clin Heamatol 1995; 8: 479–497.
Chowdhary S, Vaile JC, Fletcher J, Ross HF, Coote JH, Townend JN . Nitric oxide and cardiac autonomic control in humans. Hypertension 2000; 36: 264–269.
Davis JL, Band M, Morris A, Struthers AD . Spironolactone impairs endothelial dysfunction and heart rate variability in patients with type 2 diabetic. Diabetologica 2004; 47: 1687–1694.
Avolio AP, Chen SG, Wang RP, Zhang CL, Li MF, O'Rourke MF . Effects of aging on changing arterial compliance and left ventricular load in a northern Chinese urban community. Circulation 1983; 68: 50–58.
Wimmer NJ, Sathi K, Chen TL, Townsend RR, Cohen DL . Comparison of pulse wave analysis between persons with white coat hypertension and normotensive persons. J Clin Hypertens (Greenwich) 2007; 9: 513–517.
O'Rourke MF, Kelly RP . Wave reflection in the systemic circulation and its implications in ventricular function. J Hypertens 1993; 11: 327–337.
Safar ME, London GM . Therapeutic studies and arterial stiffness in hypertension: recommendations of the European Society of Hypertension. The Clinical Committee of Arterial Structure and Function. Working Group on Vascular Structure and Function of the European Society of Hypertension. J Hypertens 2000; 18: 1527–1535.
Hayward CS, Kelly RP . Gender-related differences in the central arterial pressure waveform. J Am Coll Cardiol 1997; 30: 1863–1871.
Wilkinson IB, MacCallum H, Flint L, Cockcroft JR, Newby DE, Webb DJ . The influence of heart rate on augmentation index and central arterial pressure in humans. J Physiol 2000; 525: 263–270.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Licence. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Vyssoulis, G., Karpanou, E., Kyvelou, SM. et al. Associations between plasma homocysteine levels, aortic stiffness and wave reflection in patients with arterial hypertension, isolated office hypertension and normotensive controls. J Hum Hypertens 24, 183–189 (2010). https://doi.org/10.1038/jhh.2009.50
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2009.50
Keywords
This article is cited by
-
C677T MTHFR Gene Polymorphism is Contributing Factor in Development of Renal Impairment in Young Hypertensive Patients
Indian Journal of Clinical Biochemistry (2021)
-
Interactions between plasma homocysteine and arterial stiffness in chronic kidney disease in community-dwelling individuals: The Maine-Syracuse Study
Journal of Human Hypertension (2015)