Abstract
Alström syndrome (ALMS) is an autosomal recessive disease characterized by multiple organ involvement, including neurosensory vision and hearing loss, childhood obesity, diabetes mellitus, cardiomyopathy, hypogonadism, and pulmonary, hepatic, renal failure and systemic fibrosis. Alström Syndrome is caused by mutations in ALMS1, and ALMS1 protein is thought to have a role in microtubule organization, intraflagellar transport, endosome recycling and cell cycle regulation. Here, we report extensive phenotypic and genetic analysis of a large cohort of Turkish patients with ALMS. We evaluated 61 Turkish patients, including 11 previously reported, for both clinical spectrum and mutations in ALMS1. To reveal the molecular diagnosis of the patients, different approaches were used in combination, a cohort of patients were screened by the gene array to detect the common mutations in ALMS1 gene, then in patients having any of the common ALMS1 mutations were subjected to direct DNA sequencing or next-generation sequencing for the screening of mutations in all coding regions of the gene. In total, 20 distinct disease-causing nucleotide changes in ALMS1 have been identified, eight of which are novel, thereby increasing the reported ALMS1 mutations by 6% (8/120). Five disease-causing variants were identified in more than one kindred, but most of the alleles were unique to each single patient and identified only once (16/20). So far, 16 mutations identified were specific to the Turkish population, and four have also been reported in other ethnicities. In addition, 49 variants of uncertain pathogenicity were noted, and four of these were very rare and probably or likely deleterious according to in silico mutation prediction analyses. ALMS has a relatively high incidence in Turkey and the present study shows that the ALMS1 mutations are largely heterogeneous; thus, these data from a particular population may provide a unique source for the identification of additional mutations underlying Alström Syndrome and contribute to genotype–phenotype correlation studies.
Similar content being viewed by others
Introduction
Alström syndrome (ALMS, MIM# 203800) is a recessively inherited genetic disorder caused by mutations in ALMS1.1,2 ALMS is characterized by a complex, progressive and variable clinical expression affecting nearly all organ systems.
Clinical signs typical in early childhood are cone–rod retinal dystrophy leading to blindness, sensorineural hearing loss, metabolic abnormalities and obesity. Dilated mitogenic cardiomyopathy occurs in approximately 70% of patients perinatally,3,4 and ALMS1 mutations are a significant cause of idiopathic mitogenic cardiomyopathy.5 In addition, restrictive cardiomyopathy with fibrosis and pulmonary hypertension can develop during adolescence or adulthood.3,4 Truncal obesity is a consistent feature, usually beginning in the first 6–18 months. The obesity increases during childhood but generally tends to moderate as the patient grows older. Insulin resistance and diabetes mellitus are observed in nearly all patients before the age of 20 years. Hepatic involvement begins with elevated transaminases and varying degrees of steatosis and inflammation. In a subset of patients, the disease progresses to overt cirrhosis and eventual hepatic failure. Additional presentations can include early developmental delay and learning difficulties, hypertension, hypertriglyceridemia, chronic otitis media, gastrointestinal reflux disease, short stature, scoliosis and pes planus. Male hypogonadism is common and females often present with hirsutism and menstrual irregularities. Kidney dysfunction begins slowly and is usually not seen before the age of 10 years. Increasing systemic fibrosis develops as patients age with clinical manifestations of multiple organ failure, including congestive heart failure, hepatic and end-stage renal disease, all of which are frequent causes of morbidity and mortality in patients.4
Differential diagnosis of ALMS can be challenging because of the gradual emergence of most of the cardinal features as well as some early clinical similarities to other genetic diseases, such as leber congenital amaurosis, idiopathic cardiomyopathy or Bardet–Biedl Syndrome (BBS).6
ALMS is caused by disruptions in ALMS1, which comprises 225 kb of genomic DNA, spanning 23 exons and encoding a predicted 461.2 kDa protein.1,2 ALMS1 is ubiquitously expressed in tissues that are pathologically affected in patients with ALMS.7 ALMS1 localizes to centrosomes and to basal bodies of ciliated cells, suggesting roles in centrosomal, intracellular and ciliary functions, and regulation of cell cycle, and other isoform-specific cellular functions have been shown.8, 9, 10, 11
To date, 120 unambiguous disease-causing mutations in ALMS1 have been reported in patients with ALMS. The majority of disease-causing alleles are nonsense and frameshift which would lead to premature protein truncation and are predicted to undergo nonsense-mediated decay of the corresponding mRNA.12, 13, 14 Exons 16, 10 and 8 account for 94% of the mutational load in families of European descent, with the remainder of the gene containing rare variants comprising 6%. Chromosomal translocations with a break point in ALMS1, AluYa5 elements inserted in ALMS1, and large deletions have also been reported in few patients.2,15,16
Our study provides a detailed description of the phenotypes of 61 patients from 44 Turkish kindreds. Disease-associated mutations, eight of which are novel, were identified in 41 of those for whom genomic DNA material was available.
Materials and methods
Sixty-seven patients of Turkish descent from 50 kindreds (33 males and 34 females), with a mean age of 15.3 years (range 3 to 38 weeks) were initially identified for the study. They were clinically diagnosed with ALMS through local hospitals and pediatric clinics throughout Turkey and Eastern and Western Europe. ALMS was diagnosed on the basis of the established age-dependent diagnostic criteria which require the presence of additional cardinal features as the patient grows older and additional manifestations develop.5 Medical records and clinical questionnaires were investigated irrespective of whether genetic analyses were available and included weight, height, cardiac, renal, hepatic, endocrine function and developmental issues. In order to compare all known Turkish patients with ALMS, we included eleven previously reported patients in this study. Two patients were excluded after subsequently receiving molecular diagnoses of BBS1 and BBS2, respectively. We excluded seven additional subjects (three male, four female) based upon an inappropriate phenotype, leaving a total of 50 patients for whom clinical data were collected and 11 case reports reviewed.
Patient data were collected from 2000 to 2013. When possible, patients and families were followed longitudinally and data were updated more than once during the course of the study. Because patients were evaluated at several different medical institutions, consistent clinical evaluations were not performed in a subset of patients.
Body mass index (BMI) was calculated using the following formula: Weight (in kilograms)/Height (in meters)2, kg m−2. The centers for disease control and prevention BMI-for-age tables were used to define BMI centiles for age (http://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm). For children 2–20 years of age, weight status category for age and gender was determined by these criteria: U: underweight (BMI <5%); N: normal weight (BMI 5–85%): O: Overweight (BMI 85–95%); OB: Obese (BMI >95%). For adults over 20 years, BMI was interpreted using standard weight status categories that are the same for both men and women: Underweight, BMI <18.5; Normal, BMI 18.5–24.9; Overweight, BMI 25–29.9; Obese BMI >30; 25 patients were previously reported.16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 Appropriate informed consent was obtained from all participants. Protocols were reviewed and approved by The Jackson Laboratory Institutional Review Board.
Mutation screening strategy
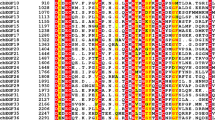
DNA, extracted from venous lymphocytes using standard protocols, was available from 30 kindreds with a presumed diagnosis of ALMS. We used the following algorithm for genetic diagnosis (Figure 1).
Mutation screening algorithm for genetic diagnosis of patients with the Alstrom Syndrome. Three different approaches were used for mutation detection; a cohort of patients were screened by the APEX array to detect the common mutations in the ALMS1 gene, then in patients without any of the mutations on the APEX array were subjected to direct-DNA sequencing or next-generation sequencing. A full color version of this figure is available at the Journal of Human Genetics online.
One subset of 16 kindreds was analyzed on an arrayed primer extension microarray to identify known ALMS1 mutations (Asper Ophthalmics; www.asperophthalmics.com).14 The test array contained 113 ALMS1 genetic variants, as well as BBS gene mutations BBS1, BBS2, BBS3, BBS4, BBS5, BBS6, BBS7, BBS8, BBS10, PHF6 (Borjeson–Forssman–Lehman syndrome) and GNAS1 (Albright hereditary osteodystrophy), including polymorphisms and variants of uncertain pathogenicity (See Supplementary Table S1 for positions screened on the Asper ophthalmics array).
A second subset of DNA from 14 kindreds was directly Sanger sequenced, likewise focusing on exons 16, 10 and 8 first. When both ALMS1 mutations were identified in these exons, the sequencing was stopped. If only one mutant allele found or none in exon 16, 10, 8, all exons were subjected to Sanger sequencing. After sequencing, the eight kindreds for whom no mutated alleles were identified were simultaneously sequenced with the targeted gene sequencing and custom analysis test.33 Briefly, samples were prepared for Illumina-based next generation sequencing (NGS) with standard methods, enriched twice by incubation with 20 477 capture probes targeting 8366 exons of 514 genes that correspond to 764 childhood genetic diseases.
Primers were designed for PCR amplification of all coding and splice site sequences of ALMS1. PCRs and amplification conditions were performed as previously described.1 Primer sequences are available from the authors upon request. Sequences were compared with ALMS1 (GenBank NM_015120.4; AC074008.5) using MacVector TM 7.2.3 (MacVector Cary, NC, USA). Nucleotide and amino-acid numbering of mutation sites began at the start codon, ATG (Met) of the open reading frame, originally described by Collin et al. and Hearn et al.1,2
A mutation was considered novel if it has not been described in the medical literature, or is not present in the Human Mutation Database (www.hgmd.cf.ac.uk/ac), the dbSNP database (www.ncbi.nlm.nih.gov/projects/SNP/index.html), the Exome Variant Server (http://evs.gs.washington.edu/EVS/), or the LOVD database (www.lovd.com).
To assess the pathogenicity of nonsynonymous-allelic variations, the bioinformatics prediction software programs PolyPhen-2 (Polymorphism Phenotyping v2: http://genetics.bwh.harvard.edu/pph2/dokuwiki/downloads) and sorting intolerant from tolerant ( http://sift.jcvi.org) were used, along with a minor allele frequency (MAF) score from the Exome Variant Server, National Heart Lung Blood Institute, Grand Opportunity Exome Sequencing Project, 6500 exomes, accessed 19/5/2014) (NHLBI GO ESP; evs.gs.washington.edu/). These tools predict possible impact of a nonsynonymous amino-acid substitution on the structure and function of a protein based on sequence homology, conservation of sequences and the physical properties of amino acids.34,35
Results
Clinical features and identified genotypes of the 61 patients enrolled in this study are summarized in Table 1. To our knowledge, 22 kindreds (48%) were born to consanguineous marriages, and 23 were either non-consanguineous or the family history was not known. All patients were of Turkish origin from different geographical regions of Turkey and Turkish immigrants living in Europe.
Clinical findings
Many of the features typical in ALMS display age-related penetrance. There is also a wide spectrum in severity of the disease phenotypes. Ten patients died before the age of 38 years, and their average age of death was 17 years.
Sensory loss
Retinal dystrophy within the first year was a consistent feature in our cohort, with the exception of four patients whose vision impairment was not noticed or reported until early childhood. Electroretinography was not always available for families from isolated locations. We observed hearing loss in 34 of the 47 patients over the age of 4 years, with an average age of onset of 7 years.
Obesity
Relatively mild obesity phenotypes are noted in this cohort of patients. We found that 14 (five males, nine females) out of 61 patients (age range 6–36 years) had normal weight (22.5%), and only one was morbidly obese (patient 39 with a BMI of 43.4 kg m−2). The average BMI was 27.3±5.9 (N=40).
Diabetes and endocrinological dysfunction
The youngest age of onset of diabetes was 6 years (patient 44). Of the 54 cases in our cohort 6 years and older, six were hyperinsulinemic or glucose intolerant, and 36 (66%) had diabetes. Endocrinological abnormalities included hypogonadotropic hypogonadism in males and menstrual irregularities and early puberty in females, short stature, advanced bone age, hypertriglyceridemia, hypothyroidism, hyperthyroidism and alopecia.
Although not assessed in all patients, growth hormone deficiency was reported in six patients (patients 12, 52, 53, 54, 57, 59).
Cardiopulmonary
Nineteen of the 61 (30%) patients in our cohort had cardiomyopathy. There were two siblings with mitral valve insufficiency (patients 17 and 18), one patient of patent foramen ovale (patient 12), and another patient with a systolic murmur (patient 59). Although not proven, the death of two young patients (patients 58 and 60) could likely be attributed to the infantile cardiomyopathy that is common in ALMS.3,5
Hepatic
Liver size and enzymes were increased in 35 of 61 (58%) of patients. These patients (patients 13, 22 and 61) had severe cirrhosis and portal hypertension with upper gastrointestinal bleeding.
Renal dysfunction
Patients aged 12 years or older were considered for renal involvement (n=41). Fifteen showed functional abnormalities in the renal system, which included proteinuria, renal calculi, hyperuricemia, pelviectasis and microalbuminuria. Two patients presented with renal disease earlier than typical in ALMS: One (patient 40) presented with chronic renal insufficiency at age 2 months, and another (patient 28) had severe end-stage renal failure at age 5 years, and subsequently died with multiple organ failure.
Neurological findings
Neurological symptoms in 18/61 (29%) patients included mild ataxia, hypotonia, poor balance or febrile and afebrile seizures. Four patients (patients 12, 13, 26 and 27) had microcepahaly, cortical atrophy, or abnormalities observed in MRI, and another (patient 59) had cerebral hemiatrophy.
Psychomotor development and intelligence
Cognitive deficits and motor impairment was documented in half of the patients (32/61). These represented a range of developmental issues from severe-to-milder cognitive impairments, gross and fine motor delay, language delay, attention deficit disorder and autistic spectrum behavior. Of those 30 analyzed for genetic mutations, 18 presented with some degree of cognitive impairment. Array comparative genomic hybridization (CGH) to detect copy number variations has not been carried out on these patient’s DNA samples.
Other clinical manifestations
The results of our study confirm that pulmonary dysfunction (16 patients), short stature/scoliosis (16 patients), hypertension (eight patients) and urological symptoms (seven patients) are very frequent medical complications in Turkish patients with ALMS.
There were no significant differences in vision, hearing loss, obesity, cardiomyopathy, liver and renal function, and developmental delay between patients in whom disease-causing mutations were identified and in those who had not received a molecular confirmation.
Mutation screening and DNA sequencing results
In total, 30 kindreds with a phenotypic diagnosis of ALMS were screened for ALMS1 mutations. Of the 16 kindreds analyzed using the asper ophthalmics array, homozygous disease-causing mutations were identified in three, and 13 were negative for any ALMS1 mutations on the array. DNA from those 13 negative kindreds was then Sanger sequenced, focusing on exons 16, 10 and 8 first, and then if no mutations were found, sequencing the remaining exons. In seven kindreds both ALMS1 mutated alleles were identified and one heterozygous mutated allele was identified in one kindred. In five kindreds from this cohort, we were not able to identify any disease-causing ALMS1 mutations.
DNA from another cohort of 14 patients was not submitted to the asper ophthalmics array, but Sanger sequenced directly. In this cohort of 14, both ALMS1 mutated alleles were identified in nine kindreds and one mutated allele identified in two kindreds. Using both methods, 16 of 30 had homozygous ALMS1 mutations and in three, only one heterozygous mutation was identified.
In these eight kindreds, exomes were then evaluated by high-throughput sequencing, and in three of eight homozygous ALMS1 mutations were detected.
Therefore, with the three methods combined, 19 kindreds had homozygous mutations, in three kindreds, only one deleterious allele was identified. In eight of our kindreds, no mutations were found.
Eight novel and 12 previously reported12,16,23,27,28,31,36 mutations were identified in exons 8, 10, 11, 16 and intron 18 in 25 kindreds (Tables 1 and 2).
Ten were nonsense mutations, nine were frameshift mutations, and one intronic splice site mutation identified which was previously reported to be pathogenic.36
Five mutations were seen in more than one of apparently unrelated kindreds: c.4156insA; p.Thr1386AsnfsX15 (two kindreds), c.5311C>T; p.Gln1769* (two kindreds), c.5969C>G; p.Ser1990* (three kindreds) and c.11870-3T>G (two kindreds). In addition, we identified c.8506G>T; p.Glu2836* in three kindreds from the Konya that were not knowingly related to each other (kindred 14, 15, 16), suggesting an early founder effect in that region.
Interestingly, kindred 6, residing in a rural village outside of İnebolu, Kastamonu, is comprised of three siblings heterozygous for c.5311C>T; p.Gln1769* in exon 8 and c.10563_10564delTA; p.His3521Glnfs*16 in exon 16. Their first cousin, also affected, carried p.Gln1769* in homozygous state. The remaining mutations were only identified in one kindred each, ruling out potential founder effects.
Three kindreds (kindreds 7, 10, 19) harbored three mutated alleles. Patient 10 (kindred 7), homozygous for p.Tyr1862*, also carried a third deleterious allele, p.Leu968fs*4.30 Patient 13 (kindred 10) was homozygous for a splice site mutation c.11870-3T>G while carrying a third ALMS1 stop mutation, p.Ser1990* in exon 8. Finally, as we described previously, patient 27 (kindred 19) is homozygous for p.Ser3250* and also carries a heterozygous intronic mutation IVS19-8delT.27
An intriguing observation was that in three kindreds (kindred 1, 12, 13) only one heterozygous mutation was identified, no other potentially deleterious alterations were found, despite extensive molecular sequencing of the coding regions. However, 49 variants of uncertain pathogenicity were identified in 44 kindreds (31 nonsynonymous, 13 synonymous, one deletion and four intronic nucleotide changes). Nonsynonymous variations were evaluated using two different in silico protein prediction programs (PolyPhen-2; and sorting intolerant from tolerant); and their minor allele frequencies are reported in Supplementary Table S2. We consider the variations which have <1% MAF and were predicted damaging from both PolyPhen and sorting intolerant from tolerant, as most probably deleterious allelic variations.
Based on their rarity and in silico prediction results, four novel variations (p.Asp505Asn, p.Ser764Phe, p.Asp3295Tyr, p.Asn3306Ser), might be deleterious and contribute to the patients’ phenotype. An amino-acid change p.Asp505Asn, predicted to be damaging and not seen before in controls, was detected in patient 33 who is also homozygous for p.Ile773Phefs*13. Likewise, p.Ser764Phe (MAF 0.008%) was identified in patient 12 who harbored one deleterious heterozygous mutation, p.Ser1990*. No nonsense or frameshift mutations were detected in kindreds 24 and 25. However, two patients from kindred 24 were homozygous for a rare variation, p.Asn3306Ser (MAF 0.3%) and patient 36 (kindred 25) was homozygous for novel missense variation, p.Asp3295Tyr. These results lend support to the notion that these rare allelic variations most probably contribute or drive the disease phenotype of the patients in these families. As the high degree of variation within ALMS1, further functional studies will be required to determine the potential pathogenicity of these variants.
There were 13 synonymous variants, of which c.2764C>A (rs143885319) was the most common, carried by 36% of the families (MAF 49.5% in EVS). A 5′ splice site variant c.767+20T>A (rs1881246) was also seen in five families, p.Arg4031Lys (rs1320374) whose MAF is 46.3%, is the most common nonsynonymous allele in the cohort (Supplementary Table S2 shows nonsynonymous and synonymous alterations observed).
Discussion
In this study, we review clinical phenotypes in a large series of 61 Turkish patients with ALMS. We report eight novel ALMS1 mutations and four additional nonsynonymous rare alleles that could be potentially disease-associated variants.
ALMS has an estimated prevalence of <1:1 000 000 in Europe and North America,13 with the frequency higher in geographically or culturally isolated populations where consanguinity is more common, a well-established phenomenon. However, genetic homogeneity and founder effects in this study population clearly cannot be invoked as plausible explanations for the high incidence of ALMS in Turkey, as 20 different ALMS1 mutations have been identified so far in Turkish patients. This implies that ALMS in Turkey is likely a result of multiple isolates rather than being attributable to a single founder.
Located between Europe and Asia, Anatolia served as a gateway for various ethnicities, which may contribute to form a diverse and a unique genetic background. Hence, finding a wide variety of different allelic variations and deleterious mutations is not surprising. It is notable that four of the most common ALMS1 mutations in the world population13 (10775delC, c.10483delC, 11316_11319delAGAG and c.11449C>T), are absent in the Turkish cohort. Conversely, 80% of the variants found in Turkish kindred’s have not been seen in other ethnicities, which emphasizes the population specificity of some ALMS1 mutations, and has potential diagnostic implications.
Previous reports have shown ‘hot spots’ for deleterious mutations in exon 16 (41%), exon 10 (27%) and exon 8 (25%).12,13 Although 97% of the pathogenic alleles in this cohort are clustered in the ‘hot spots’, in our cohort, there were more than expected in exon 8 (40%) and 10 (32%), and fewer than expected (25%) in exon 16 and no missense variants or single-nucleotide polymorphisms were detected in these exons in any of our patients.
Consanguinity is reported in only a minority of patients of European origin, but founder effects have been suggested in the Acadian population in Nova Scotia37 and in a UK cohort.12 In the Turkish population, with an estimated population of 81 619 392 (www.cia.gov, July 2014), the consanguinity rate is estimated to be between 20 and 25%38 and it is not currently feasible to accurately determine the prevalence of ALMS.
Another possible reason is that the clinical diagnostic criteria of this disorder are not always well-known to the clinicians. In addition, the emerging phenotype as the child grows poses a diagnostic challenge for pediatricians. Therefore, many affected individuals likely remain undiagnosed.
Including this study, there are 120 predicted disease-causing ALMS1 mutations reported to date in patients of diverse ethnic and national origins.13 The mutation detection rate is relatively low, as 5/31 patients whose coding regions were sequenced had no mutations identified. It is possible, indeed likely given their clinical presentation that a mutation exists in the intronic regions but was not detected. We cannot exclude cryptic splicing mutations, which can be very difficult to identify on direct-DNA sequencing. Further, the possibility that some of the additional missense variants we identified are pathogenic that cannot be excluded. Finally, allelic variations which may modify or interact with ALMS1 require further investigation. Therefore, future genetic studies of the disease should consider the next-generation sequencing approach which allows us to see all variations of the genome or exome of an individual.
Genotype–phenotype correlation
The ALMS phenotype is highly variable within and between families but, at this time, there are few studies presenting any genotype–phenotype correlation. Although variable expressivity has been reported widely, the clinical manifestations between our nine sets of siblings were very similar. There were seven patients who had both mutated alleles in exon 8, four patients with both mutations in exon 10, and one patient with both mutations in exon 11. Although the numbers are small, there were no significant differences in clinical course between patients with homozygous mutations in a specific exon and different biallelic ALMS1 mutations located in two different exons.
ALMS1 which spans 225 kb is a large and repetitive gene and the mutational load is quite high, especially combined with the high prevalence of consanguineous marriages in Turkey. Therefore, it is not surprising that we detect more allelic variations in the population. In this light, we might explain the patients (patients 10, 13, 29) who harbor three different deleterious variations in the ALMS1 gene. However, the phenotypes of the three patients did not differ from the other patients for whom one or two alleles were found. Furthermore, their presence did not correlate with increasing disease severity as estimated by the number of primary or secondary features of the disease. Therefore, it is hard to predict the effect of the third allele on the protein without functionally testing the alleles together. As DNA samples of parents were not available, we could not show segregation of the variations within the family.
Although most of the phenotypic manifestations that are present in our cohort did not differ from the classical features, we want to emphasize that the characteristics of pulmonary dysfunction, urological dysfunction and neurological abnormalities are frequent in this group of patients.
This is the first comprehensive study of ALMS in Turkey. We estimate that ALMS is under-reported in this population. Most patients with Alström Syndrome manifest classic features that could lead to a diagnosis in early childhood. Although a great effort was made to identify and include all known patients in Turkey, it is likely that many individuals with ALMS remain unidentified. Many families have limited contact with the health-care system, and single sporadic patients are often missed. Earlier and more accurate clinical diagnosis will improve patient care and monitoring, and will present an opportunity to uncover novel disease-causing mutations in ALMS1.
Change history
26 January 2015
This article has been corrected since Advance Online Publication, and a corrigendum is also printed in this issue.
References
Collin GB, Marshall JD, Ikeda A, So WV, Russell-Eggitt I, Maffei P et al. Mutations in ALMS1 cause obesity, type 2 diabetes and neurosensory degeneration in Alström syndrome. Nat. Genet. 2002; 31: 74–78.
Hearn T, Renforth GL, Spalluto C, Hanley NA, Piper K, Brickwood S et al. Mutation of ALMS1, a large gene with a tandem repeat encoding 47 amino acids, causes Alström syndrome. Nat. Genet. 2002; 31: 79–83.
Marshall JD, Bronson RT, Collin GB, Nordstrom AD, Maffei P, Paisey RB et al. New Alström syndrome phenotypes based on the evaluation of 182 cases. Arch. Intern. Med. 2005; 165: 675–683.
Marshall JD, Maffei P, Beck S, Barrett TG, Paisey RB Clinical utility gene card for: Alström syndrome. Eur. J. Hum. Genet. 2011; 19: e1–e3.
Shenje LT, Andersen P, Halushka MK, Lui C, Fernandez L, Collin GB et al. Mutations in Alström protein impair terminal differentiation of cardiomyocytes. Nat. Commun. 2014; 4: 3416.
Marshall JD, Beck S, Maffei P, Naggert JK Alström Syndrome. Eur. J. Hum. Genet. 2007; 15: 1193–1202.
Collin GB, Cyr E, Bronson R, Marshall JD, Gifford EJ, Hicks W et al. Alms1-disrupted mice recapitulate human Alström syndrome. Hum. Mol. Genet. 2005; 14: 2323–2333.
Hearn T, Spalluto C, Phillips VJ, Renforth GL, Copin N, Hanley NA et al. Subcellular localization of ALMS1 supports involvement of centrosome and basal body dysfunction in the pathogenesis of obesity, insulin resistance, and type 2 diabetes. Diabetes 2005; 54: 1581–1587.
Knorz VJ, Spalluto C, Lessard M, Purvis TL, Adigun FF, Collin GB et al. Centriolar association of ALMS1 and likely centrosomal functions of the ALMS motif-containing proteins C10orf90 and KIAA1731. Mol. Biol. Cell. 2010; 21: 3617–3629.
Zulato E, Favaretto F, Veronese C, Campanaro S, Marshall JD, Romano S et al. ALMS1-deficient fibroblasts over-express extra-cellular matrix components, display cell cycle delay and are resistant to apoptosis. PLoS ONE 2011; 6: e19081.
Collin GB, Marshall JD, King BL, Milan G, Maffei P, Jagger DJ et al. The Alström syndrome protein, ALMS1, interacts with α-actinin and components of the endosome recycling pathway. PLoS ONE 2012; 7: e37925.
Marshall JD, Hinman EG, Collin GB, Beck S, Cerqueira R, Maffei P et al. Spectrum of ALMS1 variants and evaluation of genotype-phenotype correlations in Alström syndrome. Hum. Mutat. 2007; 28: 1114–1123.
Marshall JD, Maffei P, Collin GB, Naggert JK Alström syndrome: genetics and clinical overview. Curr. Genomics 2011; 12: 225–235.
Pereiro I, Hoskins BE, Marshall JD, Collin GB, Naggert JK, Piñeiro-Gallego T et al. Arrayed primer extension (APEX) technology simplifies mutation detection in BardetBiedl and Alström Syndrome. Eur. J. Hum. Genet. 2011; 19: 485–488.
Bond J, Flintoff K, Higgins J, Scott S, Bennet C, Parsons J et al. The importance of seeking ALMS1 mutations in infants with dilated cardiomyopathy. J. Med. Genet. 2005; 42: e10.
Taşkesen M, Collin GB, Evsikov AV, Güzel A, Özgül RK, Marshall JD et al. Novel Alu retrotransposon insertion leading to Alström syndrome. Hum. Genet. 2012; 13: 407–413.
Zumsteg U, Muller PY, Miserez AR Alström Syndrome: confirmation of linkage to chromosome 2p 12-13 and phenotypic heterogeneity in three affected sibs. J. Med. Genet. 2000; 37: e8.
Koray F, Corter C, Benderli Y, Satman I, Yilmaz T, Dinccag N et al. Alström syndrome: a casereport. J. Oral. sci. 2001; 43: 221–224.
Satman İ, Yilmaz MT, Gürsoy N, Karşıdağ K, Dinççağ N, Ovalı T et al. Evaluation of insulin resistant diabetes mellitus in Alström syndrome: a long-term prospective follow-up of three siblings. Diabetes Res. Clin. Pract. 2002; 56: 189–196.
Uçar T, Berberoğlu M, Öcal G, Evliyaoğlu O, Adıyaman P, Aycan Z et al. Metabolic, endocrine and clinical findings in a case with Alström Syndrome. J. Ankara Med. School 2003; 25: 143–148.
Koc E, Bayrak G, Suher M, Ensari C, Aktas D, Ensari A Rare case of Alström syndrome without obesity and with short stature, diagnosed in adulthood. Nephrology 2006; 11: 81–84.
Yılmaz C, Çaksen H, Yılmaz N, Güven AS, Arslan D, Cesur Y Alström syndrome associated with cerebral involvement: an unusual presentation. Eur. J. Gen. Med. 2006; 3: 32–34.
Özgül RK, Satman İ, Collin GB, Hinman EG, Marshall JD, Kocaman O et al. Molecular analysis and long-term clinical evaluation of three siblings with Alström Syndrome. Clin. Genet. 2007; 72: 351–356.
Ünlü C, Üstün İ, Akay F, Doğan U A rare cause of dilated cardiomyopathy; Alström syndrome. Anadolu Kardiyol. Derg. 2008; 8: 316–317.
Pirgon Ö, Atabek ME, Tanju IA Metabolic syndrome features presenting in early childhood in Alström syndrome: a case report. J. Clin. Res. Pediatr. Endocrinol. 2009; 1: 278–280.
Akdeniz N, Bilgili SG, Aktar S, Yuca S, Calka O, Kılıç A et al. Alström syndrome with acanthosisnigricans: a case report and literature review. Genet. Couns. 2011; 22: 393–400.
Taşdemir Ş, Güzel-Ozantürk A, Marshall JD, Collin GB, Özgül RK, Narin N et al. Atypical presentation and a novel mutation in ALMS1: implications for clinical and molecular diagnostic strategies for Alström syndrome. Clin. Genet. 2012; 83: 96–98.
Redin C, Le Gras S, Mhamdi O, Geoffroy V, Stoetzel C, Vincent MC et al. Targeted high-throughput sequencing for diagnosis of genetically heterogeneous diseases: efficient mutation detection in Bardet-Biedl and Alström Syndromes. J. Med. Genet. 2012; 49: 502–512.
Çakmak E, Acıbucu DO, Yonem O, Ataseven H A rare cause of bleeding esophageal varices: Alström syndrome. Clin. Res. Hepatol. Gastroenterol. 2012; 36: e106–107.
Kaya A, Orbak Z, Çayır A, Döneray H, Taşdemir S, Ozanturk A et al. Combined occurrence of Alström syndrome and bronchiectasis. Pediatrics 2014; 133: e780.
Bıyık M, Uçar R, Güngör G, Çakır Ö, Esen H, Aksan S et al. Alström Syndrome with liver cirrhosis: first case from Turkey. Turk. J. Gastroenterol. 2013; 24: 546–548.
Holder M, Hecker W, Gilli G Impaired glucose tolerance leads to delayed diagnosis of Alström Syndrome. Diabetes Care 1995; 18: 698–700.
Kingsmore SF, Dinwiddie DL, Miller NA, Soden SE, Saunders CJ For the Children’s Mercy Genomic Medicine Team Adopting orphans: comprehensive genetic testing of Mendelian diseases of childhood by next-generation sequencing. Expert Rev. Mol. Diagn. 2011; 11: 855–868.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P et al. A method and server for predicting damaging missense mutations. Nature Met. 2010; 7: 248–249.
Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC . SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012; 40(Web server issue) W452–W457.
Sanyoura M, Woudstra C, Halaby G A novel ALMS1 splice mutation in a non-obese juvenile-onset insulin-dependent syndromic diabetic patient. Eur. J. Hum. Genet. 2013; 22: 140–143.
Marshall JD, Ludman MD, Shea SE, Salisbury SR, LaRoche R, Willi SM et al. Genealogy, natural history, and phenotype of Alström syndrome in a large acadian kindred and three additional families. Am. J. Med. Genet. 1997; 73: 150–161.
Tunçbilek E Clinical outcomes of consanguineous marriages in Turkey. Turk. J. Pediatr. 2001; 43: 277–279.
Acknowledgements
We are grateful to Alström Syndrome International and Nevin Bengür, Alström Syndrome-Canada, Alström Sendromu Derneği Turkey. We are grateful to A Düfke, A Kiraz, F Sılan, H Önal, JR Lupski, N Narin, Ö Çogulu, S Günis-Bilgili, Ş Taşdemir, T Uçar, Y Seçkin, and many physicians who referred their patients for this study. This study was supported, in part, by NIH HD036878 (JKN, JDM, GBC), DPT 1206400603 and TÜBİTAK, 111S217, Turkey (AO and RKO).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Ozantürk, A., Marshall, J., Collin, G. et al. The phenotypic and molecular genetic spectrum of Alström syndrome in 44 Turkish kindreds and a literature review of Alström syndrome in Turkey. J Hum Genet 60, 1–9 (2015). https://doi.org/10.1038/jhg.2014.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.85
This article is cited by
-
Mutation identification and prediction for severe cardiomyopathy in Alström syndrome, and review of the literature for cardiomyopathy
Orphanet Journal of Rare Diseases (2022)
-
Consensus clinical management guidelines for Alström syndrome
Orphanet Journal of Rare Diseases (2020)
-
A case report of two siblings with Alstrom syndrome without hearing loss associated with two new ALMS1 variants
BMC Ophthalmology (2019)
-
ALMS1 and Alström syndrome: a recessive form of metabolic, neurosensory and cardiac deficits
Journal of Molecular Medicine (2019)
-
Rare coding variants and X-linked loci associated with age at menarche
Nature Communications (2015)