Abstract
Various studies on association of glutathione S-transferase (GST) polymorphisms and childhood acute lymphoblastic leukemia (ALL) have yielded conflicting results. We examined this association among north Indian children and conducted an updated meta-analysis to overcome sample size-related limitations. GSTM1, GSTP1 and GSTT1 genotypes in 100 children with ALL and 300 healthy controls were compared. GSTT1 null mutation (odds ratio (OR) 2.54, 95% confidence interval (CI) 1.50–4.32) and GSTP1 homozygous mutation (OR 3.13, 95%CI 1.48–6.59) were found to increase the risk of childhood ALL, while GSTM1 did not alter the risk. Meta-analysis included 22, 10 and 20 studies examining the association of childhood ALL with GSTM1, GSTP1 and GSTT1 genotypes, respectively. Only GSTM1 genotype (OR 1.29, 95%CI 1.10–1.62) was associated with increased risk in the overall analysis. However, both GSTM1 (OR 1.54, 95%CI 1.12–2.10) and GSTT1 (OR 1.63, 95%CI 1.32–1.99) null genotypes were associated with increased risk in Asian subjects. The risk of developing childhood ALL was not associated with GSTP1 genotype.
Similar content being viewed by others
Introduction
Childhood acute lymphoblastic leukemia (ALL), the most common pediatric cancer has been conventionally regarded to be the result of a complex gene-environment interplay.1 Environmental factors encompass exposure to various biological, physical and chemical agents and the differences in individual ability to handle these mutagens and carcinogens may be responsible for individual variation in susceptibility to cancer.2 Children are vulnerable to environmental toxins more than adults because of their relatively greater exposure, immature metabolism and higher levels of cell division and growth.2, 3 Existence of an effective detoxifying enzyme system helps in the metabolism of potentially harmful environmental toxins to inactive metabolites thereby imparting protection from development of cancer.3
Glutathione S-transferase (GST) M1, P1 and T1 are phase II enzymes involved in metabolism and detoxification of reactive oxygen species, xenobiotics and carcinogens.4 Genetic variation in this gene family have been associated with increased susceptibility to certain primary as well as chemotherapy-induced second cancers.4, 5 The genes encoding the enzymes GSTM1, GSTP1 and GSTT1 are polymorphic, and polymorphisms in these genes lead to decreased activity of the corresponding enzymes leading to increased susceptibility to environmental as well as other toxins.6 Null mutations in GSTM1 and GSTT1 lead to loss in the corresponding enzyme activity6 whereas 1578 A>G transition leads to reduction in GSTP1 activity.3
The association of GST polymorphisms and childhood ALL was reported in 1997 for the first time,7 which led a number of subsequent investigators to examine the association and arrive at conflicting results. Previous studies from India studying this association also reached different conclusions. The present study is the fifth case–control study from India8, 9, 10, 11 and first from the northern region of the Indian subcontinent. Rest of the studies are from southern part of India which has a different genetic pool compared with the north.12, 13 We also reviewed the previously published studies14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 (between 1997 and January 2014) and performed a meta-analysis examining the association of GST gene variation and susceptibility to childhood ALL.
Materials and methods
All children between 1 and 15 years of age, diagnosed as ALL in the pediatric hematology-oncology unit of King George’s Medical University, Lucknow, Uttar Pradesh, India from July 2011 till June 2013 were taken as cases. Controls were normal healthy adults (between 18 and 40 years of age) without any history of malignancy or other known disease. The study was performed in accordance with the ethical standards laid down by the Declaration of Helsinki, and all persons/parents of the children with ALL involved gave their informed consent before the inclusion in the study. The study was approved by the ethics committees of King George’s Medical University, Lucknow, Uttar Pradesh, India and Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
Five milliliters of peripheral blood samples was collected in EDTA-coated vials and stored at −20 °C until use. Genomic DNA was obtained using QIAamp DNA mini kit; Qiagen, Hilden, Germany.
Genotype analysis
Genotype analyses of GSTP1 were performed based on the restriction digestion of PCR-amplified products whereas those of GSTM1 and GSTT1 were performed in duplex PCR systems based on primers and reaction conditions as per Supplementary Table S1. In each reaction, 50 ng of genomic DNA was amplified in 10 ml of PCR buffer (67 mM Tris-HCl, pH 8.8, 16 mM (NH4)2SO4, 2 mM MgCl2, 0.01% Tween-20, 100 mM dNTPs) containing 0.5 U of Taq DNA polymerase. All reactions were conducted in an oil-free thermal cycler (PTC 200 Thermal Cyclers; Bio-Rad Laboratories Inc., Hercules, CA, USA) The amplification products were electrophoresed on 2% agarose gels containing ethidium bromide with a migrating distance of ∼3 cm, and the product bands were visualized under ultraviolet light. The presence of functional GSTT1 and GSTM1 genes was determined by a band of the expected size. Individuals were determined null for a GSTT1 or GSTM1 gene when a band of the expected size was absent in the presence of the positive internal control band. Variant alleles of GSTP1 were characterized by a gain of restriction site upon digestion with restriction enzyme Alw261.
Meta-analysis
Search strategy
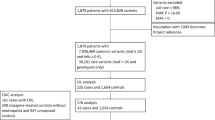
Pubmed and Medline databases were searched using search terms ‘GSTM1’or ‘GSTP1’ or ‘GSTT1’ and ‘childhood/ p(a)ediatric’ and ‘acute lymphoblastic leukemia’ and/or ‘acute leukemia’. Google Scholar was also searched to identify publications in un-indexed locations. The last date of search was 31 January 2014. We also searched the previously published meta-analyses to identify relevant studies. The references of the published meta-analyses as well as the case–control studies were hand-searched to identify more studies. The details of the search results are depicted in Figure 1.
Inclusion and exclusion criteria
We included studies published in English language, had a case–control design, with children with ALL as the cases and individuals without any history of malignancy as the controls and with sufficient accessible data required to calculate the effect size of the polymorphisms. All related studies not in case–control design (for example, case series, cohort studies without a control group and family-based studies) were excluded. Studies dealing with leukemia other than the de novo ones were also excluded. Studies reporting on more than one ethnicity were considered as separate studies if data on different ethnicities were presented separately. Studies reporting on the associations of GST polymorphisms with different forms of leukemia (for example, ALL, AML and ANLL) were included only if the data related to ALL could be separately retrieved. The reporting quality of the studies was assessed by the quality control, validity of genotyping technique, number of cases and controls in each genotype and conformity of the control groups to Hardy–Weinberg equilibrium.
Data extraction
Data extraction was done after two different investigators (NRM and FP) independently reviewed the abstracts followed by the full texts of relevant studies, any difference in opinion was sorted out upon mutual discussion. The following data were extracted from the studies: first author, year of publication, ethnicity and country, number of cases and control subjects. The frequencies of the allele and the genotypic distributions were extracted (if not available, the allele frequencies were calculated from genotypes), for both the cases and the controls.
Statistical analysis
Allele and genotype frequency differences were tested between patients and controls by means of two-sided Fisher’s exact test with Bonferroni correction. The magnitude of the effect was estimated by odds ratio (OR) and its 95% confidence interval (CI). Statistical analysis was performed by using SPSS version 20.0 for Windows (Statistical Package for Social Sciences, SPSS Inc., Chicago, IL, USA). Yates correction was applied wherever required. Allele and genotype frequencies and heterozygosities were tested for Hardy–Weinberg equilibrium via a 1 degree-of-freedom χ2 goodness-of-fit by using the software PopGen v 16 (http://www.ualberta.ca/_fyeh/fyeh). A binary logistic regression was carried out to examine the effect of the individual genes on the risk of childhood ALL.
The meta-analysis was carried out using the MetaAnalyst v2.0 (http://tuftscaes.org/meta_analyst) software based on bivariate and random-effect models. The risk of ALL associated with the GSTM1, GSTT1 and GSTP1 polymorphisms was evaluated by OR, risk ratio and risk difference with corresponding 95% CIs under allele contrast, dominant and the recessive models (for GSTP1 gene). The heterogeneity between studies was assessed using the I2 value along with Cochrane Q statistic. A P-value of <0.10 was taken as significant for assessing heterogeneity. We chose to perform the random-effect OR for all the models to provide a conservative estimate of the overall effect size. The forest plots were drawn with the use of ORs. The studies were also sub-grouped according to the ethnicity into three groups namely the Whites, the Blacks and the Asians.
Results
One hundred cases of childhood ALL (B-ALL 82 and T-ALL 18) with a mean age of 6.5±2.8 years (range 1–15 years) with a male to female ratio of 5:1 and three hundred population-based controls with a mean age of 23±6.7 years (range 18–40 years) with a male to female ratio of 4.6:1 included according to the inclusion and exclusion criteria were enrolled in this study. Frequency distributions of the GSTM1, GSTT1 and GSTP1 genotypes among the cases and control groups are presented in Table 1.
GSTM1 null mutation was not associated with increased risk of ALL (OR 1.38, 95%CI 0.85–2.24) whereas GSTT1 null mutation contributed to a significantly higher risk (OR 2.54, 95%CI 1.50–4.32) of ALL in the study children.
The presence of homozygous mutation in GSTP1 gene was also associated with a significantly higher risk of childhood ALL in our patients (OR 3.13, 95%CI 1.48–6.59), similarly mutant G allele increased the risk for ALL when compared with the wild A allele (OR 1.62, 95%CI 1.12–2.33).
Upon combined genotypic analysis of GSTM1 and GSTT1, the simultaneous presence of both the genes imparted protection (OR 0.54, 95%CI 0.34–0.86) whereas null mutation in both the genes was associated with a high risk (OR 3.59, 95%CI 1.41–9.11) of ALL.
Similarly, on combined genotypic analysis of GSTM1 and GSTP1, an increased risk (OR 2.29, 95%CI 1.15–4.54) was associated in children with combined GSTM1 null mutation and GSTP1 variant (AG or GG) genotype. The presence of GSTT1 gene and GSTP1 wild genotype was protective (OR 0.44, 95%CI 0.27–0.71) while GSTT1 null genotype in combination with GSTP1 mutated (AG or GG) genotypes was associated with increased risk (OR 2.24, 95%CI 1.26–3.98) of childhood ALL.
When all the three genotypes were combined, protection against ALL was observed in individuals with combined presence of GSTT1, GSTM1 and wild GSTP1 genotypes (OR 0.50, 95%CI 0.29–0.85) while a significantly higher risk (OR 1.97, 95%CI 1.05–3.73) of ALL was observed in children with combined GSTT1 null/GSTM1 null/GSTP1 variant genotype.
The independent effects of the various genotypes on the risk of childhood ALL are presented in Table 2. Significantly increased risk was found with GSTT1 (OR 3.06, 95%CI 1.75–5.32) and GSTP1 (OR 1.75 95%CI 1.23–2.51) mutation while GSTM1 (OR 1.55, 95%CI 0.94–2.56) mutation was unassociated with the risk of developing ALL.
Meta-analysis
The detailed search strategies and results obtained thereof are summarized in a flow diagram (Figure 1). The genotypic distributions for all the three GST genes in the studies included are presented in Supplementary Table S2.
GSTM1
In total, 22 studies (11 on Whites, 9 on Asians and 2 on Blacks) comprising 3311 cases and 4903 controls were analyzed for the association of GSTM1 mutation and childhood ALL. The effect size was measured as the susceptibility of GSTM1 null variant as compared with the wild (present) variant. Between-study heterogeneity was observed to be high (62%), hence random-effect OR was used to measure the effect size. Funnel plot did not reveal any obvious asymmetry. In the overall analysis, a significant association between GSTM1 null genotype and childhood ALL was noted (OR 1.29, 95%CI 1.10–1.62) (Table 3; Figure 2). Subgroup analysis revealed a significant association among Asian subjects only (OR 1.54, 95%CI 1.12–2.10) whereas no association was observed among White (OR 1.13, 95%CI 0.96–1.35) and Black (OR 1.62, 95%CI 0.96–2.73) populations (Table 4).
Forest plots for GSTM1 (a) and GSTT1 (b), showing the association between these genotypes and risk of childhood acute lymphoblastic leukemia (ALL). Overall analysis showed an increased risk with GSTM1 null genotype (odds ratio (OR) 1.29, 95% confidence interval (CI) 1.10–1.62), but no association of GSTT1 genotype and childhood ALL (OR 1.17, 95%CI 0.97–1.41). A full color version of this figure is available at the Journal of Human Genetics journal online.
GSTP1
Only 10 studies (6 from Whites and 4 from Asians) comprising 1576 cases and 2205 controls were found to examine the association between GSTP1 genotype and childhood ALL and were analyzed. Analysis was done using dominant (AG+GG vs AA) and recessive (AA+AG vs GG) models of analysis. Between-study heterogeneity was not significant; however, random-effect OR was used to provide a conservative estimate of effect size. No significant association between GSTP1 genotype and risk of ALL was found in any of the models of analysis—dominant (OR 1.13, 95%CI 0.99–1.3) or recessive (OR 1.20, 95%CI 0.93–1.55) (Table 3; Figure 3). Subgroup analysis according to ethnicities did not reveal any significant association among Whites or Asians in the dominant model. However in the recessive model GSTP1 mutation was associated with almost twofold higher risk of ALL (OR 1.93, 95%CI 1.21–3.09) in Asians (Table 4). There were no studies examining the association of GSTP1 and childhood ALL among the Blacks.
Forest plots showing the association of GSTP1 genotypes ((a) dominant and (b) recessive models of analysis) with childhood acute lymphoblastic leukemia (ALL). Overall analysis shows no association in either of the models (dominant (odds ratio (OR) 1.13, 95% confidence interval (CI) 0.99–1.3) or recessive (OR 1.20, 95%CI 0.93–1.55)). A full color version of this figure is available at the Journal of Human Genetics journal online.
GSTT1
In all, 20 studies (11 on Whites, 2 on Blacks and 7 on Asians) comprising 2826 cases and 4232 controls were analyzed for the association of GSTT1 null mutation and the risk of childhood ALL. Between-study heterogeneity was high and random-effect OR was used to determine the effect size. Funnel plot did not reveal any obvious asymmetry. No association between GSTT1 null genotype and ALL was observed in the overall analysis (OR 1.17, 95%CI 0.97–1.41) (Table 3; Figure 2). However, there was significantly enhanced risk among the Asian subjects (OR 1.63, 95%CI 1.32–1.99), while a lack of association was seen among Whites (OR 0.98, 95%CI 0.77–1.24) and Blacks (OR 0.97, 95%CI 0.32–3.06) (Table 4).
Discussion
Of the various genes implicated in enhancing the susceptibility to childhood ALL, genes encoding the detoxifying enzymes in the body are important.31 GST group of enzymes are among those detoxifying enzymes responsible for metabolism of xenobiotics in the body, thereby reducing the body’s exposure to environmental toxins and leukemogens.6 Many studies have been conducted till date to find the association between genes of GST family and the risk of childhood leukemias especially ALL. But unfortunately, similar to other genetic association studies no consistent trend have been observed. This lack of consensus between studies prompted subsequent investigators to examine these associations among subjects of various ethnicities. But the validity of most of these studies was threatened due to inadequate sample size, as well as bias in selection of cases and controls.32 Ethnic differences have also been cited to be one of the reasons behind this disagreement.32 Even a lack of agreement was observed among the four previous studies conducted on Indian children.8, 9, 10, 11
All the earlier studies from India have originated from south India which has a distinct genetic pool from north India. Three of these studies examined only GSTM1 and GSTT1 genes of the GST pathway,8, 9, 11 whereas one examined the association of GSTM1 and GSTP1 genes with childhood ALL.10 Our study is the first to evaluate association of all the three genes among north Indian children and the first of its kind to be conducted among north Indian children. We have selected non-age matched controls because taking blood samples from healthy children as controls was an ethical issue, moreover we do not have any cord blood archival system in our set-up to recruit control samples.
In the present study, GSTT1 null mutation was seen to increase the risk of childhood leukemia, whereas GSTM1 mutation did not increase the risk. However, we found that co-existence of double (GSTT1 and GSTM1) null genotype increased the risk of ALL by 3.5 times. The lack of association between GSTM1 and ALL seen in our study did not compare favorably with the previously published Indian studies except one,9 similarly the role of GSTT1 null genotype was in agreement with only one of these previous studies.12 The evidence for the increased risk of ALL in children with GSTM1 null genotype was conflicting, with many14, 25, 29 endorsing such an association while others7, 9, 16 refuting it. This difference in observations may stem from sample size issues, population heterogeneity and difference in susceptibility across populations.32 However what appears more common between studies is the association of double null (GSTM1 and GSTT1) genotypes and childhood ALL.11, 23
The differential susceptibility of the GSTM1 and GSTT1 genotypes may be due to the difference in the set of chemicals metabolized by these genes.4
Only one study form India have examined the association of GSTP1 genotype with childhood ALL but could not find any association, our findings however support the association of GSTP1 mutation (homozygous/GG) with an increased risk similar to the one reported by a Canadian study.18 Our finding of increased risk of ALL with compound mutant genotype (GSTM null and mutant GSTP) however agrees with both the previous studies.
We also observed that combination of mutant genotypes (GSTM null, GSTT null and mutant GSTP) was associated with more than sixfold increase in risk of childhood ALL, which can be explained by the fact that individuals with mutations in all the varieties of detoxifying GST family of enzymes would be the most inefficient handlers of environmental leukemogens making themselves vulnerable to development of ALL.
The latest meta-analysis on GSTM and GSTT combines data till 2012 but it combined evidence from studies dealing with all forms of childhood leukemias including ALL, AML and ANLL. The biology of different types of childhood leukemia is different and combining all the varieties into a common group while studying genetic risk may not be prudent. Moreover, few studies were missed in some of the previous meta-analyses while new case–control studies were published after those.
In view of the above factors and also the fact that our study did not generate a clear evidence (as ORs were only borderline) and also differed with some of the previously published data from India, we performed a meta-analysis. This is an updated meta-analysis combining studies which deal with childhood ALL only. We searched for indexed publications in Pubmed and Medline databases whereas Google Scholar was searched to locate articles in un-indexed locations. In fact one Indian study9 found in such an un-indexed location was not included by the authors of the earlier meta-analyses3, 32, 33, 34, 35 on this subject, except one36 which studied the association of GST genes with acute leukemia among Asians only.
We combined 22, 10 and 20 studies each for GSTM1, GSTP1 and GSTT1 genes respectively including larger number of subjects compared with the previous meta-analyses.3, 32, 33, 34, 35, 36 We also noted a considerable lack of studies among Black subjects, only two studies examined the association of GSTM1 and GSTT1 in a limited number of Black subjects (n=473). No GSTP1-related study conducted among the Blacks was noted by us.
Our meta-analysis revealed an overall association of only GSTM1 with childhood ALL whereas there was no association observed with GSTP1 or GSTT1 genotypes. The results of our case–control study did not go hand-in-hand with the findings of meta-analysis especially with regard to the GSTM1 genotype, this was due to a small sample size generating an inadequate power of the study. The case–control analyses with GSTT1 and GSTP1 however yielded powers >80% and revealed results that were comparable to the meta-analysis results.
Our findings pertaining to the GSTM1 genotype is in agreement with all the previously conducted meta-analyses,3, 32, 33, 34, 35, 36 while that pertaining to GSTT1 compared favorably with some33, 34 while disagreeing with others.32, 35, 36 None of the earlier meta-analyses found any association between GSTP1 polymorphism and risk of childhood ALL.3, 33, 36
The presence of significant association of childhood ALL with both GSTM and GSTT among Asians, as seen in our study was noted by earlier studies as well.34, 35, 36 The reason behind this finding may be different genetic susceptibility of Asians as well as excessive exposure to environmental toxins in Asian children as compared with others,37 which may be reflective of the rapid rate of industrialization of Asian countries near the time when these studies were conducted. However, the above explanation is only based on speculation at this stage pending further evidence. A similar association was also noted in the recessive model for the GSTP1 genotype in Asians, which may be due to small number of studies available or reasons as described above.
Our findings highlight the need of more data from well-designed case–control studies conducted on individuals from all the ethnicities, especially the Blacks, where the data are extremely scanty.
In conclusion, our study provides data on GST genes and risk of ALL in north Indian children for the first time, showing the association of childhood ALL with GSTT1 and GSTP1 genotypes only. The updated meta-analysis endorsed the findings of previous meta-analyses and demonstrated a greater GST gene variation-related risk of childhood ALL in the Asians.
References
Pui, C. H. & Evans, W. E. Treatment of acute lymphoblastic leukemia. New Engl. J. Med. 354, 166–178 (2006).
Perera, F. P. Environment and cancer: who are susceptible? Science 278, 1068–1073 (1997).
Huang, G. Z., Shan, W., Zeng, L. & Huang, L. G. The GSTP1 A1578G polymorphism and the risk of childhood acute lymphoblastic leukemia: results from an updated meta-analysis. Genet. Mol. Res. 12, 2481–2491 (2013).
Strange, R. C., Spiteri, M. A., Ramachandran, S. & Fryer, A. A. Glutathione-S-transferase family of enzymes. Mutat. Res. 482, 21–26 (2001).
Allan, J. M., Wild, C. P., Rollinson, S., Willett, E. V., Moorman, A. V., Dovey, G. J. et al. Polymorphism in glutathione S-transferase P1 is associated with susceptibility to chemotherapy-induced leukemia. Proc. Natl Acad. Sci. USA 98, 11592–11597 (2001).
Strange, R. C. & Fryer, A. A. The glutathione S-transferases: influence of polymorphism on cancer susceptibility. IARC Sci. Publ. 148, 231–249 (1999).
Chen, C. L., Liu, Q., Pui, C. H., Rivera, G. K., Sandlund, J. T., Ribeiro, R. et al. Higher frequency of glutathione S-transferase deletions in black children with acute lymphoblastic leukemia. Blood 89, 1701–1707 (1997).
Joseph, T., Kusumakumary, P., Chacko, P., Abraham, A. & Radhakrishna Pillai, M. Genetic polymorphism of CYP1A1, CYP2D6, GSTM1, and GSTT1 and susceptibility to acute lymphoblastic leukaemia in Indian children. Pediatr. Blood Cancer 43, 560–567 (2004).
Haranatha Reddy, P. & Jamil, K. Polymorphisms in the GST (M1 andT1) gene and their possible association with susceptibility to childhood acute lymphocytic leukemia in Indian population. African J. Biotechnol. 5, 1454–1456 (2006).
Suneetha, K. J., Nancy, K. N., Rajalekshmy, K. R., Sagar, T. G. & Rajkumar, T. Role of GSTM1 (Present/Null) and GSTP1 (Ile105Val) polymorphisms in susceptibility to acute lymphoblastic leukemia among the South Indian population. Asian Pac. J. Cancer Prev. 9, 733–736 (2008).
Dunna, N. R., Vure, S., Sailaja, K., Surekha, D., Raghunadharao, D., Rajappa, S. et al. Deletion of GSTM1 and T1 genes as a risk factor for development of acute leukemia. Asian Pac. J. Cancer Prev. 14, 2221–2224 (2013).
Indian Genome Variation Consortium. Genetic landscape of the people of India: a canvas for disease gene exploration. J. Genet. 87, 3–20 (2008).
Majumder, P. P. The human genetic history of South Asia. Curr. Biol. 20, R184–R187 (2010).
Krajinovic, M., Labuda, D., Richer, C., Karimi, S. & Sinnett, D. Susceptibility to childhood acute lymphoblastic leukemia: influence of CYP1A1, CYP2D6, GSTM1, and GSTT1 genetic polymorphisms. Blood 93, 1496–1501 (1999).
Saadat, I. & Saadat, M. The glutathione S-transferase mu polymorphism and susceptibility to acute lymphocytic leukemia. Cancer Lett. 158, 43–45 (2000).
Davies, S. M., Bhatia, S., Ross, J. A., Kiffmeyer, W. R., Gaynon, P. S., Radloff, G. A. et al. Glutathione S-transferase genotypes, genetic susceptibility, and outcome of therapy in childhood acute lymphoblastic leukemia. Blood 100, 67–71 (2002).
Alves, S., Amorim, A., Ferreira, F., Norton, L. & Prata, M. J. The GSTM1 and GSTT1 genetic polymorphisms and susceptibility to acute lymphoblastic leukemia in children from north Portugal. Leukemia 16, 1565–1567 (2002).
Krajinovic, M., Labuda, D. & Sinnett, D. Glutathione S-transferase P1 genetic polymorphisms and susceptibility to childhood acute lymphoblastic leukaemia. Pharmacogenetics 12, 655–658 (2002).
Balta, G., Yuksek, N., Ozyurek, E., Ertem, U., Hicsonmez, G., Altay, C. et al. Characterization of MTHFR, GSTM1, GSTT1, GSTP1, and CYP1A1 genotypes in childhood acute leukemia. Am. J. Hematol. 73, 154–160 (2003).
Barnette, P., Scholl, R., Blandford, M., Ballard, L., Tsodikov, A., Magee, J. et al. High-throughput detection of glutathione s-transferase polymorphic alleles in a pediatric cancer population. Cancer Epidemiol. Biomarkers Prev. 13, 304–313 (2004).
Canalle, R., Burim, R. V., Tone, L. G. & Takahashi, C. S. Genetic polymorphisms and susceptibility to childhood acute lymphoblastic leukemia. Environ. Mol. Mutagen. 43, 100–109 (2004).
Wang, J., Zhang, L., Feng, J., Wang, H., Zhu, S., Hu, Y. et al. Genetic polymorphisms analysis of glutathione S-transferase M1 and T1 in children with acute lymphoblastic leukemia. J. Huazhong Univ. Sci. Technolog. Med. Sci. 24, 243–244 (2004).
Pakakasama, S., Mukda, E., Sasanakul, W., Kadegasem, P., Udomsubpayakul, U., Thithapandha, A. et al. Polymorphisms of drug-metabolizing enzymes and risk of childhood acute lymphoblastic leukemia. Am. J. Hematol. 79, 202–205 (2005).
Clavel, J., Bellec, S., Rebouissou, S., Menegaux, F., Feunteun, J., Bonaiti-Pellie, C. et al. Childhood leukaemia, polymorphisms of metabolism enzyme genes, and interactions with maternal tobacco, coffee and alcohol consumption during pregnancy. Eur. J. Cancer Prev. 14, 531–540 (2005).
Aydin-Sayitoglu, M., Hatirnaz, O., Erensoy, N. & Ozbek, U. Role of CYP2D6, CYP1A1, CYP2E1, GSTT1, and GSTM1 genes in the susceptibility to acute leukemias. Am. J. Hematol. 81, 162–170 (2006).
Pigullo, S., Haupt, R., Dufour, C., Di Michele, P., Valsecchi, M. G., Basso, G. et al. Are genotypes of glutathione S-transferase superfamily a risk factor for childhood acute lymphoblastic leukemia? Results of an Italian case-control study. Leukemia 21, 1122–1124 (2007).
Chan, J. Y., Ugrasena, D. G., Lum, D. W., Lu, Y. & Yeoh, A. E. Xenobiotic and folate pathway gene polymorphisms and risk of childhood acute lymphoblastic leukaemia in Javanese children. Hematol. Oncol. 29, 116–123 (2011).
Gra, O. A., Glotov, A. S., Kozhekbaeva, Z., Makarova, O. V. & Nasedkina, T. V. [Genetic polymorphism in GST, NAT2, and MTRR and susceptibility to childhood acute leukemia]. Mol. Biol. (Mosk) 42, 214–225 (2008).
Rimando, M. G., Chua, M. N., Yuson, E., de Castro-Bernas, G. & Okamoto, T. Prevalence of GSTT1, GSTM1 and NQO1 (609C>T) in Filipino children with ALL (acute lymphoblastic leukaemia). Biosci. Rep. 28, 117–24 (2008).
Gatedee, J., Pakakassama, S., Muangman, S. & Pongstaporn, W. Glutathione S-transferase P1 genotypes, genetic susceptibility and outcome of therapy in Thai childhood acute lymphoblastic leukemia. Asian Pac. J. Cancer Prev. 8, 294–296 (2007).
Pui, C. H., Robison, L. L. & Look, A. T. Acute lymphoblastic leukaemia. Lancet 371, 1030–1043 (2008).
Ye, Z. & Song, H. Glutathione s-transferase polymorphisms (GSTM1, GSTP1 and GSTT1) and the risk of acute leukaemia: a systematic review and meta-analysis. Eur. J. Cancer 41, 980–989 (2005).
Vijayakrishnan, J. & Houlston, R. S. Candidate gene association studies and risk of childhood acute lymphoblastic leukemia: a systematic review and meta-analysis. Haematologica 95, 1405–1414 (2010).
Tang, Q., Li, J., Zhang, S., Yuan, B., Sun, H., Wu, D. et al. GSTM1 and GSTT1 null polymorphisms and childhood acute leukemia risk: evidence from 26 case-control studies. PLoS ONE 8, e78810 (2013).
Xu, L. Y. & Cao, L. F. GSTT1 genetic polymorphism and susceptibility to childhood acute lymphoblastic leukemia: a meta-analysis. Tumour Biol. 35, 1433–1437 (2014).
Tang, Z. H., Zhang, C., Cheng, P., Sun, H. M., Jin, Y., Chen, Y. J. et al. Glutathione-S-transferase polymorphisms (GSTM1, GSTT1 and GSTP1) and acute leukemia risk in Asians: a meta-analysis. Asian Pac. J. Cancer Prev. 15, 2075–2081 (2014).
Ebenstein, A. The consequences of industrialization: evidence from water pollution and digestive cancers in China. Rev. Econ. Stat. 94, 186–201 (2012).
Acknowledgements
NRM is supported by a post-doctoral grant from the Indian Council of Medical Research, New Delhi, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Moulik, N., Parveen, F., Kumar, A. et al. Glutathione-S-transferase polymorphism and acute lymphoblastic leukemia (ALL) in north Indian children: a case–control study and meta-analysis. J Hum Genet 59, 529–535 (2014). https://doi.org/10.1038/jhg.2014.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.66
This article is cited by
-
Meta-analysis of polymorphic variants conferring acute lymphoblastic leukemia risk in the Indian population
The Nucleus (2024)
-
Genetic association study of rs1801133 of MTHFR, rs4646903 of CYP1A1, null mutation of GSTM1&GSTT1 with leukemia in the Jammu region of north Indian population
The Nucleus (2023)
-
Impact of ABCB1 Gene (C3435T/A2677G) Polymorphic Sequence Variations on the Outcome of Patients with Chronic Myeloid Leukemia and Acute Lymphoblastic Leukemia in Kashmiri Population: A Case–Control Study
Indian Journal of Hematology and Blood Transfusion (2021)
-
Glutathione S-Transferase P1 313 (A > G) Ile105Val Polymorphism Contributes to Cancer Susceptibility in Indian Population: A Meta-analysis of 39 Case–Control Studies
Indian Journal of Clinical Biochemistry (2020)