Abstract
Studies on the association of methylenetetrahydrofolate reductase (MTHFR) genotype in childhood acute lymphoblastic leukemia (ALL) have yielded conflicting results. The present study examines this association in north Indian children with ALL and includes an updated meta-analysis. MTHFR (677 and 1298) genotype of children with ALL and healthy adult controls were done by the PCR–restriction fragment length polymorphism (PCR-RFLP) method and were compared using various models of inheritance. A total of 150 patients and 300 controls were included. The 677T allele was found protective (odds ratio (OR) 0.21, 95% confidence interval (CI) 0.04–0.94), whereas 1298C allele led to an increase in risk (OR 4.44, 95% CI 2.19–8.99) of childhood ALL. Meta-analysis included 31 and 27 studies examining the association of 677 and 1298 genotypes, respectively. The 677 C→T polymorphism was protective (OR 0.90, 95% CI 0.82–0.99). Protection was more pronounced in folate-sufficient populations as compared with those not covered by folate fortification guidelines. The 1298A→C polymorphism was associated with a marginal increase in risk (OR 1.19, 95% CI 1.01–1.40).
Similar content being viewed by others
Introduction
Acute lymphoblastic leukemia (ALL) is the most common childhood malignancy seen all over the world.1 The etiopathogenesis of ALL is partly because of genetic susceptibility and partly because of environmental factors.2 Many genes including that of the folate metabolism have been studied as probable risk modifiers for pediatric ALL. Methylenetetrahydrofolate reductase (MTHFR) gene has been the most frequently studied gene in this context with variable results.3 Interethnic variation of susceptibility, dietary folate availability, genotyping errors as well as lack of adequate power of the individual studies because of small number of subjects may be responsible for the contradictory results.3, 4 These factors in varying combinations might have yielded different answers to the same question. To circumvent the problem of underpowered studies, many meta-analyses were performed using case–control studies.
The MTHFR enzyme leads to the formation of 5-MTHF (5-methyl tetrahydroxyfolate), the circulating form of folic acid, and a methyl donor for the conversion of homocysteine to methionine. Polymorphisms in the MTHFR gene lead to alteration in the enzyme’s activity by altering its thermal stability or affinity toward its coenzyme, thereby reducing production of 5-MTHF.5 This decrease in the enzyme activity may alter folate metabolism leading to alteration in DNA formation and stability that in turn may alter the risk of malignancy. Numerous studies have been conducted to investigate the association between MTHFR polymorphisms and various types of solid and hematological cancers in both adults and children.
Most of the case–control studies have revealed a protective role of 677T allele and no effect of 1298C allele on the development of childhood ALL. In the present study we examined the association between MTHFR polymorphism (at 677 and 1298 loci) and pediatric ALL in a case–control study and also performed a meta-analysis including the present as well as previous studies from India and around the world in order to present the latest and most updated evidence to assess the risk modification of childhood ALL by MTHFR genotypes. This is the largest case–control study from India and the first from this part of the country and the current meta-analysis provides an update to the last meta-analysis conducted on this subject.3
Materials and methods
Case–control study
Patients and controls
The ALL patients ranged between 1 and 15 years of age admitted for treatment in the department of Paediatrics of the King George’s Medical University, Lucknow, India from July 2011 till June 2013 were taken as cases. The controls were normal healthy adults (between 18 and 40 years of age) without any history of malignancy or any other disease. The study was performed in accordance with the ethical standards laid down by the Declaration of Helsinki, and all individuals/parents of the children with ALL involved gave their informed consent before inclusion in the study. Furthermore, the study was also approved by the ethics committees of King George’s Medical University, Lucknow, India, and Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India. Peripheral blood samples (5 ml) were collected in EDTA-coated vials and stored at −20 °C until use. Genomic DNA was obtained using genomic DNA extraction kit from Quiagen (Brand GMbH and Co KG, cat no. 51104, Valencia, CA, USA).
Genotype analysis
Genotypes for MTHFR 677 and 1298 loci were determined by PCR–restriction fragment length polymorphism (PCR-RFLP) method; the primers for PCR amplification, restriction enzymes for RFLP and the reaction conditions are mentioned in Supplementary Table S1. The RFLP products were run on 9 and 12% non-denaturing polyacrylamide gel for 677 and 1298 loci respectively and stained with ethidium bromide. The sizing of the RFLP product was done using 10-bp DNA ladder, the PCR product was visualized under ultraviolet light and scored by two different observers, genotyping was performed in batches and at the end of each batch genotype and allele frequency was matched from previous one to avoid the confounding factor. After decoding the results of two different observers, nearly 15% of the samples required re-genotyping because of lack of mutual agreement. In addition, 10% of the samples were randomly selected and subjected to sequencing and the results were compared with that of the PCR-RFLP findings.
Meta-analysis
Search strategy
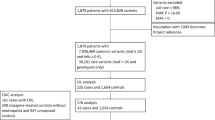
PubMed database was searched using MESH terms Leukemia/etiology and methylenetetrahyrofolatereductase (NADPH2)/etiology and general terms like case–control studies, P(a)ediatric/childhood ALL, MTHFR polymorphism, genetic association and folate pathway genes. In addition, Google scholar was also searched for studies that may have been published in non-PubMed indexed journals. The last date of search was 30 October 2013. A total of 22 studies were shortlisted and 8 more studies were included based on bibliography search. We also searched the previously published meta-analyses to identify relevant studies. In addition, one study was included from Google scholar search. The total numbers of studies analyzed were 31 and 27 for MTHFR 677 and 1298 polymorphisms, respectively. The details of the search results are depicted in Supplementary Figure S1.
Inclusion criteria
We included studies that were published in English language, had a case–control design, had children of ALL as the cases and individuals without any history of malignancy as the controls and had sufficient accessible data required to calculate the effect size of the polymorphisms. All related studies that were not in case–control design (for example, case series, cohort studies without a control group, family-based studies) were excluded. The reporting quality of the studies were also assessed by the quality control, validity of genotyping technique, number of cases and controls in each genotype and conformity of the control groups to Hardy–Weinberg equilibrium (HWE).
Data extraction
Data extraction was done after two different investigators (NRM and FP) independently reviewed the abstracts followed by the full texts of relevant studies, and any difference in the opinion was sorted out upon mutual discussion. The following data were extracted from the studies: first author, year of publication, ethnicity and country, number of cases and control subjects. The frequencies of the allele and the genotypic distributions were extracted (if not available, the allele frequencies were calculated from genotypes) for both the cases and the controls.
Statistical analysis
Allele and genotype frequency differences were tested between patients and controls by means of two-sided Fisher’s exact test with Bonferroni correction. The magnitude of the effect was estimated by odds ratio (OR) and its 95% confidence interval (CI). Statistical analysis was performed by using SPSS version 20.0 for Windows (Statistical Package for Social Sciences, SPSS, IBM Corporation, New York, NY, USA). Yates correction was applied wherever required. Allele and genotype frequencies, heterozygosities and likelihood ratio were tested for HWE via a 2 degree-of- freedom χ2 goodness of fit by using software PopGen v 16 (http://www.ualberta.ca/~fyeh/popgene.html). The haplotype analysis was carried out using Arliquin v3.5 software package (http://cmpg.unibe.ch/software/arlequin35/, University of Geneva, Switzerland).
The meta-analysis was carried out using the Meta Analyst v2.0 (http://tuftscaes.org/meta_analyst) software based on bivariate and random effect models. The risk of ALL associated with the MTHFR C677T and A1298C polymorphisms was evaluated by OR, risk ratio and risk difference with corresponding 95% CIs under allele contrast, dominant and the recessive models. The heterogeneity between studies was assessed using the I2 value along with Cochrane Q-statistic. A P-value of <0.10 was taken as significant for assessing heterogeneity. We chose to perform the random effects OR for all the models in order to provide a conservative estimate of the overall effect size. Recursive cumulative meta-analysis was also performed to determine the temporal trend in change of evidence with availability of more studies (Supplementary Figures S2 and S3). The forest plots were drawn with the use of ORs. We also compared the genotype frequencies of both cases and controls of all the studies included with that of our study subjects to examine the population/ethnic differences between our study subjects and other studies included in the meta-analysis (Supplementary Tables S2 and S3). Subgroup analysis was done according to the continents of origin (Supplementary Table S4) as well as existing folate fortification guidelines (Table 1).
Results
Case–control study
A total of 150 children with mean (±s.d.) age of 7.5 (±3.2) years and gender ratio of 7.4:1(M/F) diagnosed as ALL were included as cases. Immunophenotyping of the cases revealed B-ALL in 106 and T-ALL in 28 children; immunophenotyping could not be done in 16 of these children. Genotyping by PCR-RFLP was successfully done in all the children with ALL and the control subjects included in the study. The genotypic frequencies for MTHFR 677 and 1298 loci were in HWE in both cases and controls (P-values for HWE for 677 genotype were 0.69 and 0.26 for cases and controls respectively; P-values for HWE for 1298 genotype were 0.89 and 0.13 for cases and controls respectively). The different genotypes, alleles, recessive, dominant and additive models for both the single-nucleotide polymorphisms under study are presented in Table 2.
There were significant differences in the genotypic frequencies between cases and controls for both the 677 and 1298 polymorphisms. The 677T allele was found to be protective for development of childhood ALL (OR 0.21, 95% CI 0.04–0.94; P=0.024 for TT genotype). In both the dominant and recessive models of comparison, TT and CT were found protective for ALL in children. The T allele (OR 0.57, 95% CI 0.38–0.84; P=0.005) conferred protection against childhood ALL, whereas the C allele (OR 1.74, 95% CI 1.18–2.57; P=0.005) was associated with increased risk.
The 1298C allele revealed higher risk of ALL among children with ALL (OR 4.44, 95% CI 2.19–8.99; P<0.0001 for CC genotype). Both the dominant and recessive models showed similar increase in risk. The C allele was associated with an increase in risk of childhood ALL (OR 1.87,95% CI 1.39–2.51; P=0.0001), whereas the A allele was found to be protective (OR 0.53, 95% CI 0.39–0.71; P=0.0001).
Upon haplotypic analyses (Table 2) there were four possible combinations; that is, CC, CA, TA and TC. One (CC) of these was associated with increased risk (OR 2.06, 95% CI 1.53–2.77; P<0.0001) and two (CA and TA) were protective in nature (OR for CA 0.73, 95% CI 0.55–0.96; P=0.028) and (OR for TA 0.62, 95% CI 0.41–0.93; P=0.021).
Meta-analysis
In this meta-analysis we included 31 studies6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 and 27 studies6, 7, 9, 10, 11, 12, 13, 14, 15, 17, 18, 20, 21, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 examining the association of MTHFR677 and MTHFR1298 polymorphisms and childhood ALL, respectively. There were 12 studies from Asia, 11 from Europe, 4 from South America, 2 from North America and 1 from Africa.
The allele contrast, dominant and recessive models were used while analyzing the effect of polymorphism (Table 2). In the pooled analysis (including all the studies), the 677 C→T polymorphism was found to be imparting protection in the recessive (OR 0.84, 95% CI 0.75–0.95; P=0.01) and allele contrast (OR 0.90, 95% CI 0.82–0.99; P=0.05; Figure 1) models, whereas the 1298A→C polymorphism was found to be associated with a borderline increase in risk for childhood ALL only in the allele contrast model (OR 1.19, 95% CI 1.01–1.40; P=0.05; Figure 1). Leave-one-out analysis did not suggest excessive influence of any one study on the overall effect size in any of the models.
Forest plots (allele contrast model) showing the association of methylenetetrahydrofolate reductase (MTHFR; 677 and 1298) genotypes with childhood acute lymphoblastic leukemia (ALL). (a) A protective effect of MTHFR C677T mutation on the risk of childhood ALL, cumulative odds ratio 0.90 (0.82–0.99), and (b) marginal increase in risk of childhood ALL with MTHFR A1298C mutation; cumulative odds ratio 1.19 (1.01–1.40). A full color version of this figure is available at the Journal of Human Genetics journal online.
Subgroup analyses of the studies grouped according to the continents of origin as well as by the existing folate fortification guidelines were also done (Table 1 and Supplementary Table S4). The groups comprising South American and Asian studies showed protective effect of 677T allele in the allele contrast and recessive models, respectively, whereas increased risk was observed for 1298C allele from the South American group. Countries with folate fortification (United States, Canada, Brazil and Indonesia)7, 9, 13, 20, 29, 34 showed a higher protection of 677T allele as compared with those without fortification. The 1298C allele was found to increase the risk in countries with folate fortification, an effect that was no longer significant (OR 1.37, 95% CI 0.98–1.92) on removing the study from the United States.20
Discussion
Folate pathway genes, responsible for the one-carbon metabolism, have received special attention in cancer genetics. Among hematological malignancies, the association of folate pathway genes and acute leukemias are the best studied and the association of MTHFR polymorphisms has received special interest. The MTHFR genotypes, and especially the 677T allele are known to modify cancer risk in a site-specific manner.35 Many studies have investigated its association with childhood ALL in children from different ethnicities including those from India. The present study is the largest case–control study (including 150 patients and 300 controls) form India. The cases were children with a diagnosis of ALL, whereas healthy adults (18–40 years) without any environmental risk factors for cardiovascular diseases or malignancies were taken as controls. Like previous investigators,16, 17, 21, 28 we also had to choose adults as controls because drawing blood for genotyping from a large number of healthy children was an ethical issue and facility for archival of cord blood20, 23 is unavailable at our center.
Our study showed protective role of 677T allele in childhood ALL in the dominant, recessive and the additive models. Haplotype analysis also revealed protective effect. The 1298C allele was associated with increase in the risk of ALL among children. One of the previous north Indian studies showed increased risk of ALL with 677T allele,25 whereas another showed no association.31 When ALL and 1298C allele were taken into consideration, none of these studies revealed any association. Of the studies done from south India, one study showed lack of effect of MTHFR genotypes at both the loci,26 whereas the other showed protective effect with both 677T and 1298C alleles.14 This discrepancy in the findings from the same geographical area was perplexing; the probable reason behind this may be the small sample sizes and the wide genetic variation in the population of the Indian subcontinent that is diverse and known to give rise to prevalence of variable single-nucleotide polymorphism patterns among different regions as well as between communities and castes.36 Our findings pertaining to the 677T allele is in agreement with most of the association studies done worldwide, and that related to the 1298C allele is compatible with some of the earlier studies.11, 33, 34 Many studies6, 12, 13, 21, 25 show a lack of effect of 1298C allele on childhood ALL, whereas few of them show protection.18, 27
Of the 7 previously published meta-analyses on this subject, the latest one done in 2011 included 25 and 22 studies for the 677T and 1298C alleles, respectively.3 The present meta-analysis includes a larger number of studies compared with the previously published ones (Table 3).
Although there exists a considerable amount of disagreement among the meta-analyses3, 4, 37, 38, 39, 40, 41 performed till date (Table 3), the trend of the results point towards a protective effect of the 677T allele and lack of association between 1298C allele and ALL risk in children. One of these meta-analyses40 showed an increase in risk with 1298C allele, a finding not endorsed by the rest. The difference in the findings of the meta-analyses may be because of nonuniform inclusion and exclusion criteria resulting in variation in the number of studies included for analysis.3 The present meta analysis, like the previous ones,37, 38 also demonstrated statistically significant protective effect of the 677T allele and showed only a borderline increase in risk of childhood ALL with 1298C allele and that too only in the allele contrast model.
To examine the ethnic differences in the effect of MTHFR and ALL risk, we performed meta-analysis grouping studies according to their continents of origin as details on the ethnicity of the study groups were unavailable in many of the studies. While studying the intercontinental variation of susceptibility, we found statistically significant protection of 677T allele in the Asian and the South American studies as compared with the European studies, whereas for the 1298C allele no significant effect was observed from any part of the world. Data from Africa were insufficient as we had only one study from the entire continent.18
Gene–environment interactions play a significant role in deciding the resultant effect of a genotype on a certain disease risk that is true for the enzymes of folate pathway as well. Availability of dietary folates alter the effect of genetic polymorphisms in the folate pathway. One of the major deficits in the association studies pertaining to MTHFR polymorphisms and ALL risk is the noninclusion of the folate status of the subjects in most of these studies. Taking cognizance of this phenomenon, we tried to examine the combined effect of MTHFR genotype and folate status on the risk of childhood ALL. When the countries were stratified by mandatory folate fortification guidelines, significant protection of 677T allele was documented in the group of countries with mandatory fortification (United States, Canada, Brazil and Indonesia)7, 9, 13, 20, 29, 34 and not in those without fortification. The protective effect that we observed in our meta-analysis may be a combined effect of adequate folate levels as well as the genetic factors. Although mandatory fortification guidelines may not be reflective of the folate levels in the study subjects, we had no other way to assess folate status as data related to folate levels in the study subjects are sparse;3 moreover, studies show that folate fortification of food has raised the mean serum folate level of the population covered, thereby reducing the prevalence of folate deficiency.42 We found a borderline increase in risk of ALL with the 1298C allele in the folate-fortified countries, an observation difficult to explain given the beneficial role of folate in reducing risk of various cancers including that of acute leukemias. However, this significant effect size was lost when we performed leave-one-out analysis (OR 1.37, 95% CI 0.98–1.92) excluding the study from the United States6 that, when included, altered the OR for the entire group of folate-fortified countries. Recursive cumulative meta-analysis (Supplementary Figures S1 and S2) showed gradual narrowing of the CIs with accumulation of more studies over the years.
The protective effect of the 677T allele on childhood leukemia may be because of reduced MTHFR enzyme activity and consequent intracellular accumulation of 5,10-methylene leading to decreased uracil mis-incorporation to the DNA thereby preventing neoplastic transformation (Figure 2). This protective effect may in fact be enhanced in the presence of adequate dietary folate intake, an effect observed in both adult ALL43 and colorectal carcinomas.44 In the presence of inadequate folate intake, the protective effect offered by the genotype may get mitigated.43 This explains the statistically significant protection rates of the 677T allele in populations under mandatory food folate fortification.43 The lack of association of 1298C allele on the risk of ALL may be because of less significant alteration in the MTHFR enzyme produced by polymorphism at this locus. In conclusion, we found that in north Indian children, 677T allele is protective whereas 1298C allele increases the risk of developing ALL. The risk of childhood ALL is modulated by MTHFR polymorphisms but the effect varies between ethnic groups and populations with different folate intakes. Present meta-analysis shows a protective effect of 677T allele on childhood ALL that appears to be more in children from regions with mandatory folate fortification guidelines. No effect of 1298C allele on the risk of childhood ALL was observed. Studies from around the world taking into account the folate status of the study subjects are needed to arrive at a meaningful inference of the yet unresolved issue of association between childhood ALL and MTHFR polymorphism.
Effect of methylenetetrahydrofolate reductase (MTHFR) polymorphism and folate availability on leukemogenesis. This figure depicts the proposed relationship between leukemogenesis and MTHFR gene mutation in situations of adequate availability of folate versus folate deficiency. MTHFR mutation leading to decreased enzyme activity leads to increased uracil misincorporation (and susceptibility to leukemia) in states of folate deficiency and vice versa.
References
Pui, C. H., Relling, M. V. & Downing, J. R. Acute lymphoblastic leukemia. N. Engl. J. Med. 350, 1535–1548 (2004).
Kim, Y. I. Methylenetetrahydrofolate reductase polymorphisms, folate, and cancer risk: a paradigm of gene-nutrient interactions in carcinogenesis. Nutr. Rev. 58, 205–209 (2000).
Wang, H., Wang, J., Zhao, L., Liu, X. & Mi, W. Methylenetetrahydrofolate reductase polymorphisms and risk of acute lymphoblastic leukemia-evidence from an updated meta-analysis including 35 studies. BMC Med. Genet. 13, 77 (2012).
Zintzaras, E., Doxani, C., Rodopoulou, P., Bakalos, G., Ziogas, D. C., Ziakas, P. et al. Variants of the MTHFR gene and susceptibility to acute lymphoblasticleukemia in children: a synthesis of genetic association studies. Cancer Epidemiol. 36, 169–176 (2012).
Sibani, S., Leclerc, D., Weisberg, I. S., O'Ferrall, E., Watkins, D., Artigas, C. et al. Characterization of mutations in severe methylenetetrahydrofolate reductase deficiency reveals an FAD-responsive mutation. Hum. Mutat. 21, 509–520 (2003).
Wiemels, J. L., Smith, R. N., Taylor, G. M., Eden, O. B., Alexander, F. E., Greaves, M. F. et al. United Kingdom Childhood Cancer Study Investigators Methylenetetrahydrofolate reductase (MTHFR) polymorphisms and risk of molecularly defined subtypes of childhood acute leukemia. Proc. Natl Acad. Sci. USA 98, 4004–4009 (2001).
Franco, R. F., Simões, B. P., Tone, L. G., Gabellini, S. M., Zago, M. A. & Falcão, R. P. The methylenetetrahydrofolate reductase C677T gene polymorphism decreases the risk of childhood acute lymphocytic leukaemia. Br. J. Haematol. 115, 616–618 (2001).
Balta, G., Yuksek, N., Ozyurek, E., Ertem, U., Hicsonmez, G., Altay, C. et al. Characterization of MTHFR, GSTM1, GSTT1, GSTP1, and CYP1A1 genotypes in childhood acute leukemia. Am. J. Hematol. 73, 154–160 (2003).
Krajinovic, M., Lamothe, S., Labuda, D., Lemieux-Blanchard, E., Theoret, Y., Moghrabi, A. et al. Role of MTHFR genetic polymorphisms in the susceptibility to childhood acute lymphoblastic leukemia. Blood 103, 252–257 (2004).
Thirumaran, R. K., Gast, A., Flohr, T., Burwinkel, B., Bartram, C., Hemminki, K. et al. MTHFR genetic polymorphisms and susceptibility to childhood acute lymphoblastic leukemia. Blood 106, 2590–2591 (2005) author reply 2591-2.
Schnakenberg, E., Mehles, A., Cario, G., Rehe, K., Seidemann, K., Schlegelberger, B. et al. Polymorphisms of methylenetetrahydrofolate reductase (MTHFR) and susceptibility to pediatric acute lymphoblastic leukemia in a German study population. BMC Med. Genet. 6, 23 (2005).
Oliveira, E., Alves, S., Quental, S., Ferreira, F., Norton, L., Costa, V. et al. The MTHFR C677T and A1298C polymorphisms and susceptibility to childhood acute lymphoblastic leukemia in Portugal. J Pediatr. Hematol. Oncol. 27, 425–429 (2005).
Zanrosso, C. W., Hatagima, A., Emerenciano, M., Ramos, F., Figueiredo, A., Félix, T. M. et al. The role of methylenetetrahydrofolate reductase in acute lymphoblastic leukemia in a Brazilian mixed population. Leuk. Res. 30, 477–481 (2006).
Reddy, H. & Jamil, K. Polymorphisms in the MTHFR gene and their possible association with susceptibility to childhood acute lymphocytic leukemia in an Indian population. Leuk. Lymphoma. 47, 1333–1339 (2006).
Kim, N. K., Chong, S. Y., Jang, M. J., Hong, S. H., Kim, H. S., Cho, E. K. et al. Association of the methylenetetrahydrofolate reductase polymorphism in Korean patients with childhood acute lymphoblastic leukemia. Anticancer Res. 26, 2879–2881 (2006).
Chatzidakis, K., Goulas, A., Athanassiadou-Piperopoulou, F., Fidani, L., Koliouskas, D. & Mirtsou, V. Methylenetetrahydrofolate reductase C677T polymorphism: association with risk for childhood acute lymphoblastic leukemia and response during the initial phase of chemotherapy in Greek patients. Pediatr. Blood Cancer 47, 147–151 (2006).
Petra, B. G., Janez, J. & Vita, D. Gene-gene interactions in the folate metabolic pathway influence the risk for acute lymphoblastic leukemia in children. Leuk. Lymphoma. 48, 786–792 (2007).
Kamel, A. M., Moussa, H. S., Ebid, G. T., Bu, R. R. & Bhatia, K. G. Synergistic effect of methyltetrahydrofolate reductase (MTHFR) C677T and A1298 polymorphism as risk modifiers of pediatric acute lymphoblastic leukemia. J. Egypt Natl Canc. Inst 19, 96–105 (2007).
Giovannetti, E., Ugrasena, D. G., Supriyadi, E., Vroling, L., Azzarello, A., de Lange, D. et al. Methylenetetrahydrofolate reductase (MTHFR) C677T and thymidylate synthase promoter (TSER) polymorphisms in Indonesian children with and without leukemia. Leuk. Res. 32, 19–24 (2008).
Alcasabas, P., Ravindranath, Y., Goyette, G., Haller, A., Del Rosario, L., Lesaca-Medina, M. Y. et al. 5,10-methylenetetrahydrofolatereductase (MTHFR) polymorphisms and the risk of acute lymphoblastic leukemia (ALL) in Filipino children. Pediatr. Blood Cancer 51, 178–182 (2008).
De Jonge, R., Tissing, W. J., Hooijberg, J. H., Jansen, G., Kaspers, G. J., Lindemans, J. et al. Polymorphisms in folate-related genes and risk of pediatric acute lymphoblastic leukemia. Blood 113, 2284–2289 (2009).
Damnjanovic, T., Milicevic, R., Novkovic, T., Jovicic, O., Bunjevacki, V., Jekic, B. et al. Association between the methylenetetrahydrofolate reductase polymorphisms and risk of acute lymphoblastic leukemia in Serbian children. J. Pediatr. Hematol. Oncol. 32, e148–e150 (2010).
Yeoh, A. E., Lu, Y., Chan, J. Y., Chan, Y. H., Ariffin, H., Kham, S. K. et al. Genetic susceptibility to childhood acute lymphoblastic leukemia shows protection in Malay boys: results from the Malaysia-Singapore ALL Study Group. Leuk. Res. 34, 276–283 (2010).
Tong, N., Fang, Y., Li, J., Wang, M., Lu, Q., Wang, S. et al. Methylenetetrahydrofolate reductase polymorphisms, serum methylenetetrahydrofolate reductase levels, and risk of childhood acute lymphoblastic leukemia in a Chinese population. Cancer Sci. 101, 782–786 (2010).
Sood, S., Das, R., Trehan, A., Ahluwalia, J., Sachdeva, M. U., Varma, N. et al. Methylenetetrahydrofolate reductase gene polymorphisms: association with risk for pediatric acute lymphoblastic leukemia in north Indians. Leuk. Lymphoma. 51, 928–932 (2010).
Sadananda Adiga, M. N., Chandy, S., Ramachandra, N., Appaji, L., Aruna Kumari, B. S., Ramaswamy, G. et al. Methylenetetrahydrofolate reductase gene polymorphisms and risk of acute lymphoblastic leukemia in children. Indian J. Cancer 47, 40–45 (2010).
Lightfoot, T. J., Johnston, W. T., Painter, D., Simpson, J., Roman, E. et al. United Kingdom Childhood Cancer Study Genetic variation in the folate metabolic pathway and risk of childhood leukemia. Blood 115, 3923–3929 (2010).
Karathanasis, N. V., Stiakaki, E., Goulielmos, G. N. & Kalmanti, M. The role of the methylenetetrahydrofolate reductase 677 and 1298 polymorphisms in Cretan children with acute lymphoblastic leukemia. Genet. Test Mol. Biomarkers 15, 5–10 (2011).
Chan, J. Y., Ugrasena, D. G., Lum, D. W., Lu, Y. & Yeoh, A. E. Xenobiotic and folate pathway gene polymorphisms and risk of childhood acute lymphoblastic leukaemia in Javanese children. Hematol. Oncol. 29, 116–123 (2011).
Atashrazm, F., Zaker, F., Aghaeipour, M. & Pazhakh, V. Polymorphisms of the methylene tetrahydrofolate reductase and susceptibility to acute lymphoblastic leukemia in children. Lab. Med. 42, 275–279 (2011).
Nikbakht, M., MalekZadeh, K., Kumar Jha, A., Askari, M., Marwaha, R. K., Kaul, D. et al. Polymorphisms of MTHFR and MTR genes are not related to susceptibility to childhood ALL in North India. Exp. Oncol. 34, 43–48 (2012).
Azhar, M. R., Rahimi, Z., Vaisi-Raygani, A., Akramipour, R., Madani, H., Rahimi, Z. et al. Lack of association between MTHFR C677T and A1298C polymorphisms and risk of childhood acute lymphoblastic leukemia in the Kurdish population from Western Iran. Genet. Test Mol. Biomarkers 16, 198–202 (2012).
Amigou, A., Rudant, J., Orsi, L., Goujon-Bellec, S., Leverger, G., Baruchel, A. et al. Folic acid supplementation, MTHFR and MTRR polymorphisms, and the risk of childhood leukemia: the ESCALE study (SFCE). Cancer Causes Control 23, 1265–1277 (2012).
Silva, R. M., Fontes, A. C., Silva, K. A., Sant'Ana, T. A., Ramos, F. J., Marques-Salles Tde, J. et al. Polymorphisms involved in folate metabolism pathways and the risk of the development of childhood acute leukemia. Genet. Test Mol. Biomarkers 17, 147–152 (2013).
Kim, Y. I. Role of the MTHFR polymorphisms in cancer risk modification and treatment. Future Oncol. 5, 523–542 (2009).
Xing, J., Watkins, W. S., Hu, Y., Huff, C. D., Sabo, A., Muzny, D. M. et al. Genetic diversity in India and the inference of Eurasian population expansion. Genome Biol. 11, R113 (2010).
Pereira, T. V., Rudnicki, M., Pereira, A. C., Pombo-de-Oliveira, M. S. & Franco, R. F. 5,10-Methylenetetrahydrofolate reductase polymorphisms and acute lymphoblastic leukemia risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 15, 1956–1963 (2006).
Wang, J., Zhan, P., Chen, B., Zhou, R., Yang, Y. & Ouyang, J. MTHFR C677T polymorphisms and childhood acute lymphoblastic leukemia: a meta-analysis. Leuk. Res. 34, 1596–1600 (2010).
Vijayakrishnan, J. & Houlston, R. S. Candidate gene association studies and risk of childhood acute lymphoblastic leukemia: a systematic review and meta-analysis. Haematologica 95, 1405–1414 (2010).
Tong, N., Sheng, X., Wang, M., Fang, Y., Shi, D., Zhang, Z. et al. Methylenetetrahydrofolate reductase gene polymorphisms and acute lymphoblastic leukemia risk: a meta-analysis based on 28 case-control studies. Leuk. Lymphoma. 52, 1949–1960 (2011).
Yan, J., Yin, M., Dreyer, Z. E., Scheurer, M. E., Kamdar, K., Wei, Q. et al. A meta-analysis of MTHFR C677T and A1298C polymorphisms and risk of acute lymphoblastic leukemia in children. Pediatr. Blood Cancer 58, 513–518 (2012).
Dietrich, M., Brown, C. J. & Block, G. The effect of folate fortification of cereal-grain products on blood folate status, dietary folate intake, and dietary folate sources among adult non-supplement users in the United States. J. Am. Coll. Nutr. 24, 266–274 (2005).
Skibola, C. F., Smith, M. T., Kane, E., Roman, E., Rollinson, S., Cartwright, R. A. et al. Polymorphisms in the methylenetetrahydrofolate reductase gene are associated with susceptibility to acute leukemia in adults. Proc. Natl Acad. Sci. USA 96, 12810–12815 (1999).
Ma, J., Stampfer, M. J., Giovannucci, E., Artigas, C., Hunter, D. J., Fuchs, C. et al. Methylenetetrahydrofolate reductase polymorphism, dietary interactions, and risk of colorectal cancer. Cancer Res. 57, 1098–1102 (1997).
Acknowledgements
We acknowledge the Indian Council of Medical Research and the Uttar Pradesh Council of Science and Technology for partly sponsoring the study. Nirmalya Roy Moulik is supported by a postdoctoral fellowship from the Indian Council of Medical Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Rights and permissions
About this article
Cite this article
Roy Moulik, N., Parveen, F., Kumar, A. et al. MTHFR gene polymorphism in acute lymphoblastic leukemia among North Indian children: a case–control study and meta-analysis updated from 2011. J Hum Genet 59, 397–404 (2014). https://doi.org/10.1038/jhg.2014.44
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.44
This article is cited by
-
Meta-analysis of polymorphic variants conferring acute lymphoblastic leukemia risk in the Indian population
The Nucleus (2024)
-
Lack of Impact of the A1298C MTHFR on the Risk of Childhood Acute Lymphoblastic Leukemia: Evidence from a Meta-analysis
Indian Journal of Hematology and Blood Transfusion (2022)