Abstract
Pseudomonas aeruginosa is a common cause for healthcare-associated infections, which have been historically treated by antipseudomonal β-lactam agents in the clinical setting. However, P. aeruginosa has evolved to overcome these β-lactam agents via multiple endogenous resistance mechanisms, including derepression of the chromosomal cephalosporinase (AmpC). In this article, we investigated the effective concentration of OP0595 for combination with piperacillin, cefepime or meropenem in in vitro susceptibility tests, and the antibacterial activity of cefepime in combination with OP0595 in both in vitro time-kill studies and in vivo murine thigh infection model study with AmpC-derepressed P. aeruginosa. The sufficient combinational concentration of OP0595 was a 4 μg ml−1 with all these three β-lactam agents. OP0595 increased the antibacterial activity of cefepime in both in vitro and in vivo studies against all strains tested. Taken together, OP0595 is the diazabicyclooctane serine β-lactamase inhibitor with activity against AmpC-derepressed P. aeruginosa and its combinational use with a β-lactam agent will provide a new approach for the treatment of P. aeruginosa infections.
Similar content being viewed by others
Introduction
Pseudomonas aeruginosa is a common cause for healthcare-associated infections including pneumonia, bloodstream infections, urinary tract infections, and surgical site infections.1 To treat P. aeruginosa infections, antipseudomonal β-lactam agents such as piperacillin, ceftazidime, cefepime, imipenem and meropenem have been administered in the clinical setting. However, P. aeruginosa strains have overcome against these β-lactam agents by means of endogenous multiple resistance mechanisms, including derepression of the chromosomal cephalosporinase (AmpC), upregulation of efflux systems, and loss of an outer membrane porin protein. These mechanisms may function in composite and are able to resist all antipseudomonal β-lactam agents.2, 3, 4
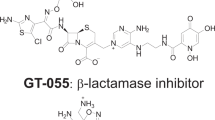
As a result, new approaches to the treatment of infection are hoped, and diazabicyclooctanes including avibactam, relebactam (MK-7655) and OP0595 have been researched.5 Diazabicyclooctanes exhibit strong inhibitory activity against both Class A β-lactamases including KPC types and Class C AmpC enzymes of the Ambler classification, and are expected as a new class of β-lactamase inhibitors.6, 7 Avibactam and relebactam have determined ceftazidime and imipenem as an initial partner β-lactam agent, respectively. Avibactam and relebactam increase the antibacterial activity of partner β-lactam agents against serine β-lactamases producing strains.8, 9, 10, 11
OP0595 acts in three ways: (i) as a β-lactamase inhibitor, (ii) as an antibacterial agent against Enterobacteriaceae, and (iii) as an ‘enhancer’ of the activity of various β-lactam agents differing from avibactam and relebactam.6 However, OP0595 does not show antibacterial activity or enhancer activity toward P. aeruginosa and works only as a β-lactamase inhibitor in this case.12
As a first approach to characterize the efficacy of OP0595 against P. aeruginosa, here its antibacterial activity in combination with β-lactam agents was evaluated to determine the effective concentration of OP0595 for combinatorial use. Then OP0595 was tested in both in vitro time-kill studies and an in vivo murine thigh infection model study. In the latter studies, cefepime was used as a partner β-lactam agent for OP0595.
Materials and methods
Compounds
OP0595 was synthesized by Meiji Seika Pharma Co., Ltd. (Tokyo, Japan) and used as anhydride.6 Antibacterial compounds were obtained from the following sources: piperacillin from Sigma-Aldrich (St Louis, MO, USA); meropenem from United States Pharmacopeial Convention (Rockville, MO, USA); and cefepime from United States Pharmacopeial Convention and GlaxoSmithKline K.K. (Tokyo, Japan).
Bacterial strains
The three strains of AmpC-derepressed P. aeruginosa (MSC17689, MSC17715 and MSC17716) are clinical isolates from Japan and were obtained from the Antimicrobial Susceptibility Surveillance Research Group (Osaka, Japan). The expressions of AmpC under a non-inducible condition were detected by real-time quantitative RT-PCR using the previous method.13 The levels of AmpC in all strains were over 1.5 times higher than that in wild-type P. aeruginosa ATCC 27853 (ATCC, Manassas, VA, USA) and these strains were regarded as AmpC-derepresed strains.14 The strain of P. aeruginosa ATCC 27853 was used for quality control.
Susceptibility testing
The MIC of each compound was determined by broth microdilution according to CLSI guidelines.15, 16 The inoculum size was ~5 × 104 CFU per well. The MIC was determined as the lowest concentration to inhibit the visible growth after incubation at 35 °C for 18 h.
Time-kill experiments
Bactericidal activity was determined with the time-kill method, standardized by CLSI guidelines as follows.17 Well-isolated bacterial colonies were added to cation-adjusted Mueller–Hinton broth (CAMHB; Becton, Dickinson and Company, Franklin Lakes, NJ, USA) and cultured for ~16 h at 35 °C. The cultured bacterial suspensions were diluted with CAMHB and cultured for 2 h, while being shaken at 100 r.p.m. at 35 °C. An aliquot of 4.9 ml of bacterial suspension was added to a test tube and mixed with 0.1 ml of the test compound solution. The suspension was then cultured at 35 °C with shaking at 100 r.p.m. At time points of 0, 2, 4, 6 and 24 h after addition of the test compound, a sample was collected from the culture medium, serially diluted, spread on a Mueller–Hinton agar (MHA; Becton, Dickinson and Company) plate, and cultured at 35 °C. The number of colonies growing on the plate was counted after ~24 h. The detection limit was set at <1.3 log10 CFU ml−1; if no colonies were detected, the value of 1.3 log10 CFU ml−1 was adopted. A bactericidal effect was estimated as a decrease of ⩾3 log10 CFU ml−1 relative to the control sample obtained at 0 h.
Thigh infection model in neutropenic mice
All animal studies and protocols were approved by the Animal Experiment Management Committee of the Pharmaceutical Research Center, and were based on Guidelines on the Management of Animal Experiments established by the Pharmaceutical Research Center, Meiji Seika Pharma Co., Ltd. Four-week-old, specific-pathogen-free, male Crlj:CD1 (ICR) mice (Charles River Laboratories Japan, Inc., Kanagawa, Japan) weighing 18–22 g were used for all the tests. These mice were used because a murine model of thigh infection with P. aeruginosa has been established in this strain.18 The mice were kept in an animal room under controlled conditions (temperature, 21–25 °C; humidity, 50–70%; lighting hours, 07:00–19:00), and allowed to acclimatize for 1 week before the study. During the acclimation and study periods, feed (CRF-1; Oriental Yeast Co., Ltd., Tokyo, Japan) and water were available ad libitum.
The neutropenic mice were fabricated by i.p. administration of cyclophosphamide (Sigma-Aldrich) 4 days before infection (150 mg kg−1 of body weight) and 1 day before infection (100 mg kg−1 of body weight). Six mice per group were infected with P. aeruginosa by an injection into the thigh. The mice were treated by s.c. administration of the test compound at 1, 3 and 5 h after infection, and euthanized 24 h after infection by cervical dislocation. The thigh was then removed and homogenized. Each homogenate was diluted 10-fold serially with physiological saline, and an aliquot of each initial homogenate and dilution series was smeared onto a plate of MHA, which was then cultured at 35 °C. The number of colonies grown on the plate was counted after ~22 h. The detection limit was set at <2.15 log10 CFU per thigh; if no colonies were detected in the initial homogenate, the value of 2.15 log10 CFU per thigh was adopted. The data were expressed as the mean±s.d. log10 CFU per thigh. The number of viable cells was compared between the vehicle and administration groups by using Steel’s test.
Results
Concentration dependency of in vitro antibacterial activity
To determine the effective concentration of OP0595 for use with β-lactam agents, the MICs of piperacillin, cefepime and meropenem in combination with multiple concentrations of OP0595 were determined against three strains of AmpC-derepressed P. aeruginosa, and the geometric mean MICs were plotted (Figure 1). For all β-lactam agents, the geometric mean MICs decreased according to the increase of the OP0595 concentration. The MIC attained a plateau at 4 μg ml−1 of OP0595 in all cases, and the MICs of cefepime-OP0595 were lowest among the three β-lactam agents tested. Collectively, these results suggest that a 4 μg ml−1 of OP0595 is sufficient to show the effective MIC reduction in vitro activities against AmpC-derepressed P. aeruginosa, and one of the optimal partner β-lactam agents for OP0595 is cefepime.
Bactericidal activity against AmpC-derepressed P. aeruginosa
To assess the detailed combinational activity of OP0595 against the antibacterial activity of cefepime, bactericidal activity was tested using three strains of AmpC-derepressed P. aeruginosa.
OP0595 did not show the antibacterial activity at 16 μg ml−1 and cefepime showed weak antibacterial activity against these strains (Table 1). On the other hand, Cefepime-OP0595 showed strong antibacterial activity against them and all the MICs were susceptible concentrations according to the CLSI guidelines.15 In this study, two concentrations of OP0595 were used to evaluate the capacity of its β-lactamase inhibitory activity. The data in Figure 1 indicated that the applicable combinatorial concentration of OP0595 was 4 μg ml−1; therefore, the concentrations of OP0595 were set at 1 and 4 μg ml−1 to compare an insufficient concentration with the applicable concentration. The concentrations of cefepime were set at 8 and 16 μg ml−1, which are the respective susceptible and intermediate concentrations against P. aeruginosa according to the CLSI guidelines. The time-kill curves are shown in Figure 2.
An aliquot of 16 μg ml−1 of cefepime did not decrease the viable cell counts of all the test strains. On the other hand, 16 μg ml−1 of cefepime combined with OP0595 decreased the viable cell counts. In particular, the strong bactericidal effect was observed at 4 μg ml−1 of OP0595 in combination with 16 μg ml−1 of cefepime. All test strains decreased their viable cell counts by 3 log10 CFU ml−1 after 24 h from the counts at 0 h. By contrast, cefepime alone, OP0595 alone and cefepime-OP0595 combination (16 and 1 μg ml−1, respectively) did not show a bactericidal effect against any of the test strains. These results suggested that the bactericidal effect of cefepime was restored by OP0595 that acted as an AmpC inhibitor.
Efficacy in in vivo model
To assess the efficacy of OP0595 in combination with cefepime in vivo, we carried out a study in a neutropenic murine thigh infection model (Figure 3). The strain tested was AmpC-derepressed P. aeruginosa MSC17715, which had been checked to increase in the neutropenic murine thighs. Administration of cefepime alone or OP0595 alone showed the bacterial count in the murine thigh similar to that in the vehicle group. In contrast, combinational administration of cefepime-OP0595 decreased the bacterial count to 2–4 log10 CFU per thigh (P<0.05). These results suggest that OP0595 works as an AmpC inhibitor and OP0595 alone has no antibacterial activity in vivo.
Comparison of the efficacy between sole and combined administration of β-lactam agents in a neutropenic murine model of thigh infection with AmpC-derepressed P. aeruginosa MSC17715. Six mice per group were rendered neutropenic, and 5.36 log10 CFU per mouse of P. aeruginosa MSC17715 was injected into the thigh, followed by s.c. administration of the test compounds at 1, 3 and 5 h after infection. The mean log10 CFU per thigh recovered from the infected thigh after 24 h is shown; error bars represent the s.d. A P-value of <0.05 indicates significance relative to the untreated control (vehicle) and is indicated by a hash (#). FEP, cefepime; TID, three times a day.
Discussion
In this study we have demonstrated that, when used in combination with cefepime, the diazabicyclooctane molecule OP0595 has potency against AmpC-derepressed P. aeruginosa strains in both in vitro time-kill studies and in vivo infection model study.
Recently, the concentrations of β-lactamase inhibitors have been tested at 4 μg ml−1 in combinational studies of ceftolozane–tazobactam, ceftazidime–avibactam, and imipenem–relebactam, among other combinations.5, 9, 19 Against CTX-M-15-positive Escherichia coli and KPC-positive K. pneumoniae strains, the optimal concentration of OP0595 in combination with piperacillin, cefepime or meropenem was 4 μg ml−1.20 Similar results were obtained by our in vitro tests and the sufficient combinational concentration of OP0595 was also 4 μg ml−1 against AmpC-derepressed P. aeruginosa. Interestingly, OP0595 did not affect the antibacterial activity of piperacillin, cefepime and meropenem against P. aeruginosa ATCC 27853, which expresses wild-type levels of AmpC (data not shown),14 indicating that OP0595 functions as an AmpC inhibitor.
OP0595 reduced the MICs of piperacillin and cefepime, but weakly reduced the MIC of meropenem. Piperacillin and cefepime are easily hydrolyzed by AmpC, but meropenem is stable against AmpC activity.21 This is consistent with the results shown in Figure 1. OP0595 inhibits serine-carbapanemase such as KPC, and the meropenem-OP0595 combination is expected to show strong antibacterial activity against KPC-positive P. aeruginosa strains.
To predict the efficacy of OP0595 in humans, in vitro and in vivo pharmacokinetic/pharmacodynamic (PK/PD) studies, such as an in vitro hollow-fiber infection model study using human PK and a murine thigh infection model study using murine PK, are needed. In the case of Enterobacteriaceae, OP0595 works not only as a β-lactamase inhibitor but also as an antibacterial agent and β-lactam enhancer; by contrast, OP0595 works only as a β-lactamase inhibitor against AmpC-derepressed P. aeruginosa, and thus calculations of the PK/PD parameters of OP0595 will be simplified. Currently, combinational PK/PD studies with β-lactam agent and β-lactamase inhibitor, such as ceftolozane–tazobactam, ceftaloline–avibactam and aztreonam–avibactam, have been performed with in vitro and in vivo models.18, 22, 23, 24 For example, an in vitro hollow-fiber model was investigated to detect the effect of β-lactamase inhibitory activity. They used the human PK value of a β-lactam agent and the stationary concentration of a β-lactamase inhibitor. The effects of OP0595 might be clarified in similar studies using AmpC-derepressed P. aeruginosa to establish detailed information for clinical development.
In conclusion, OP0595 has been shown to work as a β-lactamase inhibitor against P aeruginosa and increased the antibacterial activities of cefepime in both in vitro time-kill studies and an in vivo infection model study. These data present that OP0595 has a potential as a new β-lactamase inhibitor to treat P. aeruginosa infections.
References
Centers for Disease Control and Prevention Antibiotic resistance threats in the United States, 2013, (Centers for Disease Control and Prevention, Atlanta, GA, (2013).
Masuda, N. et al. Substrate specificities of MexAB-OprM, MexCD-OprJ, and MexXY-oprM efflux pumps in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 44, 3322–3327 (2000).
Winkler, M. L. et al. Unexpected challenges in treating multidrug-resistant Gram-negative bacteria: resistance to ceftazidime-avibactam in archived isolates of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 59, 1020–1029 (2015).
Castanheira, M., Mills, J. C., Farrell, D. J. & Jones, R. N. Mutation-driven β-lactam resistance mechanisms among contemporary ceftazidime-nonsusceptible Pseudomonas aeruginosa isolates from U.S. hospitals. Antimicrob. Agents Chemother. 58, 6844–6850 (2014).
Watkins, R. R., Papp-Wallace, K. M., Drawz, S. M. & Bonomo, R. A. Novel β-lactamase inhibitors: a therapeutic hope against the scourge of multidrug resistance. Front. Microbiol. 4, 1–8 (2013).
Morinaka, A. et al. OP0595, a new diazabicyclooctane: mode of action as a serine β-lactamase inhibitor, antibiotic and β-lactam ‘enhancer’. J. Antimicrob. Chemother. 70, 2779–2786 (2015).
Bush, K. & Jacoby, G. A. Updated functional classification of β-lactamases. Antimicrob. Agents Chemother. 54, 969–976 (2010).
Zhanel, G. G. et al. Ceftazidime-avibactam: a novel cephalosporin/β-lactamase inhibitor combination. Drugs 73, 159–177 (2013).
Livermore, D. M. et al. Activities of NXL104 combinations with ceftazidime and aztreonam against carbapenemase-producing Enterobacteriaceae. Antimicrob. Agents Chemother. 55, 390–394 (2011).
Hirsch, E. B. et al. In vitro activity of MK-7655, a novel β-lactamase inhibitor, in combination with imipenem against carbapenem-resistant Gram-negative bacteria. Antimicrob. Agents Chemother. 56, 3753–3757 (2012).
Livermore, D. M., Warner, M. & Mushtaq, S. Activity of MK-7655 combined with imipenem against Enterobacteriaceae and Pseudomonas aeruginosa. J. Antimicrob. Chemother. 68, 2286–2290 (2013).
Livermore, D. M., Mushtaq, S., Warner, M. & Woodford, N. Activity of OP0595/β-lactam combinations against Gram-negative bacteria with extended-spectrum, AmpC and carbapenem-hydrolysing β-lactamases. J. Antimicrob. Chemother. 70, 3032–3041 (2015).
Savli, H. et al. Expression stability of six housekeeping genes: a proposal for resistance gene quantification studies of Pseudomonas aeruginosa by real-time quantitative RT-PCR. J. Med. Microbiol. 52, 403–408 (2003).
Tam, V. H. et al. Prevalence of AmpC over-expression in bloodstream isolates of Pseudomonas aeruginosa. Clin. Microbiol. Infect. 4, 413–418 (2007).
Clinical and Laboratory Standards Institute Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Third Informational Supplement M100-S25, (Clinical and Laboratory Standards Institute, Wayne, PA, (2015).
Clinical and Laboratory Standards Institute Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically-Ninth Edition: Approved Standard M7-A10, (Clinical and Laboratory Standards Institute, Wayne, PA, (2015).
Clinical and Laboratory Standards Institute Methods for Determining Bactericidal Activity of Antimicrobial Agents; Approved Guideline M26-A, (Clinical and Laboratory Standards Institute, Wayne, PA, (1999).
Craig, W. A. & Andes, D. R. In vivo activities of ceftolozane, a new cephalosporin, with and without tazobactam against Pseudomonas aeruginosa and Enterobacteriaceae, including strains with extended-spectrum β-lactamases, in the thighs of neutropenic mice. Antimicrob. Agents Chemother. 57, 1577–1582 (2013).
Melchers, M. J., van Mil, A. C. & Mouton, J. W. In vitro activity of ceftolozane alone and in combination with tazobactam against extended-spectrum-β-lactamase-harboring Enterobacteriaceae. Antimicrob. Agents Chemother. 59, 4521–4525 (2015).
Morinaka, A. et al. In vitro and In vivo activities of OP0595, a new diazabicyclooctane, against CTX-M-15-positive Escherichia coli and KPC-positive Klebsiella pneumoniae. Antimicrob. Agents Chemother. 60, 3001–3006 (2016).
Moya, B. et al. Activity of a new cephalosporin, CXA-101 (FR264205), against β-lactam-resistant Pseudomonas aeruginosa mutants selected in vitro and after antipseudomonal treatment of intensive care unit patients. Antimicrob. Agents Chemother. 54, 1213–1217 (2010).
Singh, R. et al. Pharmacokinetics/pharmacodynamics of a β-lactam and β-lactamase inhibitor combination: a novel approach for aztreonam/avibactam. J. Antimicrob. Chemother. 70, 2618–2626 (2015).
Louie, A. et al. Pharmacodynamics of β-lactamase inhibition by NXL104 in combination with ceftaroline: examining organisms with multiple types of β-lactamases. Antimicrob. Agents Chemother. 56, 258–270 (2012).
VanScoy, B. et al. Pharmacokinetics-pharmacodynamics of tazobactam in combination with ceftolozane in an in vitro infection model. Antimicrob. Agents Chemother. 57, 2809–2814 (2013).
Acknowledgements
We thank Professor David M Livermore of University of East Anglia, Dr Takuji Yoshida, Mr Mototsugu Yamada and Mr Nobuyoshi Baba of Meiji Seika Pharma Co., Ltd. for productive discussion. We also thank Dr Tetsuro Muratani and Dr Chikara Nakahama of Antimicrobial Susceptibility Surveillance Research Group for strain provision. We also thank Dr Eiki Shitara of Meiji Seika Pharma Co., Ltd. for productive discussion and compound supply, and Ms. Erumi Murase, Ms. Yumiko Suzuki and Ms. Tomomi Koide for technical assistance with the experiments. This work was internally funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AM, KY, TT, TA, TF, YS, TI: relevant shareholdings-Meiji Holdings, amounting to <10% of portfolio value. All authors are employees of Meiji Seika Pharma Co., Ltd.
Rights and permissions
About this article
Cite this article
Morinaka, A., Tsutsumi, Y., Yamada, K. et al. In vitro and in vivo activities of the diazabicyclooctane OP0595 against AmpC-derepressed Pseudomonas aeruginosa. J Antibiot 70, 246–250 (2017). https://doi.org/10.1038/ja.2016.150
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2016.150