Abstract
Besides small molecules from medicinal chemistry, natural products are still major sources of innovative therapeutic agents for various conditions, including infectious diseases. Here we present the first attempt to design a combination treatment targeted against Chlamydia pneumoniae infection using coadministration of natural phenolics with calcium (Ca2+) modulators, and also the concomitant administration of these compounds with doxycycline. An in vitro acute C. pneumoniae model in human lung epithelial cells was used and Loewe additivity model was applied to evaluate the effects. In general, the phenolic compounds, quercetin, luteolin, rhamnetin and octyl gallate did not improve the antichlamydial effect of doxycycline, and, in some cases, resulted in antagonistic effects. The combination of doxycycline and Ca2+ modulators (isradipine, verapamil and thapsigargin) was at most additive, and at subinhibitory concentrations of doxycycline, often even antagonistic. The Ca2+ modulators showed no inhibitory effects on C. pneumoniae growth alone, whereas the coadminstration of Ca2+ modulators with phenolic compounds resulted in potentiation of the antichlamydial effect of phenolic compounds. Verapamil (100 μM) was synergistic with low quercetin and luteolin concentrations (0.39 and 1.56 μM), whereas 10 μM isradipine was synergistic with high quercetin, rhamnetin and octyl gallate concentrations (12.5 μM and 100 μM). Use of thapsigargin with the phenolic compounds resulted in the most intense synergism. Interaction indices 0.12 and 0.14 were achieved with 0.39 μM luteolin and 10 and 100 nM thapsigargin, respectively. To conclude, the observed results indicate that the Ca2+ modulators potentiate the antichlamydial effects of the phenolic compounds.
Similar content being viewed by others
Introduction
Chlamydia pneumoniae is an intracellular Gram-negative bacterium infecting readily the epithelial and smooth muscle cells, as well as monocytes and macrophages. The bacterium causes acute respiratory tract infections, and is estimated to be responsible for 5–10% of community-acquired pneumonia.1 The persistent infection of C. pneumoniae has been associated with the development of several inflammatory diseases. For example, the association between Chlamydia pneumoniae and atherosclerosis has been indicated by several approaches including in vivo animal studies, seroepidemiological studies in humans, demonstration of the presence of the bacteria in atherosclerotic lesions and atherosclerotic changes in vascular tissue.2, 3, 4, 5
Antimicrobial therapy is heading toward multidrug treatments because microbial resistance toward commonly used antibiotics has increased.6 The multidrug treatment approach has already been used for long against difficult pathogens that typically develop resistance to antibiotics such as Mycobacterium tuberculosis or respond poorly to single-drug treatment such as Helicobacter pylori. Moreover, in serious cases of C. pneumoniae infection, such as Chlamydia-induced arthritis, prolonged treatment with multiple antibiotics has been successfully used.7
Most antibiotics limit infections by inhibiting central microbial biosynthetic pathways, thus having relatively little effect on the metabolically inactive forms of pathogens.8 Occasionally, in vivo antibiotic treatment of acute C. pneumoniae infections with standard clinical doses has failed.9 These treatment failures may promote the development of persistent infection. In fact, some of the first-choice antibiotics, such as doxycycline and rifampicin, have been reported to promote the development of persistent infection at subinhibitory concentrations.10 It has been suggested that C. pneumoniae infection of macrophages is often in a persistent form, which explains the observed refractory behavior of C. pneumoniae infection to antibiotic treatment in cells of monocyte–macrophage line.11, 12 Thus, new treatments are needed to fight the chlamydial infections and avoid the treatment failures.
Calcium (Ca2+) channel blockers have been shown to inhibit the growth of some extracellular and intracellular pathogens and to have combinatory effects with certain antimicrobials.13 High doses of verapamil have been shown to inhibit the growth of Chlamydia,14 and most interestingly, Ca2+ channel blockers have been shown to improve antibiotic susceptibility of persistent C. pneumoniae infection, presumably by reactivating the persistent infection to more easily treatable acute infection.15, 16
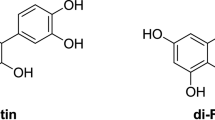
We have previously shown that phenolic compounds, common in our daily food, are potent and valid inhibitors of C. pneumoniae, in vitro and in vivo, even with doses achievable from the nutritional sources.17, 18 Phenolic compounds have been associated with a wide range of biological activities; among others, they have been shown to affect Ca2+ channel regulation in mammalian cells at physiological concentrations. As reviewed by Scholz et al.,19 the type and strength of the effect depends highly on the compound concentration and on the cell and channel type. In our earlier work with rat pituitary GH4C1 cells expressing L-type Ca2+ channels, luteolin and octyl gallate inhibited the uptake of Ca2+ from extracellular media, whereas quercetin increased the uptake, and rhamnetin showed no effect on the Ca2+ ion uptake at a concentration of 20 μg ml−1 (63–71 μM).20 These phenolic compounds sharing good antichlamydial activity, but showing differential Ca2+-modulating activities, were chosen for the current study.
In this study we investigated whether coadministration of doxycycline, Ca2+ modulators and phenolic compounds in appropriate dose could produce a synergistic antimicrobial effect on acute chlamydial infection in vitro. Two clinically used Ca2+ channel blockers were used, isradipine being highly selective inhibitor of L-type Ca2+ channels and verapamil, which is relatively non-selective Ca2+ channel inhibitor. In addition, thapsigargin, a selective inhibitor of the sarco/endoplasmic reticulum Ca2+–ATPase pump was included in the study.
Results
Dose-dependent inhibition of C. pneumoniae growth by single compounds
First, the dose-dependence of the antichlamydial effect of Ca2+ channel blockers, isradipine and verapamil, sarco/endoplasmic reticulum Ca2+–ATPase pump, inhibitor thapsigargin, doxycycline, the three flavonoids quercetin, luteolin and rhamnetin, and an alkyl gallate octyl gallate, were studied in a model for acute C. pneumoniae infection in human lung epithelial (HL) cells.
The treatment of the chlamydial cultures with Ca2+ channel blockers (up to 100 μM concentration) had minor or moderate effects on the number of chlamydial inclusions. Isradipine was the more efficient from the two tested Ca2+ channel blockers in reducing chlamydial growth, as treatment with 10 μM isradipine resulted in 56% inhibition of chlamydial growth, and with 100 μM isradipine, 87% inhibition of number of chlamydial inclusions was achieved, yet this higher concentration also decreased host cell viability to 54%. (Table 1) Verapamil, on the other hand, gave 28% inhibition of chlamydial growth at a concentration of 100 μM, whereas treatment with 10 μM concentration markedly increased the number of chlamydial inclusions. Lower concentrations of verapamil resulted in no significant change in the number of chlamydial inclusions. Thapsigargin showed 53% inhibition at 1 μM concentration, but also decreased HL cell viability at this concentration. Lower thapsigargin concentrations showed no antichlamydial effects.
The treatment of chlamydial cultures with doxycycline, quercetin, luteolin, rhamnetin and octyl gallate resulted in dose-dependent inhibition of chlamydial growth as measured by the number of chlamydial inclusions. Sigmoidal dose–response curves for the antichlamydial effects of doxycycline, the three flavonoids and octyl gallate were obtained (data not shown). The IC50 values determined by the curves were 49 nM (log IC50 −7.3±0.26) for doxycycline, 46 μM (−4.3±0.17) for quercetin, 16 μM (−4.8±0.26) for luteolin, 50 μM (−4.3±0.25) for rhamnetin and 4.2 μM (−5.4±0.18) for octyl gallate.
The inhibition of C. pneumoniae by combinations with doxycycline
Doxycycline (70, 35 and 18 nM) was combined with the three flavonoids and octyl gallate. When combined with quercetin, most samples within the combination treatments gave higher inclusion numbers than untreated controls, resulting in negative inhibition percentages; however, the inhibition values of both doxycycline and quercetin alone were consistent with the obtained dose–response curves. As a result of the negative inhibition values obtained for most of the combinations, the interaction indices (I) calculated for the different doxycycline–quercetin combination showed mostly strong-to-moderate antagonism (I-values >2, in most combinations) (Table 2). However, an I-value of 0.9 was achieved with 70 nM doxycycline + 6.25 μM quercetin combination, indicating an additive effect.
Similar data were obtained when doxycycline was combined with the two other flavonoids, luteolin and rhamnetin. Most of the samples treated with the combinations in different doses resulted in negative inhibition values and thus calculated I-values indicate strong antagonizing effects between the agents. Moreover, doxycycline–octyl gallate combinations showed some negative inhibition; antagonizing or indifferent rather than additive or synergistic effects for all the concentration combinations (Table 2).
The effect of combined treatment of infected cultures with doxycycline and the Ca2+ modulators was investigated, as this issue has earlier been addressed in persistent infection of C. pneumoniae in macrophages.15 In our model of acute C. pneumoniae infection in HL cells, the inhibitory effect of doxycycline (from 0.018 to 0.28 μM) was not markedly increased in the concomitant treatment of isradipine (100, 10, 1 μM), verapamil (100, 10, 1 μM) or thapsigargin (1 μM, 100 or 10 nM). Table 3 presents the inhibition percentages resulting from each of the combinations, together with the I-values calculated for the combinations. As indicated by the I-values, many of the combined inhibitory concentrations of doxycycline and each of the Ca2+ modulators show additive (0.75 < I⩽1.25), however not synergistic (I⩽0.75), effects on inhibition of chlamydial growth. On the other hand, the combinations with subinhibitory concentrations of doxycycline and Ca2+ modulators were often indifferent (1.25<I⩽2) or antagonistic (I-values >2).
The inhibition of C. pneumoniae by natural phenol and Ca2+ modulator combinations
The effect of combining the phenolic compounds with Ca2+ modulators were studied in similar experiments by titrating the effect of each phenolic compounds with 100, 10 and 1 μM isradipine or verapamil, or with 1 μM, 100 nM and 10 nM thapsigargin. Majority of the combinations with 100 μM isradipine lowered the host cell viability below 2/3 of control and thus those results are not presented.
When quercetin and rhamnetin were assayed with 10 μM isradipine, I-values of approximately 0.5 were achieved in the presence of 50 μM of 100 μM rhamnetin and quercetin. Thus, 10 μM isradipine functioned synergistically with the high polyphenol concentrations. Furthermore, 1 μM isradipine, which showed no antichlamydial effect when administered alone, was able to potentiate the antichlamydial effect of 100 and 50 μM of quercetin and rhamnetin. In the case of isradipine–luteolin combinations, increased numbers of chlamydial inclusions compared with untreated controls, resulting in negative inhibition values, were seen for most concentration combinations (Table 4). Thus, the I-values for these combinations gave values higher than 2 and were classified as antagonistic effects. Antagonism was also seen in most of the isradipine–octyl gallate combinations.
Changing the Ca2+ channel blocker from isradipine to verapamil resulted in somewhat similar results, however, with some exceptions in the case of quercetin. When the highest verapamil concentration (100 μM) was combined with 0.39 and 1.56 μM luteolin, I-values of 0.52 and 0.58 were achieved, indicating that these agents have a moderate synergistic effect in the antichlamydial assay. Verapamil (100 μM) was moderately synergistic also with 1.56 μM quercetin (I-value 0.63). Lower verapamil concentrations (10 and 1 μM) resulted in negative inhibition values (up to threefold number of chlamydial inclusion compared with untreated controls) independent of luteolin, quercetin (except for 100 μM) or rhamnetin concentration present in the assay media. Moreover, in the case of verapamil and octyl gallate combinations, the counts were up to fourfold compared with untreated controls, and thus heavy or moderate antagonism was indicated for all concentration combinations.
The antichlamydial effect of the three flavonoids was potentiated by thapsigargin. Thapsigargin (10 and 100 nM), having no antichlamydial effect alone, resulted in I-values of 0.45 and 0.82, with 6.25 μM quercetin and I-values of 0.53 and 0.63 with 50 μM quercetin, respectively. Furthermore, 10 and 100 nM thapsigargin were also able to strongly potentiate the antichlamydial effect of 0.39 μM luteolin, providing I-values of 0.12 and 0.14, respectively. Furthermore, 100 nM thapsigargin moderately potentiated the inhibition of C. pneumoniae growth when combined with 25, 50 or 100 μM rhamnetin, showing I-values of 0.3–0.7. The beneficial effects on inhibition of C. pneumoniae were less prone in the combinations of thapsigargin with octyl gallate.
Discussion
Plant polyphenolic compounds, such as flavonoids, are ubiquitous in most edible plants especially tea, onion, apple, berries and grapes. They are important metabolites of plants in defense against radiation and microorganisms.21 So far, most of the antibacterial agents from nature have been derived from microbial resources, but plant metabolites deserve consideration in this respect for at least two reasons. First, plants have exceptional ability to produce cytotoxic agents and second there is an ecological rationale that antimicrobial natural products should be present or plants following microbial attack to protect the producer from pathogenic microbes in its environment.22 We have previously shown that dietary phenolic compounds are effective against the intracellular bacterium C. pneumoniae.17, 18 As it has been proposed that natural compounds in combination with antibiotics could be a new strategy for developing therapies for infections caused by bacterial species and that natural plant products can potentiate the activity of antibiotics in combination,23, 24 we wanted to investigate whether coadministration of phenolic compounds with the antichlamydial compound doxycycline results in synergistic inhibition of acute C. pneumoniae infection. The combinations of natural phenols and doxycycline did not improve antichlamydial activity compared with the activity of compounds alone, except for 100 μM rhamnetin, where additive and synergistic effects were received. However, lower concentrations of rhamnetin slightly diminished the antichlamydial effect of doxycycline. Quercetin, luteolin and octyl gallate clearly antagonized the activity of doxycycline in most of the concentration combinations. These in vitro results of the observed antagonism between doxycycline and natural phenols might give further support to the current user recommendations to avoid simultaneous intake of doxycycline with food.
The Ca2+ channel inhibitors have been shown to be of value in antimicrobial therapy by interacting with antimicrobial compounds and helping to prevent resistance.14, 25, 26 Azenabor et al.16 demonstrated that an L-type Ca2+ channel blocker, nifedipine, may enhance the antichlamydial effect of doxycycline in persistent infection cell model. Nifedipine treatment of macrophages infected with C. pneumoniae downregulated chlamydial hsp60 mRNA expression and upregulated major outer membrane protein expression, thus shifting the infection toward a form, which is more susceptible to antibiotic treatment. The authors concluded that the combination therapy using antibiotics and Ca2+ channel blockers should be evaluated for the treatment of chlamydial diseases. In our study, the combination of doxycycline and Ca2+ modulators against acute infection of C. pneumoniae in HL cells was at most additive and at subinhibitory concentrations of doxycycline often antagonistic.
C. pneumoniae has been shown to affect the cellular Ca2+ homeostasis in different ways. In C. pneumoniae-infected macrophages L-type Ca2+ channels are activated and intracellular Ca2+ concentrations are increased.27 The entry of chlamydiae has been shown to cause redistribution of cellular Ca2+ stores in HeLa cells.28, 29 Local high Ca2+ concentrations and Ca2+-binding protein accumulate in the proximity of chlamydial aggregates and they are pivotal for the proper formation of chlamydial inclusions. In a recent microarray study by Alvesalo et al.,30 expression levels of genes associated with regulation of Ca2+ homeostasis were significantly changed by C. pneumoniae infection in HL cells. The results presented in the current work indicate that Ca2+ modulators alone have only a minor effect on acute C. pneumoniae infection in HL cells, or in the case of verapamil, may even increase the number of chlamydial inclusions.
When studying phenolic compounds and Ca2+ modulators, more antagonistic combinations were found than synergic or additive combinations. However, 10 μM isradipine was synergistic with high quercetin and rhamnetin concentrations (100 μM and 50 μM), whereas in the presence of low quercetin/rhamnetin concentrations, the combinations increased the inclusion counts. Verapamil (100 μM) was synergistic with low quercetin and luteolin concentrations, but unfortunately, compromised cell viability limits the use of higher polyphenol concentrations. Although thapsigargin had no antichlamydial effect on its own, it was able to potentiate the growth inhibitory effect of quercetin, luteolin and rhamnetin on C. pneumoniae.
To summarize our results, monotherapy with Ca2+ modulators was not inhibitory on chlamydial growth. Verapamil (10 and 1 μM) increased the number of C. pneumoniae inclusions in the acute infection model, and this effect was generally not reversed by inhibitory concentrations of the phenolic compounds. However, verapamil did not abolish the antichlamydial effect of doxycycline. High concentrations of quercetin and rhamnetin combined with isradipine and thapsigargin showed clear positive effects on the inhibition of C. pneumoniae, whereas other combinations of Ca2+ modulators and phenolic compounds only occasionally resulted as improved inhibition.
To conclude, high degree of dose dependence was associated with the observed effects in all cases. The coadminstration of Ca2+ modulators with phenolic compounds resulted in synergistic inhibition of C. pneumoniae growth, whereas combination of these with doxycycline resulted in additive effects at best. Coadministration of phenolic compounds with doxycycline provided no marked beneficial effects. The present study suggest on the potential usefulness of phenolic compounds and Ca2+ modulators in combination for combating infections caused by this pathogen.
Materials and methods
Cell lines
HL cell line was used as host cells for the C. pneumoniae infection. The cells were grown as described in Salin et al.31 Briefly, the culture medium consisted of RPMI 1640 supplemented with 7.5% fetal bovine serum and 2 mM L-glutamine, all purchased from BioWhittaker, Lonza (Basel, Switzerland) and with 20 μg gentamycin (Fluka, Buchs, Switzerland) per ml. Cells were cultured to confluence in culture flasks (Greiner, Bio-One, Frickenhausen, Germany) in standard cell culture conditions (37°C, 5% CO2 and 95% humidity). The Chlamydia strain used was a sequenced ATCC strain CWL-029 (VR-1310) and was grown and purified as described in Alvesalo et al.17
Compounds
The natural compounds, luteolin and rhamnetin were purchased from Extrasynthese (Genay, France), quercetin from Carl Roth GmbH (Karlsruhe, Germany) and octyl gallate from Fluka. Doxycycline was from ICN Biomedicals (Aurora, OH, USA) and verapamil and isradipine from Sigma-Aldrich (St Louis, MO, USA). Thapsigargin was a generous gift from Professor Kid Törnquist at Abo Akademi University, Turku, Finland. All stock solutions were made in DMSO (Mallinckrodt Baker, Phillipsburg, NJ, USA) at a concentration of 100 mM, except for doxycycline (0.56 mM) and thapsigargin (1 mM).
Antichlamydial assays
The antichlamydial assays were performed by an immunofluorescence method on a 24-well plate, quantifying the number of chlamydial inclusions in infected HL cells using a Chlamydia-specific anti-LPS antibody, as described earlier in Salin et al.31and Keurulainen et al.32
The antichlamydial effect of compound combinations was assayed by using a checkerboard method, with a single replicate.33 Combinations were chosen, based on the activity results from dose–response experiments for single agents, and on each of the combination plates, the compounds were also present alone.
Cell viability assays
The effect of different concentrations of single compounds (n=3) and the studied combinations in different concentrations (n=1 for each concentration combination) on the host cell viability was determined using the luminescent ATP level determination method as described in Salin et al.31 All chemical treatments were well tolerated by the host cells (67% viability or higher of DMSO-treated control), unless otherwise stated in the text or tables.
Data analysis
All antichlamydial results represent mean and s.e.m. values from the number of replicates indicated for each experiment. The sigmoidal dose response curves and the IC50 values were determined by fitting the data from experiments with concentration series into nonlinear regression models using the GraphPad Prism software version 5.0. (GraphPad Software, Inc., La Jolla, CA, USA) For the analysis of concomitant administration of the chemical agents, Loewe model for additivity was applied by calculating the I-values for each combined dose. The equation for calculating I was as follows:

where D1 and D2 represent the concentrations of compounds in the combination, and DX1 and DX2 represent the concentrations of the drugs alone giving similar response.
References
Kuo, C. C., Jackson, L. A., Campbell, L. A. & Grayston, J. T. Chlamydia pneumoniae. Clin. Microbiol. Rev. 8, 451–461 (1995).
Rassu, M. et al. Demonstration of Chlamydia pneumoniae in atherosclerotic arteries from various vascular regions. Atheroscerosis 158, 73–79 (2001).
Cao, F., Castrillo, A., Tontonoz Re, F. & Byrne, G. I. Chlamydia pneumoniae-induced macrophage foam cell formation is mediated by Toll-like receptor 2. Infect. Immun. 75, 753–759 (2007).
Blessing, E., Campbell, L. A., Rosenfeld, M. E., Chough, N. & Kuo, C. C. Chlamydia pneumoniae infection accelerates hyperlipidemia induced atherosclerotic lesion development in C57BL/6J mice. Atherosclerosis 158, 13–17 (2001).
Volanen, I. et al. Increased aortic intima-media thickness in 11-year-old healthy children with persistent Chlamydia pneumoniae seropositivity. Arterioscler. Thromb. Vasc. Biol. 26, 649–655 (2006).
Kohanski, M., Dwyer, D. & Collins, J. J. How antibiotics kill bacteria: from targets to networks. Nat. Rev. Microbiol. 8, 423–435 (2010).
Carter, J. D. et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis. Arthritis. Rheum. 62, 1298–1307 (2010).
Kutlin, A., Roblein, P. M. & Hammerschlag, M. R. Effect of prolonged treatment with azithromycin, clarithromycin or levofloxacin on Chlamydia pneumoniae in a continuous-infection model.. Antimicrob. Agents Chemother. 46, 409–412 (2002).
Grayston, J. T. Infections caused by Chlamydia pneumoniae strain TWAR. Clin. Infect. Dis. 15, 757–763 (1992).
Gieffers, G., Rupp, J., Gebert, A., Solbach, W. & Klinger, M. First-choice antibiotics at subinhibitory concentrations induce persistence of Chlamydia pneumoniae.. Antimicrob. Agents Chemother. 48, 1402–1405 (2004).
Bellman-Weiler, R. et al. Divergent modulation of Chlamydia pneumoniae infection cycle in human monocytic and endothelial cells by iron, tryptophan availability and interferon gamma. Immunobiology 215, 842–848 (2010).
Gieffers, G. et al. Chlamydia pneumoniae infection in circulating human monocytes is refractory to antibiotic treatment. Circulation. 103, 351–356 (2001).
Mazumdar, K., Kumar, K. A. & Dutta, N. K. Potential role of the cardiovascular non-antibiotic (helper compound) amlodipine in the treatment of microbial infections: scope and hope for the future. Int. J. Antimicrob. Agents 36, 295–302 (2010).
Shainkin-Kestenbaum, R., Winikoff, Y., Kol, R., Chaimovizt, C. & Sarov, I. Inhibition of growth of Chlamydia trachomatis by the calcium antagonist verapamil. J. Gen. Microbiol. 135, 1619–1623 (1989).
Azenabor, A. A. & Chaudhry, A. U. Macrophage L-type Ca2+ channel antagonists alter Chlamydia pneumoniae MOMP and HSP-60 mRNA gene expression, and improve antibiotic susceptibility. Immunobiology 207, 237–245 (2003).
Azenabor, A. A. Treatment of chronic bacterial infections Pat. Pub. No: WO 2005/007082. International Application No.: PCT/US2004/016780.
Alvesalo, J., Vuorela, H., Tammela, P., Leinonen, M., Saikku, P. & Vuorela, P. Inhibitory effect of dietary phenolic compounds on Chlamydia pneumoniae in cell cultures. Biochem. Pharmacol. 71, 735–741 (2006).
Törmäkangas, L. et al. In vivo treatment of acute Chlamydia pneumoniae infection with the flavonoids quercetin and luteolin and an alkyl gallate, octyl gallate, in a mouse model. Biochem. Pharmacol. 70, 1222–1230 (2005).
Scholz, E. P., Zitron, E., Katus, H. A. & Carle, C. A. Cardiovascular ion channels as a molecular target of flavonoids. Cardiovasc. Ther. 28, 46–52 (2010).
Summanen, J. et al. Effects of simple aromatic compounds and flavonoids on Ca2+ fluxes in rat pituitary GH4C1 cells. Eur. J. Pharmacol. 414, 125–133 (2001).
Cushnie, T. P. T. & Lamb, A. G. Antimicrobial activity of flavonoids. Int. J. Antimicrob. Agents 26, 343–356 (2005).
Gibbons, S. Plants as a source of bacterial resistance modulators and anti-infective agents. Phytochem. Rev. 4, 63–78 (2005).
Lewis, K. & Ausubel, F. M. Prospects for plant-derived antibacterial. Nat. Biotechnol. 24, 1504–1507 (2006).
Jayaraman, P., Sakharkar, M. K., Lim, C. S., Tang, T. H. & Sakharkar, K. R. Activity and interactions of antibiotic and phytochemical combinations against Pseudomonas aeruginosa in vitro. Int. J. Biol. Sci. 6, 556–568 (2010).
Liebermann, L. A. & Higgins, D. E. Inhibition of Listeria monocytogenes infection by neurological drugs. Int. J. Antimicrob. Agents 35, 292–296 (2010).
Gunics, G., Motohasi, N., Amaral, L., Farkas, S. & Molnár, J. Interaction between antibiotics and non-conventional antibiotics on bacteria. Int. J. Antimicrob. Agents 14, 239–242 (2000).
Azenabor, A. & Chaudry, A. Effective macrophage redox defence against Chlamydia pneumoniae depends on L-type Ca2+ channel activation. Med. Microbiol. Immunol. 192, 99–106 (2003).
Majeed, M., Krause, K.- H., Clark, R., Kihlström, E. & Stendahl, O. Localization of intracellular Ca2+ stores in HeLa cells during infection with Chlamydia trachomatis. J. Cell Sci. 112, 35–44 (1999).
Majeed, M., Ernst, J., Magnusson, K.- E., Kihlström, E. & Stendahl, O. Selective translocation of annexins during intracellular redistribution of Chlamydia trachomatis in HeLa and McCoy cells. Infect. Immun. 62, 126–134 (1994).
Alvesalo, J. et al. Microarray analysis of a Chlamydia pneumoniae–infected human epithelial cell line by use of gene ontology hierarchy. J. Infect. Dis. 197, 156–162 (2008).
Salin, O. et al. Inhibitory effect of the natural product betulin and its derivatives against the intracellular bacterium Chlamydia pneumoniae. Biochem. Pharmacol. 80, 1141–1151 (2010).
Keurulainen, L. et al. Design and synthesis of 2-arylbenzimidazoles and evaluation of their inhibitory effect against Chlamydia pneumoniae. J. Med. Chem. 53, 7664–7674 (2010).
How, S. J., Hobson, D., Hart, A. C. & Webster, R. E. An in vitro investigation of synergy and antagonism between antimicrobials against Chlamydia trachomatis. J. Antimicrob. Chemother. 15, 533–538 (1985).
Acknowledgements
We acknowledge the Sigrid Juselius Foundation, Tor, Joe och Pentti Borgs Minnesfond Foundation and the Finnish Cultural Foundation (Elli Turunen) for financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salin, O., Pohjala, L., Saikku, P. et al. Effects of coadministration of natural polyphenols with doxycycline or calcium modulators on acute Chlamydia pneumoniae infection in vitro. J Antibiot 64, 747–752 (2011). https://doi.org/10.1038/ja.2011.79
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2011.79