Abstract
The in vivo-mimic assay system using silkworm larvae was used as a screening tool to discover antibiotics against methicillin-resistant Staphylococcus aureus (MRSA). Microbial culture broths were screened in this in vivo-mimic assay system and a culture broth of Streptomyces sp. K04-0144 was selected. New antibiotics, designated nosokomycins A–D, were isolated from the culture broth by HP-20 and ODS column chromatography and HPLC. Nosokomycins inhibited the growth of MRSA with MIC values of 0.125 μg ml−1 using the liquid microdilution method. Furthermore, MRSA-infected silkworms survived when nosokomycin A or B was injected at a dose of 50 μg per larva.
Similar content being viewed by others
Introduction
Animal models using mammals such as mice, rats, rabbits, dogs and monkeys have been used for in vivo studies of the development of clinical drugs. However, such studies have several problems; namely, high costs, ethical issues and so on. Furthermore, it is very difficult to use such in vivo models as a primary screening system for the discovery of new antibiotics. Recently, a number of researchers have focused on nonmammalian animals such as zebrafish,1 Caenorhabditis elegans,2 Drosophila melanogaster3 and silkworms4, 5, 6 as alternative in vivo models. Sekimizu et al.4, 5 proposed an alternative method using silkworm larvae (silkworm assay) for evaluating the in vivo efficacy of antibiotics. In this silkworm assay, when silkworm larvae were infected with various human pathogenic microorganisms, including methicillin-resistant Staphylococcus aureus (MRSA), they died within several days of infection. On the other hand, when clinically used antibiotics were injected into such infected larvae, they survived, indicating that the efficacy of various antibiotics can be evaluated by this method.4, 5 These findings prompted us to incorporate the silkworm assay as a tool for the screening of microbial culture broths for anti-MRSA antibiotics. We predicted that new antibiotics that are effective in in vivo systems would be more efficiently discovered by the silkworm assay than by the agar diffusion assay using paper disks. Using the silkworm assay, screening was performed to identify culture broths that caused MRSA-infected silkworm larvae to survive until at least 3 days after infection. The anti-MRSA activity of such culture broths was also tested using the agar diffusion assay.
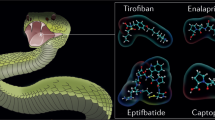
A culture broth of Streptomyces sp. K04-0144, which was previously reported as a cyslabdan-producing actinomycete,7, 8 showed anti-MRSA activity in the silkworm assay. During the process used to purify the active components, the fractions showing anti-MRSA activity were the same as those found in the agar diffusion assay. Thus, activity-guided purification led to the discovery of four new compounds, designated as nosokomycins A (1)–D (4) (Figure 1). The structure elucidation of nosokomycins is reported in an accompanying paper.9 In this study, the fermentation, isolation and biological properties of nosokomycins are described.
Results
Time course of nosokomycin production by fermentation
The production of nosokomycins started on day 3 after inoculation. The concentrations reached a maximal level (nosokomycin A, 2.7 mg l−1; B, 2.8 mg l−1; C, 1.5 mg l−1; D, 1.8 mg l−1) on day 4 and then gradually decreased on day 6 (data not shown). Structurally related moenomycin A10 was not observed in the culture broth by HPLC analysis.
Isolation
The procedure for the isolation of nosokomycins from the culture broth is summarized in Figure 2. The 6-day-old culture broth (50 l) was centrifuged with a Sharpless centrifugal separator (Kokusanseikou Co., Kanagawa, Japan) to obtain the supernatant. The supernatant was then passed through a column containing previously activated Diaion HP-20 resin (100ø × 200 mm, Mitsubishi Chemical Co., Tokyo, Japan). After being washed with water (1500 ml), the active materials were eluted with methanol (1500 ml), which was concentrated in vacuo to dryness to yield a brown material (32 g). The material was dissolved in water and then partitioned by EtOAc to remove the antifoaming agent. Next, the water layer was concentrated in vacuo to dryness to yield a brown material (27.2 g), and this material (15 g) was dissolved in a small amount of water and applied to an ODS column (50ø × 280 mm, Pegasil ODS, Senshu Scientific, Tokyo, Japan) that had been previously equilibrated with 40% aq. methanol. After being washed with 40 and 50% aq. methanol (1500 ml), the active materials were eluted with 60% aq. methanol (1500 ml), and the eluent was concentrated in vacuo to dryness to yield a brown material (450 mg), which was dissolved in a small amount of methanol and purified by HPLC under the following conditions: column, Pegasil ODS (20ø × 250 mm); mobile phase, 50% acetonitrile/10 mM CH3COONH4 (pH 3, adjusted with HCOOH); flow rate, 8 ml min−1; detection, UV 210 nm. The retention times of the active fractions containing 1–4 were 21, 24, 33 and 37 min, respectively (Figure 3a). These fractions were neutralized by NH4OH and concentrated to remove acetonitrile. After each aqueous solution had been partitioned with EtOAc to remove impurities, the water layer was concentrated in vacuo to dryness to afford enriched 1 (34 mg) as a pale brown material, pure 2 (71.4 mg) as a white powder, enriched 3 (11.2 mg) as a pale brown material and pure 4 (19.4 mg) as a white powder. Compounds 1 and 3 were further purified by preparative HPLC under the following conditions: column, Pegasil ODS (20ø × 250 mm); mobile phase, 46% acetonitrile/10 mM KH2PO4 (pH 4.7); flow rate, 8 ml min−1; detection, UV 210 nm. Under these conditions, 1 and 3 were eluted for retention times of 21 min (Figure 3b) and 27 min (Figure 3c), respectively. Each fraction was collected and treated in the same way as described above to yield pure 1 (15.7 mg) and 3 (5.6 mg) as white powders.
Anti-MRSA activities of nosokomycins
Compounds 1–4 and vancomycin had potent anti-MRSA activity by the agar diffusion method, with inhibition zones of 27, 25, 23, 22 and 16 mm at 10 μg/6 mm disk, respectively. Their anti-MRSA activity was confirmed by the liquid microdilution method. All compounds had MIC values of 0.125 μg ml−1 (Table 1). Under the same conditions, vancomycin and imipenem had MIC values of 0.5 and 16 μg ml−1, respectively. Therefore, in two in vitro assays, nosokomycins had more potent activity against MRSA than vancomycin.
Furthermore, 1, 2 and vancomycin were evaluated by the silkworm method. In the absence of an antibiotic, MRSA-infected silkworms died within 3 days. However, when 1, 2 or vancomycin (50 μg per larva) was injected into silkworms after infection, the silkworms survived for more than 3 days. Thus, 1 and 2 proved to be effective as anti-MRSA agents, as did vancomycin in the in vivo-mimic silkworm assay.
Other antimicrobial activities of nosokomycins
The antimicrobial activities of nosokomycins are summarized in Table 2. The nosokomycins had potent anti-Gram-positive activity and weak anti-Gram-negative bacterial activity at 10 μg/6 mm disk; they showed no antimycoplasma, antifungal or antiyeast activity.
Discussion
New antibiotic nosokomycins were isolated from the culture broth of Streptomyces sp. K04-0144, which also produced cyslabdan, a potentiator of imipenem activity against MRSA.7, 8 Thus, this strain produced two kinds of compounds with completely different structures in the same culture broth, demonstrating the high potential of actinomycetes for producing new diverse metabolites.
In this study, an in vivo-mimic MRSA-infection assay using silkworm larvae was used as the primary screening method for anti-MRSA antibiotics, and nosokomycins were discovered. Thus, it is expected that the application of this in vivo-mimic assay as a primary screening system will enable us to more efficiently select practically useful new antibiotics. The anti-MRSA activity of each fraction obtained in the purification process from the culture broth was evaluated using the silkworm assay and the agar diffusion assay. Anti-MRSA activity was found in the same fractions in both assays, resulting in the discovery of four nosokomycins. Nosokomycins showed very potent anti-MRSA activity with MIC values of 0.125 μg ml−1. Furthermore, nosokomycin A was also found to be effective in an in vivo system using a mouse model (data not shown). As described in the accompanying study,9 nosokomycins are structurally related to moenomycins10 (Figure 1). Nosokomycin B is identical to the semisynthetic moenomycin A derivative,11 which lacks the chromophoric cyclopentenone moiety. Furthermore, nosokomycins A and B were recently reported to be biosynthetic intermediates of moenomycin A in a comprehensive set of genetic and enzymatic experiments that illuminated the moenomycin biosynthetic pathway.12 In this study, nosokomycins were discovered as potential end products using the silkworm larvae system to detect anti-MRSA compounds.
Moenomycins are known to inhibit the transglycosylase of penicillin-binding protein, which is involved in bacterial cell-wall biosynthesis. Recently, two research groups reported the crystal structure of penicillium-binding protein13, 14 and demonstrated that moenmycin A is bound to the active site of transglycosylase in penicillin-binding protein. Moenomycin A has been practically used as a growth promoter in animal feed.15
Methods
Strains
Streptomyces sp. K04-0144, which was isolated from a soil sample from Ishigakijima Island, Okinawa, Japan,7 was used to produce nosokomycins. MRSA K21 was clinically isolated at Juntendo University Hospital, Tokyo, Japan. The microorganisms used for the paper disk method were as follows: Bacillus subtilis PCI 219, S. aureus FDA 209P, Micrococcus luteus PCI 1001, Mycobacterium smegmatis ATCC 607, Escherichia coli NIHJ, Pseudomonas aeruginosa P-3, Xanthomonas campestris pv. Oryzae KB 88, Bacteroides fragilis ATCC 23745, Acholeplasma laidlawii PG 8, Pyricularia oryzae KF 180, Aspergillus niger ATCC 6275, Mucor racemosus IFO 4581, Candida albicans ATCC 64548 and Saccharomyces cerevisiae.
Fermentation
Strain K04-0144 was grown and maintained on an agar slant consisting of 1.0% starch, 0.3% NZ amine, 0.1% yeast extract, 0.3% meat extract, 1.2% agar and 0.3% CaCO3 (adjusted to pH 7.0 before sterilization). A loopful of Streptomyces sp. K04-0144 spores were inoculated into 100 ml of seed medium consisting of 2.4% starch, 0.1% glucose, 0.3% peptone, 0.3% meat extract, 0.5% yeast extract and 0.4% CaCO3 (adjusted to pH 7.0 before sterilization) in 500-ml Erlenmeyer flasks. The inoculated flasks were then incubated in a rotary shaker (210 r.p.m.) at 27 °C for 3 days.
For the production of nosokomycins, the seed culture (500 ml) was transferred to a 90-l jar fermenter containing 50 l of the production medium consisting of 0.5% glucose, 0.5% corn steep powder (Marcor Development Corporation, Carlstadt, NJ, USA), 1.0% oat meal (Nippon Food Manufacture, Hokkaido, Japan), 1.0% pharmamedia (Sanko Junyaku, Tokyo, Japan), 0.5% K2HPO4, 0.5% MgSO4·7H2O, 5.0 × 10−4% FeSO4·7H2O, 5.0 × 10−4% MgCl2·4H2O, 5.0 × 10−4% CuSO4·5H2O and 5.0 × 10−4% CoCl2·6H2O (adjusted to pH 7.0 before sterilization), and fermentation was carried out with agitation at 200 r.p.m. at 27 °C in an air flow of 5 l min−1 for 6 days.
Quantitative analysis of nosokomycins by HPLC
The amount of nosokomycins was measured by analytical HPLC (photo diode array 996 system, Waters Corp., Milford, MA, USA). Samples dissolved in methanol were analyzed under the following conditions: column, Pegasil ODS (ø4.6 × 250 mm, Senshu Scientific); mobile phase, 50% CH3CN/5 mM heptanesulfonic acid–0.05% H3PO4; column temperature, 40 °C; flow rate, 1.0 ml min−1; detection, UV at 210 nm. Nosokomycins A–D were eluted at retention times of 21, 20, 29 and 30 min, respectively.
Assay for anti-MRSA activity
Silkworm assay
Fertilized silkworm eggs of Bombyx mori (Hu·Yo × Tukuba·Ne) were purchased from Ehime Sansyu, Ehime, Japan.4, 5 Hatched larvae were raised by feeding them with an artificial diet (Silk Mate 2S, Nihon Nosan Kogyo, Kanagawa, Japan) in an incubator at 27 °C until they had developed into forth-molted larva. On the first day of fifth-instar larvae, the silkworms were fed for 1 day with an antibiotic-free artificial diet (Silk Mate, Katakura Industries, Saitama, Japan). On the second day, a test sample (a culture broth or known antibiotic in 10% DMSO) was injected into the hemolymph through the dorsal surface of the silkworm using a disposable 1-ml syringe with a 27-G needle (TERUMO, Tokyo, Japan). Immediately after the sample injection, MRSA K-24 (2.5 × 107 CFU in 50 μl Luria Bertani medium containing 10% NaCl) was injected into the hemolymph. When they were maintained in an incubator at 27 °C, all MRSA-infected silkworm larvae died within 3 days. Under these conditions, when vancomycin (50 μg per larva, Wako Pure Chemical Industries, Osaka, Japan) was injected as a test sample, all silkworms survived. For screening, five MRSA-infected silkworms per sample were used, and samples that caused more than three silkworms to survive after 3 days were selected.
Agar diffusion method
MRSA was cultured in Mueller–Hinton broth (BD Difco, Sparks, MD, USA) at 37 °C for 20 h and adjusted to 1 × 108 CFU ml−1. The inoculum (100 μl) was spread on Mueller–Hinton agar medium in a plate (10 × 14 cm, Eiken Chemical, Tokyo, Japan) containing Mueller–Hinton broth and 1.5% agar (Shimizu Shokuhin, Shizuoka, Japan). Paper disks (Advantec, Tokyo, Japan) containing a sample (10 μg) were placed on the Mueller–Hinton agar plate and incubated at 37 °C for 20 h. Anti-MRSA activity was expressed as the diameter (mm) of the inhibitory zone on the Mueller–Hinton agar plate.
Liquid microdilution method
After Mueller–Hinton broth (90 μl) was added to each well of a 96-well microtiter plate (Corning Inc., Corning, NY, USA), a sample dissolved in methanol (5 μl) was added.9 Finally, MRSA (5 μl) was added at a concentration of 1 × 107 CFU ml−1. Microtiter plates were incubated at 37 °C for 20 h without shaking. MIC was defined as the lowest sample concentration at which MRSA was unable to grow.
Assay of antimicrobial activity
The antimicrobial activity against 14 microorganisms was measured by the agar diffusion method using paper disks.16
References
Zon, L. I. & Peterson, R. T. In vivo drug discovery in the zebrafish. Nat. Rev. Drug Discov. 4, 35–44 (2005).
Kwok, T. C. Y. et al. A small-molecule screen in C. elegans yields a new calcium channel antagonist. Nature 441, 91–95 (2006).
Needham, A. J., Kibart, M., Crossley, H., Ingham, P. W. & Foster, S. J. Drosophila melanogaster as a model host for Staphylococcus aureus infection. Microbiology 150, 2347–2355 (2004).
Kaito, C., Akimitsu, N., Watanabe, H. & Sekimizu, K. Silkworm larvae as an animal model of bacterial infection pathogenic to humans. Microb. Pathog. 32, 183–190 (2002).
Hamamoto, H. et al. Quantitative evaluation of the therapeutic effects of antibiotics using silkworms infected with human pathogenic microorganisms. Antimicrob. Agents Chemother. 48, 774–779 (2004).
Orihara, Y. et al. A silkworm-baculovirus model for assessing the therapeutic effects of antiviral compounds: characterization and application to the isolation of antivirals from traditional medicines. J. Gen. Virol. 89, 188–194 (2008).
Fukumoto, A. et al. Cyslabdan, a new potentiator of imipenem activity against methicillin-resistant Staphylococcus aureus, produced by Streptomyces sp. K04-0144. I. Taxonomy, fermentation, isolation and structure elucidation. J. Antibiot. 61, 1–6 (2008).
Fukumoto, A. et al. Cyslabdan, a new potentiator of imipenem activity against methicillin-resistant Staphylococcus aureus, produced by Streptomyces sp. K04-0144 II. Biological activities. J. Antibiot. 61, 7–10 (2008).
Uchida, R., Iwatsuki, M., Kim, Y. P., Ōmura, S. & Tomoda, H. Nosokomycins, new antibiotics, discovered in an in vivo-mimic infection model using silkworm larvae. II. Structure elucidation. J. Antibiot. 63, 157–163 (2010).
Wallhaeusser, K. H., Nesemann, G., Praeve, P. & Strigler, A. Moenomycin, a new antibiotic. I. Fermentation and isolation. Antimicrob. Agents Chemother. 1965, 734–736 (1965).
Marzan, S. et al. Moenomycin A: reactions at the lipid part. New structure-activity relations. Tetrahedron 50, 5299–5308 (1994).
Ostash, B. et al. Complete characterization of the seventeen step moenomycin biosynthetic pathway. Biochemistry 48, 8830–8841 (2009).
Lovering, A. L., de Castro, L. H., Lim, D. & Strynadka, N. C. Structure insight into the transglycosylation step of bacterial cell-wall biosynthesis. Science 315, 1402–1405 (2007).
Yuan, Y. et al. Crystal structure of a peptidoglycan glycosyltransferase suggests a model for processive glycan chain synthesis. Proc. Natl Acad. Sci. USA 104, 5348–5353 (2007).
Huber, G. Moenomycin and related phosphorus-containing antibiotics. in Antibiotics, Vol. 5, part 1 (ed. Hahn, F. E.) 135 (Springer, New York, 1979).
Koyama, N. et al. Stemphones, novel potentiators of imipenem activity against methicillin-resistant Staphylococcus aureus, produced by Aspergillus sp. FKI-2136. J. Antibiot. 58, 695–703 (2005).
Acknowledgements
This study was supported in part by a Grant-in Aid for Scientific Research 21310146 (to HT) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan and by a grant from the Uehara Memorial Foundation of Japan (to HT). We thank Dr H Hanaki for providing us with the MRSA K24 clinical strain.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uchida, R., Iwatsuki, M., Kim, YP. et al. Nosokomycins, new antibiotics discovered in an in vivo-mimic infection model using silkworm larvae. I: Fermentation, isolation and biological properties. J Antibiot 63, 151–155 (2010). https://doi.org/10.1038/ja.2010.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2010.9
Keywords
This article is cited by
-
New liposidomycin congeners produced by Streptomyces sp. TMPU-20A065, anti-Mycobacterium avium complex agents with therapeutic efficacy in a silkworm infection model
The Journal of Antibiotics (2024)
-
A novel silkworm infection model with fluorescence imaging using transgenic Trichosporon asahii expressing eGFP
Scientific Reports (2020)
-
Pharmacokinetic parameters explain the therapeutic activity of antimicrobial agents in a silkworm infection model
Scientific Reports (2018)
-
Anti-Rhizopus activity of tanzawaic acids produced by the hot spring-derived fungus Penicillium sp. BF-0005
The Journal of Antibiotics (2018)
-
An invertebrate infection model for evaluating anti-fungal agents against dermatophytosis
Scientific Reports (2017)