Abstract
Our aim was to evaluate whether the serum level of galectin-1 (Gal-1) at 18–24 and 27–31 weeks of gestation is a risk factor for predicting the later occurrence of not only preeclampsia (PE) but also gestational hypertension (GH). We measured serum levels of soluble fms-like tyrosine kinase 1 (sFlt-1), placental growth factor (PlGF), and Gal-1 using an enzyme-linked immunosorbent assay in 81 and 73 normal pregnant women, 22 and 16 women with a later onset of GH, and 37 and 29 women with a later onset of PE at 18–24 and 27–31 weeks, respectively. We also measured Gal-1 in 33 women with GH and 78 women with PE after the onset. The levels of Gal-1 after the onset of GH, late-onset PE (onset at ⩾34 weeks), and early-onset PE (onset at <34 weeks) were significantly higher than those in normal pregnant women at 27–31 weeks. However, the low levels of Gal-1 (<8.1 ng ml−1) at 18–24 weeks, but not at 27–31 weeks, predicted the later occurrence of not only early-onset PE and late-onset PE but also GH. The low level of Gal-1 at 18–24 weeks was an independent risk factor for the later occurrence of GH and PE, after adjusting for the effects of a high BP and increased sFlt-1/PlGF ratio at 18–24 weeks. In conclusion, the serum level of Gal-1 is a novel risk factor for both GH and PE, specifically its expression at a low level in the second trimester and a high level after onset.
Similar content being viewed by others
Introduction
Preeclampsia (PE) and gestational hypertension (GH) are associated with preterm delivery, intrauterine fetal death and increased maternal morbidity/mortality.1, 2 However, the risk factors associated with the occurrence of GH are very limited.3, 4, 5, 6, 7, 8, 9, 10, 11, 12 High blood pressure levels in the first and/or second trimesters are well-known risk factors for not only PE but also GH,13, 14, 15 and a past history of PE and/or GH is a risk factor for both PE and GH.16 While uterine artery Doppler (UAD) in the first and/or second trimesters is associated with the onset of PE,17 its association with the onset of GH is very weak or absent.3, 7, 10, 18, 19 Although the serum soluble fms-like tyrosine kinase 1/placental growth factor (sFlt-1/PlGF) ratio and soluble endoglin levels mildly to moderately predict the subsequent occurrence of PE,20 their correlation with the onset of GH is weak.6, 10, 21 In a longitudinal study from the first to third trimesters, maternal flow-mediated dilatation was enhanced in women with GH compared with normal pregnancy, while it was suppressed in women with PE compared with normal pregnancy.6 Thus, PE and GH may be separate clinical entities, resulting in difficulty in predicting GH using prediction models.10, 11, 12 For example, a prediction model for GH using only maternal characteristics and blood pressure level did not provide clinically useful power, because the sensitivity was very low and the positive likelihood ratio was <10.12 Therefore, a more powerful model including new biomarkers for predicting GH is needed.
Galectin-1 (Gal-1) is a carbohydrate-binding protein with many major functions.22 Gal-1 is differentially expressed by several tissues and shows a wide range of biological activity.22 Gal-1 regulates healthy gestation. Gal-1 is implicated in the processes of implantation, decidualization and recruitment of uterine natural killer cells. Gal-1 supports the maternal adaptation to pregnancy in the modulation of cross-regulatory interactions between uterine natural killer cells and dendritic cells in the early pregnancy decidua. The differentiation into syncytiotrpohoblas from cytotrophoblast is accompanied by a loss of Gal-1 expression, whereas the extravillous trophoblast arising from the cytotrophoblast displays increased Gal-1 expression. In addition, Gal-1 appears to be implicated in pregnancy-associated angiogenesis by selective binding to neuropilin-1 to promote the adhesion and migration of endothelial cells.23
Although galectins are known to constitute a galectin family including 19 members, of which at least 13 are expressed in human tissues,24 circulating levels of Gal-1, galectin 7 and galectin 13 (placental protein 13) have been shown to be significantly correlated with the later occurrence of PE.25, 26, 27 Serum levels of Gal-1 were also increased in women with HELLP syndrome.28 Recently, the serum levels of Gal-1 in the second trimester were reported to be significantly decreased in women with a later occurrence of PE, although the levels of Gal-1 after the onset of PE were significantly increased.25 Gal-1 has a proangiogenic function through vascular endothelial growth factor receptor-2 signaling by directly binding to neuropilin-1.29 The blocking of Gal-1 induced a spontaneous PE-like syndrome with intrauterine fetal growth restriction in mice,25 suggesting that Gal-1 is essential for a normal pregnancy. In addition, Gal-1-expressing peripheral blood T and NK cells are markedly lower in women with PE than in normal pregnant women in the third trimester.30, 31 Circulating levels of Gal-1 may be lower in women with gestational diabetes mellitus in the second and third trimesters than in normal pregnant women.31 However, to the best of our knowledge, there has been no study reporting that the decreased level of Gal-1 in the second trimester is a risk factor for the occurrence of not only PE but also GH or that the level of Gal-1 is an independent risk factor for the occurrence of PE/GH after adjusting for other risk factors. In addition, there have been few studies investigating the relationship between the level of Gal-1 in the early third trimester and the later occurrence of PE/GH.30
Our first aim was to evaluate whether the serum level of Gal-1 at 18–24 and 27–31 weeks of gestation is a risk factor that predicts the later occurrence of not only PE but also GH. Our second aim was to evaluate whether a decreased level of Gal-1 at 18–24 weeks of gestation is an independent risk factor for the occurrence of PE/GH after adjusting for the effects of blood pressure (BP) levels in the second trimester and the serum sFlt-1/PlGF ratio at 18–24 weeks of gestation. The main findings of our work is that the serum level of Gal-1 was a novel risk factor for both GH and PE, specifically its expression at a low level at 18–24 weeks, but not at 27–31 weeks, and a high level after onset.
Methods
Subjects and procedures
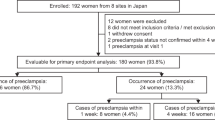
In 2004, we planned a prospective cohort study to evaluate maternal characteristics, BP, UAD and blood biomarkers after approval from the Ethics Committee of our institute. BP levels were measured at every maternal checkup. UAD was measured twice at 16–19 and 20–23 weeks of gestation, and the mean pulsatility index (mPI) was calculated. Blood samples were collected at 18–24 and 27–31 weeks. In the prospective cohort study, 1724 pregnant women with a singleton pregnancy who sought an antepartum maternal checkup before 24 weeks of gestation provided written informed consent between April 2004 and October 2008. Serum levels of sFlt-1, PlGF and Gal-1 were measured in 100 consecutive pregnant women at 6–13, 18–24, 27–31 and 33–38 weeks, respectively. However, seven samples at 6–13 weeks were duplicated, three samples were taken at ⩾14 weeks, one sample was from a twin pregnancy, and eight women delivered at other centers; three women with sampling at 18–24 weeks later developed gestational proteinuria, and eight women delivered at other centers; one sample at 27–31 weeks was duplicated, nine women with sampling at 27–31 weeks later developed GH, PE or gestational proteinuria, three samples were taken at <27 or ⩾32 weeks, six women delivered at other centers, and two samples were not measured because of an insufficient volume; and six women with sampling at 33–38 weeks later developed GH, PE or gestational proteinuria, one sample was taken at ⩾39 weeks, five women delivered at other centers, and one sample was not measured because of an insufficient volume. Therefore, we used 81, 89, 79 and 87 samples at 6–13, 18–24, 27–31 and 33–38 weeks, respectively, as samples from normal pregnant women. The serum levels of sFlt-1, PlGF and Gal-1 were also measured in 37 and 29 samples at 18–24 and 27–31 weeks, respectively, in women with a later occurrence of PE and 22 and 16 women at 18–24 and 27–31 weeks, respectively, in women with a later occurrence of GH. In addition, we measured Gal-1 after the onset of disease in 33 women with GH, 41 women with late-onset PE, and 37 women with early-onset PE.
BP measurement
Details of the BP measurement were reported previously.17 In brief, systolic BP (SBP) and diastolic BP (DBP) were measured with an Omron HEM-906 automated digital oscillometric sphygmomanometer (OMRON Healthcare, Kyoto, Japan), which was located in the waiting room. Each pregnant woman measured her BP by herself during every routine antenatal medical checkup while sitting in a chair after a 1–2-min rest, without conversation during measurement. Omron HEM-906 has been validated by OMRON Healthcare for use by non-pregnant adults in Japan (unpublished data). The mean value of the two readings of SBP and DBP at 16–23 weeks of gestation was documented for each participant. A high BP was defined as when SBP/DBP was ⩾120/80 mm Hg, according to our previous results.5
Measurements of PlGF, sFlt-1 and Gal-1
Blood samples centrifuged at 4 °C at 2500 r.p.m. for 15 min were stored at −20 °C until use. Enzyme-linked immunosorbent assays (ELISAs) for human sFlt-1 (DVR100B, R&D Systems, Minneapolis, MN, USA) and PlGF (DPG00, R&D Systems, Minneapolis, MN, USA) were performed according to the manufacturer’s instructions. In this study, we reused the data of sFlt-1 and PlGF that had been published in our previous manuscript.5 An ELISA for human Gal-1 (DGAL10, R&D Systems, Minneapolis, MN, USA) was also performed according to the manufacturer’s instructions. The Gal-1 ELISA was performed with freshly thawed serum samples.
Cutoff levels of the mPI and serum levels of sFlt-1, PlGF, sFlt-1/PlGF ratio and Gal-1
Details of the gestational age-specific reference ranges for mPI and the serum levels of sFlt-1, PlGF, and the sFlt-1/PlGF ratio were published previously.32, 33, 34 In brief, high mPI was defined as mPI ⩾90th percentile, high sFlt-1 as ⩾95th percentile, low PlGF as <5th percentile, and high sFlt-1/PlGF ratio as ⩾95th percentile.32, 33, 34 Data on angiogenesis-related factors were previously used to evaluate the screening and diagnostic performances of those indices for the clinical manifestation of PE and GH.10, 33, 34 Low Gal-1 was defined as <8.1 ng ml−1, with the threshold determined by the receiver-operating characteristic curve for analyzing the relationship between the serum levels of Gal-1 at 18–24 weeks and the later occurrence of PE, using 81 samples at 18–24 weeks in normal pregnant women and 37 samples at 18–24 weeks in those with a later occurrence of PE.
Definitions of PE, GH and small-for-gestational-age infant
We defined GH and PE according to the definition and classification of pregnancy-induced hypertension (2004) of the Japan Society for the Study of Hypertension in Pregnancy.35, 36 In brief, GH was defined as hypertension without proteinuria occurring after 20 weeks but resolving by 12 weeks postpartum. PE was defined as hypertension with proteinuria occurring after 20 weeks but resolving by 12 weeks postpartum. Superimposed PE includes the following three conditions: (1) chronic hypertension diagnosed before pregnancy or by 20 weeks, with which proteinuria emerges after 20 weeks; (2) aggravations of either or both hypertension and proteinuria in women with preexisting hypertension and proteinuria after 20 weeks; and (3) hypertension emerging after 20 weeks in patients with preexisting renal diseases that solely manifest proteinuria. In this study, superimposed PE was included in the category of PE. Hypertension was defined as when the systolic blood pressure was ⩾140 mm Hg and/or diastolic blood pressure was ⩾90 mm Hg. Proteinuria was defined as 300 mg per day from 24-h urine collection. If only urinary dipstick testing was available, repeated semiquantitative test results of 2+ were considered to constitute a positive result. When PE occurred at <34 weeks, we defined it as early-onset PE, and when PE occurred at ⩾34 weeks, we defined it as late-onset PE.37 We defined a small-for-gestational-age infant as having a birth weight below the 10th percentile for the Japanese population.38
Statistics
The data are presented as the mean±s.d. or the mean±s.e.m. as appropriate. For serum sFlt-1 and PlGF levels and the sFlt-1/PlGF ratio, statistical testing was conducted after logarithmic transformation. For the comparisons of risk factors among normal pregnant women, those with GH, late-onset PE, and early-onset PE, we selected complete data with both serum levels of Gal-1 at 18–24 weeks and the sFlt-1/PlGF ratio at 18–24 weeks. Therefore, the number of normal pregnant women at 18–24 weeks decreased from 89 to 81. We also selected complete data with both serum levels of Gal-1 at 27–31 weeks and the sFlt-1/PlGF ratio at 27–31 weeks. Therefore, the number of normal pregnant women at 27–31 weeks decreased from 79 to 73. Analysis of variance (ANOVA) was used to compare the multiple groups with continuous variables, followed by multiple comparisons with Bonferroni’s test. The chi-squared test was used to compare the categorical data, followed by multiple comparisons with Bonferroni’s test. Univariate and multivariate logistic regression analyses were used. As the numbers of the outcomes of GH or PE were a maximum of 24, the adjusting risk factors were restricted to only three: serum levels of Gal-1, the sFlt-1/PlGF ratio, and a high BP. The positive and negative likelihood ratios (LR+ and LR-, irrespectively) and 95% CIs were calculated using the CONFIDENCE INTERVAL CALCULATOR (created by Rob Herbert at The University of Sydney).39 LR+ ⩾10 was considered clinically useful.40, 41 All analyses were performed using IBM SPSS Statistics (version 21 for Windows) and R commander (EZR ver. 1.32).42 P<0.05 was considered significant.
Results
In normal pregnant women with blood sampling at 6–13, 18–24, 27–31, and 33–38 weeks of gestation, the serum Gal-1 levels were 6.2±0.5 (mean±s.e.m.), 11.9±0.3, 10.5±0.3, and 12.8±0.3 ng ml−1, respectively (Figure 1). In normal pregnant women, the serum level of Gal-1 at 18–24 weeks was significantly higher than that at 6–13 weeks. The level of Gal-1 at 27–31 weeks was slightly but significantly lower than that at 18–24 weeks. In contrast, the level of Gal-1 at 33–38 weeks was significantly higher than that at 27–31 weeks.
For GH, late-onset PE and early-onset PE after the onset of these diseases, the sampling periods in women with early-onset PE were similar to those in the normal pregnancy control with blood sampling at 27–31 weeks (mean: 29.6 vs. 29.0 weeks, respectively), and the sampling periods in women with GH and late-onset PE were similar to those in the normal pregnancy control with blood sampling at 33–38 weeks (mean: 36.5 and 36.4 vs. 37.1 weeks, respectively) (Supplementary Table S1). In women with blood sampling after the onset of GH, late-onset PE and early-onset PE, the serum Gal-1 levels were 23.8±2.9, 22.5 ±1.8 and 16.6±1.3 ng ml−1, respectively (Figure 2). The levels of Gal-1 after the onset of GH, late-onset PE, and early-onset PE were significantly higher than those in the controls at 27–31 weeks. The levels after the onset of GH and late-onset PE were also significantly higher than those in controls at 33–38 weeks. The level of Gal-1 after the onset of early-onset PE was significantly lower than that after the onset of GH and after the onset of late-onset PE, whereas the level of Gal-1 after the onset of GH was almost identical to that after the onset of late-onset PE. The delivery methods did not affect the serum levels of Gal-1 in normal controls and women with GH, late-onset PE and early-onset PE (Supplementary Table S2).
Serum levels of Gal-1 (ng ml−1) in normal pregnant women at 27–31 and 33–38 weeks of gestation (wk), those with gestational hypertension (GH), late-onset preeclampsia (PE), and early-onset PE. The levels of Gal-1 for women with GH, late-onset PE, and early-onset PE were measured soon after the onset of disease. The mean±s.e.m. and dot plots with the median for each group are shown.
For the nested case-control study with blood sampling at 18–24 weeks of gestation, in women with GH and early-onset PE, the frequency of obesity was significantly higher than that in normal pregnant women (controls) (Table 1). In women with GH, late-onset PE, and early-onset PE, the SBP and DBP were significantly higher than in controls, and the frequency of a high BP (SBP ⩾120 and/or DBP ⩾80) was significantly higher than in controls. In women with early-onset PE, the frequency of abnormal UAD was significantly higher than in controls. Women with both late- and early-onset PE delivered by cesarean section more frequently than controls. In women with early-onset PE, preterm delivery was significantly more frequent, the gestational week at delivery was significantly earlier, and the birth weight was significantly lower than in controls.
The serum levels of Gal-1 at 18–24 weeks in normal pregnancy (n=81), later occurrence of GH (n=22), late-onset PE (n=24) and early-onset PE (n=13) were 12.0±0.3, 9.6±0.9, 10.0±1.0, and 12.0±2.8, respectively (ANOVA, P=0.053) (Supplementary Figure S1). The levels of Gal-1 at 27–31 weeks in normal pregnancy (n=73), later occurrence of GH (n=16), late-onset PE (n=21) and early-onset PE (n=8) were 10.6±0.3, 10.6±0.63, 11.2±0.9 and 12.5±2.3, respectively, and there were no differences among the 4 groups (ANOVA, P=0.340) (Supplementary Figure S2). Interestingly, when the screening performance of serum levels of Gal-1 at 18–24 weeks and 27–31 weeks was evaluted using receiver-operating characteristic curves, the serum level of Gal-1 at 18–24 weeks showed a significantly larger area under the curve for the later occurrence of PE, although the serum level of Gal-1 at 27–31 weeks did not have sufficient power to predict the later occurrence of PE (Figure 3). The best cutoff value for the serum level of Gal-1 at 18–24 weeks was 8.1 ng ml−1.
Receiver-operating characteristic curve for evaluating the screening performances of the serum levels of Gal-1 at 18–24 weeks of gestation (wk) (left panel) and 27–31 wk (right panel) for predicting the later occurrence of PE. The area under the receiver-operating characteristic curve and the 95% confidence interval (CI) of Gal-1 at 18–24 wk for predicting PE was significantly larger, but that at 27–31 wk was not. The arrow indicates the best cutoff level of Gal-1 at 18–24 wk, which yielded a sensitivity of 33% and specificity of 98% for the later occurrence of late-onset PE and a sensitivity of 46% and specificity of 98% for the later occurrence of early-onset PE.
For the occurrence of GH, obesity, a high BP, and low level of Gal-1 at 18–24 weeks were risk factors, although a high sFlt-1/PlGF ratio was not a risk factor (Table 2). For the occurrence of late-onset PE, a high BP, high sFlt-1/PlGF ratio at 18–24 weeks, and low level of Gal-1 at 18–24 weeks were risk factors. For the occurrence of early-onset PE, a past history of PE/GH, obesity, chronic hypertension, a high BP, an abnormal UAD at 16–23 weeks, a high sFlt-1/PlGF ratio at 18–24 weeks, and low level of Gal-1 at 18–24 weeks were risk factors. Notably, the LR+s of a low level of Gal-1 at 18–24 weeks for predicting GH, late-onset PE and early-onset PE were all >10.
As the frequencies of obesity in women with a later occurrence of GH and early-onset PE were significantly higher than in controls, we investigated the effect of obesity on the serum level of Gal-1 at 18–24 weeks and on the frequency of low Gal-1 levels (<8.1 ng ml−1) at 18–24 weeks. In all women, the serum level of Gal-1 was not significantly different between women with and without obesity; in addition, the frequency of a low Gal-1 level was not significantly different between these women (Supplementary Table S3). The results were similar even for separate analyses of normal pregnant women and those with GH, late-onset PE or early-onset PE.
In the multivariate logistic regression model for predicting GH, a high BP and low level of Gal-1 at 18–24 weeks were independent risk factors, although a high sFlt-1/PlGF ratio at 18–24 weeks was not a risk factor (Table 3). For predicting late-onset PE, a high BP and low level of Gal-1 at 18–24 weeks were independent risk factors, and a high sFlt-1/PlGF ratio was not an independent risk factor. For predicting early-onset PE, a high BP, low level of Gal-1 at 18–24 weeks, and high sFlt-1/PlGF ratio at 18–24 weeks were all independent risk factors.
Discussion
In this nested case-control study, we found several novel findings. First, the levels of Gal-1 in women with GH, late-onset PE and early-onset PE after the onset of disease were higher than in normal pregnant women at 27–31 weeks. Second, the low levels of Gal-1 at 18–24 weeks predicted the later occurrence of not only early- and late-onset PE but also GH. Third, a low level of Gal-1 at 18–24 weeks was an independent risk factor for the later occurrence of GH, late-onset PE and early-onset PE, after adjusting for the effects of a high BP and an increased sFlt-1/PlGF ratio. Fourth, in normal pregnant women, the level of Gal-1 was increased from 6–13 to 18–24 weeks but slightly decreased from 18–24 to 27–31 weeks, with a further increase from 27–31 to 33–38 weeks. Our results can be summarized as follows: early-onset PE can be predicted using serum levels of the sFlt-1/PlGF ratio and Gal-1 at around 20 weeks; in addition, late-onset PE and GH may be predicted using the serum level of Gal-1 at around 20 weeks, suggesting that the measurement of Gal-1 at around 20 weeks can be used to detect pregnant women with a high risk of the later occurrence of hypertensive disorders of pregnancy.
The level of Gal-1 was higher in the order of normal pregnant women at 27–31 weeks< early-onset PE after the onset of PE<late-onset PE or GH after the onset of PE/GH. This finding is slightly different from the report of Freitag et al.25 Those authors reported that the level of Gal-1 in late-onset PE was higher than in normal pregnant controls, but the level of Gal-1 in early-onset PE was not different from that in normal pregnant controls.25 Placental expression of Gal-1 is decreased in women with early-onset PE but upregulated in women with late-onset PE.25, 43, 44 These data do not contradict our findings on the circulating levels of Gal-1 in women with late- and early-onset PE because the serum level of Gal-1 in women with early-onset PE was significantly lower than in those with late-onset PE. These previous data of placental expression of Gal-1 in early- and late-onset PE suggest a maladaptation in women with early-onset PE to the increase of Gal-1, which occurs in cases of GH or late-onset PE. In other words, a sufficient increase in Gal-1 may inhibit the progression from GH to early-onset PE or may delay the occurrence of PE.
The low level of Gal-1 at 18–24 weeks predicted the later occurrence of not only early- and late-onset PE but also GH. Freitag et al.25 reported for the first time that the level of Gal-1 in the second trimester in women with a later occurrence of PE was significantly lower than that in normal healthy pregnant controls. In our data, the level of Gal-1 in the second trimester was not different between normal pregnant women and those with a later occurrence of early/late-onset PE. However, interestingly, the frequency of low Gal-1 in the second trimester was significantly higher in women with a later occurrence of either late- or early-onset PE than in normal pregnant women. In normal pregnant women, the frequency of low Gal-1 in the second trimester was only 2%, whereas that in late- and early-onset PE was 33% and 46%, respectively. In addition, the frequency of low Gal-1 for those with GH in the second trimester was also higher than in controls (36% vs. 2%, respectively). These results clearly suggest that low Gal-1 levels in the second trimester may be involved in the generation of hypertensive disorders of pregnancy.
Why were low serum levels of Gal-1 in the second trimester implicated in the later occurrence of PE or GH? Although we do not know the reasons for our data, we speculate that in women with a later occurrence of PE/GH, maternal immune adaptation to fetal antigen might fail due to low levels of Gal-1. Gal-1 has important effects that facilitate maternal immune tolerance of the fetus by promoting dendritic cells and regulatory T cells30, 45 and the apoptosis of alloreactive T cells.46 Blocking of Gal-1 induced a spontaneous PE-like syndrome with intrauterine fetal growth restriction in mice,25 suggesting that the failure to produce Gal-1 in the placenta is key during the development of PE. Another possibility is that spiral remodeling might be impaired due to low production of Gal-1 in extravillous trophoblasts, because the extravillous trophoblast arising from the cytotrophoblast displays increased Gal-1 expression.23 In women with PE, failure of the extra-trophoblast invasion of the uterine spiral arteries is often observed.47, 48, 49, 50
We, for the first time, report that a low level of Gal-1 in the second trimester is independently associated with the later occurrence of hypertensive disorders of pregnancy, after adjusting for the effects of a high BP and high sFlt-1/PlGF ratio. In our previous studies, a high BP ⩾120/80 mm Hg in the second trimester was a risk factor for the later occurrence of both GH and PE,5 and a high sFlt-1/PlGF ratio was a risk factor for all PE and early-onset PE, but not GH.10 Interestingly, in the current analysis, although a high sFlt-1/PlGF ratio at 18–24 weeks of gestation was not an independent risk for the later occurrence of GH or late-onset PE, a low level of Gal-1 was a strong risk factor for GH and late-onset PE, with an LR+ ⩾10. As both a high BP and low level of Gal-1 at 18–24 weeks were independent risk factors for the occurrence of GH and late-onset PE, the combination of BP levels and measurement of the serum level of Gal-1 in the second trimester may improve the positive predictive value for narrowing down the candidates with a high risk for the later occurrence of hypertensive disorders of pregnancy. We previously demonstrated that the serial selection of a high BP, low PlGF level, and high sFlt-1 level for predicting the imminent onset of PE markedly improved the positive predictive value while retaining sensitivity.51 However, to test the above-mentioned hypothesis, we would need to measure the level of Gal-1 at 18–24 weeks in all normal pregnant women in our cohort.
The level of Gal-1 in normal pregnant women decreased from the second trimester to the early third trimester. This finding was slightly different from the report by Tirado-Gonza′lez et al.52 They compared the serum Gal-1 level in women with normal pregnancy collected at the first, second and the third trimesters. The level of Gal-1 was measured by in-house ELISA, the level of Gal-1 in the third trimester was higher than that in non-pregnant women, and the level of Gal-1 in the second trimester was higher than that in the first trimester. However, the level of Gal-1 in the second trimester was almost identical to that in the third trimester. In our data, the decrease in Gal-1 from 18–24 weeks (second trimester) to 27–31 weeks (around early third trimester) was significant, although the difference in the means between 18–24 and 27–31 weeks was only 1.4 ng ml−1 (12% decrease). Interestingly, in our current data, the levels of Gal-1 in women with early and late-onset PE and GH were significantly higher than those in controls at 27–31 weeks. Thus, we speculate that the serum level of Gal-1 in normal pregnancy might decrease from the second trimester to the early third trimester, while that for women with a later occurrence of hypertensive disorders of pregnancy might increase from the second trimester to the early third trimester. If this hypothesis is true, the increase in the level of Gal-1 from the second trimester to early third trimester might be useful for predicing PE and GH. To test this hypothesis, we need to evaluate whether the net difference in serum level of Gal-1 between 18–24 and 27–31 weeks can be used to predict the later occurrence of PE using sufficient paired data at 18–24 and 27–31 weeks in our cohort.
This study had several limitations. First, when we compared the previous work on Gal-1 systemic levels in normal pregnant women, the levels were markedly different among reports. Tirado-Gonza′lez et al.52 reported that the serum Gal-1 levels at 9–12, 18–20, and 37–41 weeks were ~30, 70, and 70 ng ml−1, respectively; Molvarec et al.30 reported that the level at 32–38 weeks was ~50 ng ml−1; thus, our results for the serum levels of Gal-1 at 6–13, 18–24, 27–31, and 33–38 weeks were all lower (<30 ng ml−1) than the data in previous reports. The difference among these studies might be due to differences in ethnicity. Although pregnant women with the combination of the absence of killer immunoglobulin receptors (KIRs) genotype AA in the mother and the presence of human leukocyte antigen (HLA)-C group 2 in the fetus have increased risk of PE, the KIR-AA and HLA-C2 frequencies are very different among races. Japanese people have the highest frequency of KIR-AA alleles and the lowest frequency of HLA-C2 alleles, wheraas Caucasians have a moderate frequency of the KIR-AA and HLA-C2 alleles.53 As the incidence of PE in Japanese is relatively low,8 the characteristics of the KIR-AA and HLA-C2 frequencies in Japanese individuals might be related to the low serum levels of Gal-1 in Japanese people. Alternatively, this finding might be due to the different ELISA kits. Although we used a commercially available ELISA kit, Tirado-Gonza′lez et al.52 and Molvarec et al.30 used in-house ELISA kits. Therefore, it is considered that the differences in the reference ranges in normal pregnant women between studies were due to the lack of standardization of Gal-1 measurement. If Gal-1 levels are measured by the same commercially available kits in a future study, differences in the levels due to ethnicity may be revealed. Another possibility for the lower levels of Gal-1 in our data might be the storage of serum for almost 10 years at −20 °C. Second, we did not measure the local Gal-1 levels. We did not collect placental samples in this cohort study.
In conclusion, we demonstrated that a low serum level of Gal-1 in the second trimester is an independent risk factor for not only late- and early-onset PE, but also GH, after adjusting for the effects of a high BP and high sFlt-1/PlGF ratio in the second trimester. As the established independent risk factors predicting the later occurrence of GH are relatively limited, in contrast to those for PE, the measurement of Gal-1 in the second trimester may improve the accuracy of predicting GH. However, our results were obtained by a nested case-control study using a relatively small sample size. Therefore, the significance of low Gal-1 levels in the second trimester for predicting PE/GH should be confirmed in a large multicenter cohort study in the future.
References
Nagaya K, Fetters MD, Ishikawa M, Kubo T, Koyanagi T, Saito Y, Sameshima H, Sugimoto M, Takagi K, Chiba Y, Honda H, Mukubo M, Kawamura M, Satoh S, Neki R . Causes of maternal mortality in Japan. J Am Med Assoc 2000; 283: 2661–2667.
Yamauchi A, Minakami H, Ohkuchi A, Usui R, Idei S, Sato I . Causes of stillbirth: an analysis of 77 cases. J Obstet Gynaecol Res 1999; 25: 419–424.
Valensise H, Bezzeccheri V, Rizzo G, Tranquilli AL, Garzetti GG, Romanini C . Doppler velocimetry of the uterine artery as a screening test for gestational hypertension. Ultrasound Obstet Gynecol 1993; 3: 18–22.
Ros HS, Cnattingius S, Lipworth L . Comparison of risk factors for preeclampsia and gestational hypertension in a population-based cohort study. Am J Epidemiol 1998; 147: 1062–1070.
Ohkuchi A, Hirashima C, Matsubara S, Takahashi K, Matsuda Y, Suzuki M . Threshold of soluble fms-like tyrosine kinase 1/placental growth factor ratio for the imminent onset of preeclampsia. Hypertension 2011; 58: 859–866.
Noori M, Donald AE, Angelakopoulou A, Hingorani AD, Williams DJ . Prospective study of placental angiogenic factors and maternal vascular function before and after preeclampsia and gestational hypertension. Circulation 2010; 122: 478–487.
Espinoza J, Kusanovic JP, Bahado-Singh R, Gervasi MT, Romero R, Lee W, Vaisbuch E, Mazaki-Tovi S, Mittal P, Gotsch F, Erez O, Gomez R, Yeo L, Hassan SS . Should bilateral uterine artery notching be used in the risk assessment for preeclampsia, small-for-gestational-age, and gestational hypertension? J Ultrasound Med 2010; 29: 1103–1115.
Shiozaki A, Matsuda Y, Satoh S, Saito S . Comparison of risk factors for gestational hypertension and preeclampsia in Japanese singleton pregnancies. J Obstet Gynaecol Res 2013; 39: 492–499.
Li X, Tan H, Huang X, Zhou S, Hu S, Wang X, Xu X, Liu Q, Wen SW . Similarities and differences between the risk factors for gestational hypertension and preeclampsia: a population based cohort study in South China. Pregnancy Hypertens 2016; 6: 66–71.
Ohkuchi A, Iwasaki R, Suzuki H, Hirashima C, Takahashi K, Usui R, Matsubara S, Minakami H, Suzuki M . Normal and high-normal blood pressures, but not body mass index, are risk factors for the subsequent occurrence of both preeclampsia and gestational hypertension: a retrospective cohort study. Hypertens Res 2006; 29: 161–167.
Poon LC, Kametas NA, Maiz N, Akolekar R, Nicolaides KH . First-trimester prediction of hypertensive disorders in pregnancy. Hypertension 2009; 53: 812–818.
Conde-Agudelo A, Belizán JM, Lede R, Bergel EF . What does an elevated mean arterial pressure in the second half of pregnancy predict–gestational hypertension or preeclampsia? Am J Obstet Gynecol 1993; 169: 509–514.
Poon LC, Akolekar R, Lachmann R, Beta J, Nicolaides KH . Hypertensive disorders in pregnancy: screening by biophysical and biochemical markers at 11–13 weeks. Ultrasound Obstet Gynecol 2010; 35: 662–670.
Skråstad RB, Hov GG, Blaas HG, Romundstad PR, Salvesen KA . A prospective study of screening for hypertensive disorders of pregnancy at 11–13 weeks in a Scandinavian population. Acta Obstet Gynecol Scand 2014; 93: 1238–1247.
Takahashi K, Ohkuchi A, Kobayashi M, Matsubara S, Suzuki M . Recurrence risk of hypertensive disease in pregnancy. Med J Obstet Gynecol 2014; 2: 1023.
Cnossen JS, Morris RK, ter Riet G, Mol BW, van der Post JA, Coomarasamy A, Zwinderman AH, Robson SC, Bindels PJ, Kleijnen J, Khan KS . Use of uterine artery Doppler ultrasonography to predict pre-eclampsia and intrauterine growth restriction: a systematic review and bivariable meta-analysis. CMAJ 2008; 178: 701–711.
Takahashi K, Ohkuchi A, Suzuki H, Usui R, Kuwata T, Shirasuna K, Matsubara S, Suzuki M . Biophysical interaction between blood pressure and uterine artery Doppler for the occurrence of early-onset preeclampsia: a prospective cohort study. Pregnancy Hypertens 2013; 3: 270–277.
Khalil A, Garcia-Mandujano R, Maiz N, Elkhaouli M, Nicolaides KH . Longitudinal changes in uterine artery Doppler and blood pressure and risk of pre-eclampsia. Ultrasound Obstet Gynecol 2014; 43: 541–547.
Kleinrouweler CE, Wiegerinck MM, Ris-Stalpers C, Bossuyt PM, van der Post JA, von Dadelszen P, Mol BW, Pajkrt E EBM CONNECT Collaboration.. Accuracy of circulating placental growth factor, vascular endothelial growth factor, soluble fms-like tyrosine kinase 1 and soluble endoglin in the prediction of pre-eclampsia: a systematic review and meta-analysis. BJOG 2012; 119: 778–787.
Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, Sibai BM, Epstein FH, Romero R, Thadhani R, Karumanchi SA, CPEP Study Group. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 2006; 355: 992–1005.
Antwi E, Groenwold RH, Browne JL, Franx A, Agyepong IA, Koram KA, Klipstein-Grobusch K, Grobbee DE . Development and validation of a prediction model for gestational hypertension in a Ghanaian cohort. BMJ Open 2017; 7: e012670.
Camby I, Le Mercier M, Lefranc F, Kiss R . Galectin-1: a small protein with major functions. Glycobiology 2006; 16: 137R–157R.
Barrientos G, Freitag N, Tirado-González I, Unverdorben L, Jeschke U, Thijssen VL, Blois SM . Involvement of galectin-1 in reproduction: past, present and future. Hum Reprod Update 2014; 20: 175–193.
Cooper DN . Galectinomics: finding themes in complexity. Biochim Biophys Acta 2002; 1572: 209–231.
Freitag N, Tirado-González I, Barrientos G, Herse F, Thijssen VL, Weedon-Fekjær SM, Schulz H, Wallukat G, Klapp BF, Nevers T, Sharma S, Staff AC, Dechend R, Blois SM . Interfering with Gal-1-mediated angiogenesis contributes to the pathogenesis of preeclampsia. Proc Natl Acad Sci USA 2013; 110: 11451–11456.
Menkhorst E, Koga K, Van Sinderen M, Dimitriadis E . Galectin-7 serum levels are altered prior to the onset of preeclampsia. Placenta 2014; 35: 281–285.
Wu P, van den Berg C, Alfirevic Z, O'Brien S, Röthlisberger M, Baker PN, Kenny LC, Kublickiene K, Duvekot JJ . Early pregnancy biomarkers in preeclampsia: a systematic review and meta-analysis. Int J Mol Sci 2015; 16: 23035–23056.
Schnabel A, Blois SM, Meint P, Freitag N, Ernst W, Barrientos G, Conrad ML, Rose M, Seelbach-Göbel B . Elevated systemic galectin-1 levels characterize HELLP syndrome. J Reprod Immunol 2016; 114: 38–43.
Hsieh SH, Ying NW, Wu MH, Chiang WF, Hsu CL, Wong TY, Jin YT, Hong TM, Chen YL . Galectin-1, a novel ligand of neuropilin-1, activates VEGFR-2 signaling and modulates the migration of vascular endothelial cells. Oncogene 2008; 27: 3746–3753.
Molvarec A, Blois SM, Stenczer B, Toldi G, Tirado-Gonzalez I, Ito M, Shima T, Yoneda S, Vásárhelyi B, Rigó J Jr, Saito S . Peripheral blood galectin-1-expressing T and natural killer cells in normal pregnancy and preeclampsia. Clin Immunol 2011; 139: 48–56.
Blois SM, Gueuvoghlanian-Silva BY, Tirado-González I, Torloni MR, Freitag N, Mattar R, Conrad ML, Unverdorben L, Barrientos G, Knabl J, Toldi G, Molvarec A, Rose M, Markert UR, Jeschke U, Daher S . Getting too sweet: galectin-1 dysregulation in gestational diabetes mellitus. Mol Hum Reprod 2014; 20: 644–649.
Takahashi K, Ohkuchi A, Hirashima C, Matsubara S, Suzuki M . Establishing reference values for mean notch depth index, pulsatility index and resistance index in the uterine artery at 16–23 weeks' gestation. J Obstet Gynaecol Res 2012; 38: 1275–1285.
Hirashima C, Ohkuchi A, Matsubara S, Suzuki H, Takahashi K, Usui R, Suzuki M . Alteration of serum soluble endoglin levels after the onset of preeclampsia is more pronounced in women with early-onset. Hypertens Res 2008; 31: 1541–1548.
Hirashima C, Ohkuchi A, Takahashi K, Suzuki H, Yoshida M, Ohmaru T, Eguchi K, Ariga H, Matsubara S, Suzuki M . Gestational hypertension as a subclinical preeclampsia in view of serum levels of angiogenesis-related factors. Hypertens Res 2011; 34: 212–217.
Sato K A proposal for a new definition and classification of ‘pregnancy induced hypertension (PIH)’ (2004). In Japan Society for the Study of Toxemia of Pregnancy (ed), Historical Perspective of Study of Pregnancy-Induced Hypertension in Japan. Medical View Co: Tokyo, Japan, 2005, pp. 54–87.
Watanabe K, Naruse K, Tanaka K, Metoki H, Suzuki Y . Outline of definition and classification of ‘Pregnancy induced Hypertension (PIH)’. Hypertens Res Pregnancy 2013; 1: 3–4.
Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai BM . The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens 2013; 3: 44–47.
Ogawa Y, Iwamura T, Kuriya N, Kuriya N, Nishida H, Takeuchi H, Yakada M, Itabashi K, Imura S, Isobe K . Birth size standards by gestational age for Japanese neonates. Acta Neonatol Jpn 1998; 34: 624–632.
Confidence interval calculatorhttp://www.pedro.org.au/english/downloads/confidence-interval-calculator/. Accessed 30 July 2016.
Jaeschke R, Guyatt G, Sackett DL . Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. J Am Med Assoc 1994; 271: 703–707.
Conde-Agudelo A, Villar J, Lindheimer M . World Health Organization systematic review of screening tests for preeclampsia. Obstet Gynecol 2004; 104: 1367–1391.
Kanda Y . Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 2013; 48: 452–458.
Jeschke U, Mayr D, Schiessl B, Mylonas I, Schulze S, Kuhn C, Friese K, Walzel H . Expression of galectin-1, -3 (gal-1, gal-3) and the Thomsen-Friedenreich (TF) antigen in normal, IUGR, preeclamptic and HELLP placentas. Placenta 2007; 28: 1165–1173.
Than NG, Erez O, Wildman DE, Tarca AL, Edwin SS, Abbas A, Hotra J, Kusanovic JP, Gotsch F, Hassan SS, Espinoza J, Papp Z, Romero R . Severe preeclampsia is characterized by increased placental expression of galectin-1. J Matern Fetal Neonatal Med 2008; 21: 429–442.
Blois SM, Ilarregui JM, Tometten M, Garcia M, Orsal AS, Cordo-Russo R, Toscano MA, Bianco GA, Kobelt P, Handjiski B, Tirado I, Markert UR, Klapp BF, Poirier F, Szekeres-Bartho J, Rabinovich GA, Arck PC . A pivotal role for galectin-1 in fetomaternal tolerance. Nat Med 2007; 13: 1450–1457.
Kopcow HD, Rosetti F, Leung Y, Allan DS, Kutok JL, Strominger JL . T cell apoptosis at the maternal-fetal interface in early human pregnancy, involvement of galectin-1. Proc Natl Acad Sci USA 2008; 105: 18472–18477.
Brosens IA, Robertson WB, Dixon HG . The role of the spiral arteries in the pathogenesis of preeclampsia. Obstet Gynecol Annu 1972; 1: 177–1791.
Gerretsen G, Huisjes HJ, Elema JD . Morphological changes of the spiral arteries in the placental bed in relation to pre-eclampsia and fetal growth retardation. Br J Obstet Gynaecol 1981; 88: 876–881.
Khong TY, De Wolf F, Robertson WB, Brosens I . Inadequate maternal vascular response to placentation in pregnancies complicated by pre-eclampsia and by small-for-gestational age infants. Br J Obstet Gynaecol 1986; 93: 1049–1059.
Meekins JW, Pijnenborg R, Hanssens M, McFadyen IR, van Asshe A . A study of placental bed spiral arteries and trophoblast invasion in normal and severe pre-eclamptic pregnancies. Br J Obstet Gynaecol 1994; 101: 669–674.
Hirashima C, Ohkuchi A, Takahashi K, Suzuki H, Matsubara S, Suzuki M . A novel three-step approach for predicting the imminent onset of preeclampsia within 4 weeks after blood sampling at 19–31 weeks of gestation. Hypertens Res 2014; 37: 519–525.
Tirado-González I, Freitag N, Barrientos G, Shaikly V, Nagaeva O, Strand M, Kjellberg L, Klapp BF, Mincheva-Nilsson L, Cohen M, Blois SM . Galectin-1 influences trophoblast immune evasion and emerges as a predictive factor for the outcome of pregnancy. Mol Hum Reprod 2013; 19: 43–53.
Hiby SE, Walker JJ, O'shaughnessy KM, Redman CW, Carrington M, Trowsdale J, Moffett A . Combinations of maternal KIR and fetal HLA-C genes influence the risk of preeclampsia and reproductive success. J Exp Med 2004; 200: 957–965.
Acknowledgements
This work was supported by Grants-in-Aid (18591809, 24390383, and 24592482 to AO, S1311029 to SM) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Rights and permissions
About this article
Cite this article
Hirashima, C., Ohkuchi, A., Nagayama, S. et al. Galectin-1 as a novel risk factor for both gestational hypertension and preeclampsia, specifially its expression at a low level in the second trimester and a high level after onset. Hypertens Res 41, 45–52 (2018). https://doi.org/10.1038/hr.2017.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.85
Keywords
This article is cited by
-
Galectin-1 expression in the serum and placenta of pregnant women with fetal growth restriction and its significance
BMC Pregnancy and Childbirth (2021)
-
Galectin-1–Related Modulation of Trophoblast Endothelial Interactions by Integrins α1 and β1
Reproductive Sciences (2020)