Abstract
The diameters of the retinal microvasculature reflect intermediate target organ damage and predict adverse health outcomes. In view of the pulsatility of the cerebral blood flow and refinement of software used for off-line analysis, we assessed the repeatability of retinal microvascular diameters in ECG-gated vs. non-gated images using nonmydriatic retinal photographs (Canon Cr-DGi visualization system) postprocessed by IVAN (Vasculomatic ala Nicola, version 1.1) or SIVA (Singapore I Vessel Assessment, version 3.6). Using these algorithms, we determined the central retinal arteriolar (CRAE) and venular (CRVE) equivalents and their ratio (arteriole-to-venule ratio (AVR)). The estimates of CRAE (mean, 158.5 μm), CRVE (222.5 μm) and AVR (0.71) in 10 volunteers were unaffected (P⩾0.059) by ECG gating. We assessed intragrader repeatability by the Bland and Altman approach in 30 participants with non-gated images and 30 with ECG-gated photographs. Repeatability, which was expressed as the percentage of near maximal variability (4-s.d. range), did not improve with ECG gating. Using SIVA, CRAE and CRVE were systematically larger (P⩽0.031), and the AVR estimates were similar (P⩾0.15) compared with IVAN. The differences (IVAN−SIVA) averaged −5.4 μm for CRAE, −3.9 μm for CRVE and −0.012 for AVR in the non-gated images and −3.3 μm, −6.9 μm and 0.006, respectively, in the ECG-gated photographs. In conclusion, ECG gating does not affect estimates of the retinal microvascular diameters or improve intragrader repeatability. SIVA yields slightly but significantly larger estimates of the retinal arteriolar and venular diameters. Combining historical readings analyzed by IVAN with more recent readings by SIVA is possible only for AVR and is not recommended for either CRAE or CRVE.
Similar content being viewed by others
Introduction
Non-mydriatic retinal photography allows clinicians to measure the retinal microvessels,1, 2 which are representative of the microcirculation in the brain. This completely non-invasive technique is easily applicable in population surveys.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 In cross-sectional studies,1, 2 hypertension is associated with retinal arteriolar narrowing, and in prospective studies, a lower arteriole-to-venule ratio (AVR) predicts the incidence of hypertension.5, 6 Moreover, the diameters of the retinal microvessels carry important prognostic information7, 8, 9 as a smaller arteriolar diameter,8, 9 wider venular caliber9 and lower AVR7 predict cardiovascular mortality,8 coronary heart disease7 and lacunar stroke.9
The brain11 and by extension the retina12 are perfused at high-volume flow with a pulsatility that is maintained up to the effluent venous blood flow. In 1994, Chen et al.12 reported that retinal arteriolar diameter peaked in mid-systole and venular diameter peaked in early diastole, with maximal increases in the diameters of 3.5% and 4.8%, respectively. Subsequent studies applying non-mydriatic photography13, 14 or confocal scanning laser ophthalmoscopy15 confirmed the changes in the diameter of the retinal microvessels during the cardiac cycle. These studies had a sample size ranging from 1012, 15 to 1513, included only healthy volunteers12, 13, 14, 15 and did not report on the repeatability of the microvascular diameters measured in relation to ECG gating or the software package used for off-line analysis.12, 13, 14, 15 The prospectively defined hypotheses underlying our study were that the changes in the diameters of the retinal microvessels observed during the cardiac cycle and the refinement achieved over the past decade in the software used for the computer-aided postprocessing of retinal photographs would enhance intraobserver and interobserver repeatability. We addressed these research objectives in ECG-gated vs. non-gated retinal images from people enrolled in the Flemish Study on Environment, Genes and Health Outcomes (FLEMENGHO)16 and healthy volunteers who were analyzed using the two software packages.
Methods
Study population
FLEMENGHO was conducted according to the principles outlined in the Declaration of Helsinki for Investigations of Human Participants. The Ethics Committee of the University of Leuven approved the study. Recruitment started in 1985 and participants underwent repeated follow-up.16 The initial participation rate was 78.0%. Follow-up included retinal imaging without ECG gating in 1243 participants examined from January 2008 until June 2014 and retinal imaging with ECG gating in 168 participants examined from August 2014 until March 2015. We randomly selected subsets of apparently healthy participants, 30 with non-gated images and 30 with ECG-gated photographs. In addition, in accord with the sample size of previous studies,12, 15, 17 we recruited 10 healthy volunteers to compare non-gated and ECG-gated images in the same subjects. All participants provided informed written consent at the time of retinal phenotyping.
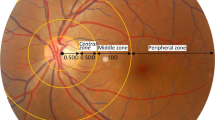
Retinal photography
Participants were asked to refrain from heavy exercise, smoking and drinking alcohol or caffeine-containing beverages for at least 3 h before retinal imaging. Patients on blood pressure-lowering drugs continued their medication on the examination days. We applied a non-mydriatic approach in a dimly lit room to obtain retinal photographs, one image per eye in each participant, with the Canon Cr-DGi retinal visualization system combined with the Canon D-50 digital camera (Canon, Medical Equipment Group, Utsunomiya, Japan). We determined the central retinal arteriolar (CRAE) and venular (CRVE) equivalents, which represent the retinal arteriolar and venular diameters, respectively. We used the validated computer-assisted program IVAN (Vasculomatic ala Nicola, version 1.1, Department of Ophthalmology and Visual Science, University of Wisconsin-Madison, Madison, WI, USA)18 or SIVA (Singapore I Vessel Assessment, version 3.6, Singapore Eye Research Institute, Singapore, Singapore) based on formulae published by Parr19, 20 and Hubbard.21 The software returns average vessel diameters according to the revised Knudtson formula.22 AVR was calculated by dividing the CRAE by the CRVE. We used a three-lead ECG monitoring device, along with a purpose-built microcontroller to sample the ECG signal outputted by a CardiMax FX-8322 recorder (Fukuda Denshi, Tokyo, Japan) to obtain the R wave in real time at a sampling rate of 8000 Hz and to generate a trigger pulse for acquiring the retinal image delayed by 300 ms relative to the top of the R wave.
Graders who were blinded to the identity of the study participants scored the 30 non-gated and 30 gated images to compare the performance of the two software packages in terms of intraobserver and interobserver variability. The 30 gated and 30 non-gated images were obtained from different participants; thus a test–retest design was not applicable to this part of the study. We randomized 10 healthy volunteers in a 1:1 ratio to undergo retinal imaging first with gating and then without gating or vice versa to test the difference between non-gated and ECG-gated images. The interval between the test and retest was 60 min. One reader (F-FW) who was blinded to the identity of the volunteer and the order in which the retinal pictures were taken scored all images.
Other measurements
Blood pressure was measured five times consecutively after the participants had rested for 5 min in a sitting position using a standard mercury sphygmomanometer (Riester, Jungingen, Germany). For analysis, the five readings were averaged. Mean arterial pressure was the diastolic blood pressure plus one-third of the difference between the systolic and diastolic blood pressure. Hypertension was defined as a blood pressure of at least 140 mm Hg systolic or 90 mm Hg diastolic or the use of antihypertensive drugs. Body mass index was defined as weight in kilograms divided by height in meters squared. Nurses administered a validated questionnaire to obtain information on each participant’s medical history, smoking and drinking habits and intake of medications. After the participants fasted for at least 6 h, venous blood samples were drawn to measure the plasma glucose and serum cholesterol levels. Diabetes was defined as a fasting plasma glucose of at least 7.0 mmol l−1 or the use of antidiabetic drugs.23
Statistical analysis
We used the SAS software, version 9.3 (SAS Institute, Cary, NC, USA) for database management and statistical analysis. For comparison of means and proportions, we applied Student’s t-test for paired or unpaired observations, as appropriate, and the χ2-statistic, respectively. We assessed the agreement between paired measurements using the method described by Bland and Altman.24 Repeatability was defined as two times the s.d. of the pairwise differences between duplicate measurements and was expressed as a percentage of the average of all first and repeat measurements. To enable comparisons with the literature, we also computed the intraclass correlation coefficient between duplicate measurements and the interclass correlation coefficient between the two observers who coded the non-gated images. Statistical significance was an α-level of <0.05 in two-sided tests.
Results
Characteristics of the participants
Table 1 lists the characteristics of the FLEMENGHO participants, 30 with non-gated images and 30 with ECG-gated retinal photographs, and of the 10 healthy volunteers who underwent both non-gated and ECG-gated imaging. In these three groups, the age ranged from 21.0 to 79.8 years, from 18.9 to 86.1 years and from 24.1 to 54.5 years, respectively. Participants who underwent ECG-gated imaging tended to have higher systolic (131.4 vs. 123.4 mm Hg; P=0.080) and diastolic (83.0 vs. 79.0 mm Hg; P=0.15) blood pressures with no difference in the prevalence of hypertension (30.0% vs. 23.3%; P=0.56) compared with those with non-gated imaging. Otherwise, there were no differences between these two groups in any of the continuous and categorical variables listed in Table 1 (P⩾0.31).
Repeatability of the measurements derived from the non-gated photographs
In the 30 participants with non-gated photographs (Table 2), the differences (repeat−first) between two photographs read by the same observer (F-FW) were 0.75 μm (P=0.18) for CRAE, 0.39 μm for CRVE (P=0.40) and 0.002 units (P=0.52) for AVR, as measured by IVAN, and −0.26 μm (P=0.56), −0.48 μm (P=0.36) and 0.001 units (P=0.70), respectively, as measured by SIVA. Expressed as a percentage of the near maximal variability (the 4-s.d. interval), the repeatability for each of these measurements was 11.0, 6.4 and 9.3% for IVAN and 9.1, 6.5 and 8.3% for SIVA, respectively, with higher values indicating worse repeatability. The intraobserver correlation coefficients were 0.98, 0.99 and 0.98 and 0.98, 0.99 and 0.98, respectively.
With regard to interobserver repeatability, the mean differences between two observers (F-FW−Z-YZ) were −1.4±5.3 μm (95% confidence interval (CI), −3.4 to 0.53 μm; P=0.14), −0.79±2.9 μm (CI, −1.9 to 0.30 μm; P=0.15) and −0.004±0.029 units (CI, −0.015 to 0.007 units; P=0.49) for CRAE, CRVE and AVR, respectively, as estimated by IVAN. The corresponding differences for the SIVA measurements were −0.50±4.6 μm (CI, −2.2 to 1.2 μm; P=0.56), −0.22±7.9 μm (CI, −3.2 to 2.7 μm; P=0.88), and −0.002±0.03 units (CI, −0.014 to 0.010 units; P=0.73). Expressed as a percentage of the near maximal variability, the repeatability was 19.8, 7.6 and 21.4% for CRAE, CRVE and AVR, respectively, using IVAN and 18.4, 19.4 and 25.0%, respectively, using SIVA. The corresponding interobserver correlation coefficients were 0.92, 0.99 and 0.91 and 0.94, 0.93 and 0.87, respectively.
Repeatability of the measurements derived from the ECG-gated photographs
In the 30 participants with ECG-gated images (Table 2), the differences between the two photographs read by the same observer (F-FW) were 0.35 μm (P=0.65) for CRAE, 0.40 μm for CRVE (P=0.44) and 0.001 units (P=0.83) for AVR as measured by IVAN and −0.64 μm (P=0.34), −0.95 μm (P=0.21) and −0.0001 (P=0.96), respectively, as measured by SIVA. Expressed as a percentage of the near maximal variability, repeatability amounted to 14.1% for CRAE, 7.3% for CRVE and 17.6% for AVR as read by IVAN and to 11.5% for CRAE, 11.4% for CRVE and 16.2% for AVR as processed by SIVA. The corresponding intragrader correlation coefficients were 0.96, 0.99 and 0.92 and 0.97, 0.97 and 0.95, respectively.
Differences between the non-gated and ECG-gated measurements
Among the 10 volunteers who underwent both non-gated and ECG-gated retinal imaging (Table 3), the two approaches yielded similar point estimates of the mean CRAE, CRVE and AVR, with differences (non-gated−ECG-gated) averaging 0.92 μm for CRAE (P=0.36), 2.7 μm for CRVE (P=0.059) and −0.004 units for AVR (P=0.63) using IVAN and −0.29 μm (P=0.71), 1.2 μm (P=0.21) and −0.004 units (P=0.42), respectively, using SIVA. Expressed as a percentage of the near maximal variability, repeatability amounted to 11.8% for CRAE, 9.8% for CRVE and 12.5% for AVR using IVAN and to 13, 11.7 and 20%, respectively, using SIVA (Table 3).
Furthermore, with adjustments applied to sex, age, systolic blood pressure, smoking and antihypertensive drug treatment, we compared CRAE between the two groups of FLEMENGHO participants who underwent retinal imaging without and with ECG gating. In these non-paired comparisons, the differences in CRAE (non-gated−ECG-gated) averaged 4.9 μm (P=0.11) using IVAN and 2.3 μm (P=0.50) using SIVA.
Differences between the off-line readings using IVAN and SIVA
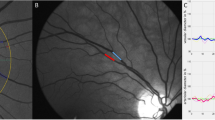
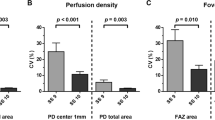
Although there was interindividual variability (Figure 1), the estimates of CRAE and CRVE were systematically larger with SIVA compared with IVAN (Table 4), with no differences in AVR, regardless of whether ECG gating was applied. The differences (IVAN−SIVA) averaged −5.4 μm (P<0.001) for CRAE, −3.9 μm (P=0.031) for CRVE and −0.012 units (P=0.15) for AVR in the non-gated images and −3.3 μm (P<0.001), −6.9 μm (P<0.001) and 0.006 units (P=0.20), respectively, in ECG-gated photographs.
Differences between the 60 individual participants in the estimates of retinal microvascular diameters in images that were postprocessed by the same observer (F-FW) using IVAN and SIVA. The differences (Δ) and corresponding significance (P) are provided for the central retinal arteriolar equivalent (CRAE) in panel (a), for the central retinal venular equivalent (CRVE) in panel (b) and for the arteriole-to-venule ratio (AVR) in panel (c). The percentage of values refer to the proportion of participants with smaller CRAE (a), CRVE (b) or AVR (c) using SIVA compared with IVAN.
Discussion
The retinal microcirculation is a pivotal trait in clinical and population research, because narrowing of the retinal microvessels reflects target organ damage and predicts adverse health outcomes. Our current study addresses two questions, which to the best of our knowledge, have both previously been addressed. First, in view of the pulsatility of the retinal blood flow, does ECG gating improve the precision of retinal microvascular diameter measurements? Second, are estimates of retinal microvascular diameters consistent if retinal photographs are postprocessed with newer (SIVA) software compared with older (IVAN) software? Regarding the first question, our key finding was that ECG gating had no influence on estimates of the retinal microvascular diameters and did not improve intraobserver repeatability, irrespective of the software used. For the second question, we showed that in the presence of large intraindividual variability, on average, SIVA produced significantly larger estimates of the retinal microvascular diameters compared with IVAN. Among the 16.7% of subjects with smaller CRAE or smaller CRVE using SIVA compared with IVAN, only two had both smaller CRAE and CRVE. The smaller diameters obtained with IVAN compared with SIVA are clinically relevant. Indeed, as estimated in the same study population1 and in accord with most published papers, as reviewed in Liu et al.,1 CRAE decreases by ~3 μm and CRVE by ~4 μm per 10-year increment in age. CRAE narrows by ~4 μm for a 10-mm Hg increase in mean arterial pressure. These estimates must be compared with the 3–5 μm lower CRAE and the 4–7 μm lower CRVE, when IVAN was used for postprocessing instead of SIVA (Table 4).
Several previous studies12, 13, 14, 15 reported the pulsatility of the retinal blood flow during the cardiac cycle and suggested that strategies that account for pulsatility might be relevant in the assessment of retinal microvascular diameters. Chen et al.12 reported maximum increases of 3.46% in the arteriolar diameter and 4.82% in the venular diameter in mid-late systole and early diastole, respectively. Kumar et al.14 observed increases in diameter averaging 3.3 μm for arterioles and 6.6 μm for venules when accounting for pulsatile motion. Without visualization of the pulsatile motion, these diameter changes were 2.1 and 4.7 μm, respectively.14 Hao et al.13 reported increases in the arteriolar and venular diameters of up to of 3.9 μm (6.3%; P<0.001) and 3.0 μm (3.4%; P<0.001), respectively. What all previous studies had in common is that 812−14 to 45 (9 per second)15 retinal images were taken at fixed intervals triggered by the ECG signal, spanning one or more cardiac cycles. The measurements were performed on a single microvascular segment that was carefully selected based on image quality. Hao et al.13 also used SIVA to obtain ‘summary’ measurements of the vessel caliber in the left eye. Using this approach, which we applied in our current study, the diameter increases during the cardiac cycle by up to 3.8 μm (2.5%) for arterioles and up to 8.7 μm (4.1%) for venules, but the difference was not statistically significant (P⩾0.12).
In the present study, we sampled the ECG signal in real time at 8000 Hz and acquired a single retinal photograph of the left and right eye with a 300-ms delay relative to the top of the R wave. This delay ensured that the trigger for the retinal photographs coincided with left ventricular ejection during the ST-segment of the ECG for heart rates ranging from 60 to 100 beats per minute. Thus, in view of the report by Hao et al.,13 the use of summary measurements probably explains why ECG gating did not affect the estimates of the retinal microvascular diameters in the present study. Indeed, the propagation of the pulse wave from the six largest arterioles to the six largest venules takes time. Therefore, the average changes in the diameters across ‘the big six estimated’ from a single photograph of both eyes with a shutter time of 1/60 s might obscure the diameter changes picked up by photography and off-line analysis of selected segments, as reported in studies describing the pulsatility of the retinal microvasculature.12, 13, 14, 15 Furthermore, Knudston et al.25 reported that the variations across photographs taken in a single individual within the same point in the cardiac cycle were too large to detect differences across the three points in the cardiac cycle. Other potential confounders obscuring the caliber changes graded by IVAN or SIVA are the pulsatile motion of the microvessels and auto-regulation of the retinal microvasculature.
A key finding was that the use of SIVA instead of IVAN for post-processing produced slightly but significantly larger estimates of CRAE and CRVE, with no difference in AVR. The implications of these observations are that it is only possible to combine historical AVR readings analyzed by IVAN with more recent readings analyzed by SIVA, but this process cannot be recommended for CRAE or CRVE. AVR is a relative measure that combines information from the arteriolar and venular side of the retinal microcirculation, is normally distributed and decreases with increasing risk, as exemplified by hypertension.21 It has the advantage of controlling for magnification differences resulting from camera lenses or refractive error.26 Our study adds the use of different software packages as an additional factor that can control for the use of AVR. From this perspective, one should note that AVR was the key prognostic variable in influential studies relating adverse health outcomes to the retinal microcirculation. Among the 10 358 participants in the Atherosclerosis Risk in Communities study,27 with adjustments applied for multiple risk factors, including mean arterial pressure, plasma glucose and total and high-density lipoprotein cholesterol, the lower AVR (mean, 0.84) over 3.5 years of follow-up was associated with a higher stroke risk (110 incident cases; P=0.03). In a case–control study (cases/controls, 413/1198) nested within the Beaver Dam Eye Study,8 the odds ratio of any cardiovascular death over the 10 years of follow-up in relation to generalized arteriolar narrowing, which was defined as the lowest quintile of the AVR distribution, was 1.5 (95% CI, 1.1–2.1). In the Rotterdam Study,3 AVR was inversely associated with carotid intima-media thickness and plaque score. On the other hand, in 386 patients with essential hypertension, Masaidi et al.28 failed to reveal formally significant multivariable-adjusted correlations of carotid intima-media thickness and left ventricular mass index (P=0.06 for both) with AVR. According to the authors’ interpretation, the lack of significance in the study might have resulted from the small sample size and the inclusion of patients with a narrow spread of demographic and clinical characteristics, most of whom were undergoing antihypertensive treatment.28
In our present study, the intraobserver variability in both the ECG-gated and non-gated images was within acceptable limits. The variability calculated using Bland and Altman’s method ranged from 2.3% to 17.6%. Other groups reported the repeatability of retinal phenotypes as a correlation coefficient29, 30 or as a coefficient of variation.17 However, the use of a correlation coefficient to compare repeated measurements is less accurate, as it measures the strength of a relation but not the agreement between two variables.24 Furthermore, coefficients of variation represent a normalized measure of the dispersion of a probability distribution. When the mean value is close to zero, the coefficient of variation will approach infinity and is therefore sensitive to small changes in the mean.
Compared with IVAN, SIVA generates information over and beyond the diameter of the retinal microvasculature, including fractal dimensions, branching pattern and tortuosity. Retinal vascular branching and tortuosity might be early indicators of microvascular damage. Indeed, in a population-based cross-sectional study, Cheung et al.31, 32 showed that the retinal arteriolar branching asymmetry ratio and arteriolar and venular tortuosity were independently correlated with the mean arterial blood pressure in multivariable linear regression analysis. In another cross-sectional study of 1159 participants with type-1 diabetes, Sasongko et al.33 observed that retinopathy (odds ratio, 2.01; CI, 1.23–3.29), early kidney dysfunction (1.56; CI, 1.06–2.28) and the coexistence of both complications (1.96; CI, 1.21–3.24) were associated with higher arteriolar tortuosity.
Our current study must be interpreted within the context of some potential limitations. First, we specifically recruited healthy normotensive volunteers to compare ECG-gated and non-gated images. To our knowledge, all previous reports on the changes in the diameter of the retinal microvasculature during the cardiac cycle also included normotensive volunteers.12, 13, 14, 15 One might hypothesize that the changes in the retinal arteriolar diameter observed during the cardiac cycle might be proportional to the extending pressure and therefore would be larger in hypertensive patients than in normotensive people. Our current findings showed similarities in the retinal arteriolar diameters in the gated and non-gated images and therefore cannot be generalized to patients with elevated systolic blood pressure. Second, the characteristics listed in Table 1 were similar among the selected and non-selected participants from the 2008–2014 cohort, with the exception of systolic blood pressure (123.4 mm Hg vs. 130.4 mm Hg; P=0.025) and the prevalence of hypertension (23.3% vs. 45.1%; P=0.018). These variables were not different among the selected and non-selected participants from the 2014–2015 cohort. The mismatch in the 2008–2014 cohort occurred by chance, as the participants were randomly selected, but it might limit the generalizability of our findings related to the non-gated retinal images. However, our findings for intraobserver variability (Table 2) and for the differences between software packages were consistent, regardless of whether the participants were recruited among the 2008–2014 cohort (non-gated images) or the 2014–2015 cohort (ECG-gated images). Third, we only assessed interobserver repeatability in 30 participants from the population study who underwent non-gated imaging that was postprocessed by both IVAN and SIVA. Because there were no differences in the retinal microvascular measurements associated with ECG gating, we did not repeat the assessment of interobserver repeatability in the 30 participants who underwent ECG-gated photography.
In population-based research, retinal microvasculature is an established key trait because of its association with hypertension1, 2, 5, 6 and its role as a predictor of adverse cardiovascular outcomes.7, 8, 9 Our study adds to the current knowledge base by showing that ECG gating does not affect estimates of the retinal microvascular diameters or improve intraobserver repeatability and that SIVA yields larger and clinically relevant estimates of CRAE and CRVE with no differences in AVR compared with IVAN. The implications for research are twofold. First, despite the pulsatility of retinal blood flow,12, 13, 14, 15 ECG gating does not enhance the accuracy of summary measurements of the retinal microvascular diameters by IVAN and SIVA. Second, it is possible to combine historical AVR readings analyzed by IVAN with more recent readings postprocessed by SIVA, but it is not possible for CRAE or CRVE. One possible way to pool CRAE and CRVE estimates obtained with IVAN and SIVA is to use standardized units by expressing each individual reading in units of s.d. after stratification for use in IVAN or SIVA. However, the validity of this approach still requires further investigation before it can be proposed as an alternative to re-measuring all historical images using the newer software.
References
Liu YP, Richart T, Jin Y, Struijker-Boudier HA, Staessen JA . Retinal arteriolar and venular phenotypes in a Flemish population: reproducibility and correlates. Artery Res 2011; 5: 72–79.
Cheung CY, Ikram MK, Sabanayagam C, Wong TY . Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension 2012; 60: 1094–1103.
Ikram MK, de Jong FJ, Vingerling JR, Witteman JC, Hofman A, Breteler MM, de Jong PT . Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Invest Ophthalmol Vis Sci 2004; 45: 2129–2134.
Myers CE, Klein R, Knudtson MD, Lee KE, Gangnon R, Wong TY, KLein BE . Determinants of retinal venular diameter: The Beaver Dam Eye Study. Ophthalmology 2012; 119: 2563–2571.
Wong TY, Shankar A, Klein R, Klein BEK, Hubbard LD . Prospective cohort study of retinal vessel diameters and risk of hypertension. Brit Med J 2004; 329: 79.
Wong TY, Klein R, Sharrett AR, Duncan BB, Couper DJ, Klein BEK, Hubbard LD, Nieto FJ,, for the Atherosclerosis Risk in Communities study. Retinal arteriolar diameter and risk for hypertension. Ann Intern Med 2004; 140: 248–255.
Wong TY, Klein R, Sharrett AR, Duncan BB, Couper DJ, Tielsch JM, Klein BEK, Hubbard LD . Retinal arteriolar narrowing and risk of coronary heart disease in men and women. The Atherosclerosis Risk in Communities study. JAMA 2002; 287: 1153–1159.
Wong TY, Klein R, Nieto FJ, Klein BEK, Sharrett AR, Meuer SM, Hubbard LD, Tielsch JM . Retinal microvascular abnormalities and 10-year cardiovascular mortality. A population-based case-control study. Ophthalmology 2003; 110: 933–940.
Yatsuya H, Folsom AR, Wong TY, Klein R, KLein BE, Sharrett AR,, ARIC Study Investigators. Retinal microvascular abnormalities and risk of lacunar stroke: Atherosclerosis Risk in Communities Study. Stroke 2010; 41: 1349–1355.
Lin F, Zhu P, Huang F, Li Q, Yuan Y, Gao Z, Yu P, Lin J, Chen F . Aortic stiffness is associated with central retinal arteriolar equivalent and retinal vascular fractal diminsion in a population along the southeastern coast of China. Hypertens Res 2015; 38: 342–348.
O’Rourke MF, Safar ME . Relationship between aortic stiffening and microvascular disease in brain and kidney. Cause and logic of therapy. Hypertension 2005; 46: 200–204.
Chen HC, Patel V, Wiek J, Rassam SM, Kohner EM . Vessel diameter changes during the cardiac cycle. Eye 1994; 8: 97–103.
Hao H, Sasongko MB, Wong TY, Che Azemin MC, Aliahmad B, Hodgson L, Kawasaki R, Cheung CY, Wang JJ, Kumar DK . Does retinal vascular geometry vary with cardiac cycle? Invest Ophthalmol Vis Sci 2012; 53: 5799–5805.
Kumar DK, Aliahmad B, Hao H, Che Azemin MC, Kawasaki R . A method for visualization of fine retinal vascular pulsation using nonmydriatic fundus camera synchronized with electrocardiogram. ISRN Ophthalmol 2013; 2013: 865834.
Moret F, Poloschek CM, Lagrèze WA, Bach M . Visualisation of fundus vessel pulsation using principal component analysis. Invest Ophthalmol Vis Sci 2011; 52: 5457–5464.
Liu YP, Gu YM, Thijs L, Knapen MHJ, Salvi E, Citterio L, Petit T, Delli Carpini S, Zhang Z, Jacobs L, Jin Y, Barlassina C, Manunta P, Kuznetsova T, Verhamme P, Struijker-Boudier HA, Cusi D, Vermeer C, Staessen JA . Inactive matrix gla protein is causally related to adverse health outcomes: a Mendelian randomization study in a Flemish population. Hypertension 2015; 65: 463–470.
Dumskyj MJ, Aldington SJ, Dore CJ, Kohner EM . The accurate assessment of changes in retinal vessel diameter using multiple frame electrocardiograph synchronised fundus photography. Curr Eye Res 1996; 15: 625–632.
Sherry LM, Wang JJ, Rochtchina E, Wong T, Klein R, Hubbard L, Mitchell P . Reliability of computer-assisted retinal vessel measurement in a population. Clin Exp Ophtalmol 2002; 30: 179–182.
Parr JC, Spears GF . Mathematic relationships between the width of a retinal artery and the widths of its branches. Am J Ophtalmol 1974; 77: 478–483.
Parr JC, Spears GF . General caliber of the retinal arteries expressed as the equivalent width of the central retinal artery. Am J Ophtalmol 1974; 77: 472–477.
Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS, Sharrett AR, Davis MD, Cai J . Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophtalmology 1999; 106: 2269–2280.
Knudtson MD, Lee KE, Hubbard LD, Wong TY, Klein R, Klein BE . Revised formulas for summarizing retinal vessel diameters. Curr Eye Res 2003; 27: 143–149.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003; 26: S5–S20.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Knudtson MD, Klein BEK, Klein R, Wong TY, Hubbard LD, Lee KE, Meuer SM, Bulla CP . Variation associated with measurement of retinal vessel diameters at different points in the pulse cycle. Br J Ophthalmol 2004; 88: 57–61.
Wong TY, Wang JJ, Rochtchina E, Klein R, Mitchell P . Does refractive error influence the association of blood pressure and retinal vessel diameters? The Blue Mountains Eye Study. Am J Ophthalmol 2004; 137: 1050–1055.
Wong TY, Klein R, Couper DJ, Cooper LS, Shahar E, Hubbard LD, Wofford MR . Retinal microvascular abnormalities and incident stroke: the Atherosclerosis Risk in Communities Study. Lancet 2001; 358: 1134–1140.
Masaidi M, Cuspidi C, Giudici V, Negri F, Sala C, Zanchetti A, Grassi G, Mancia G . Is retinal arteriolar-venular ratio associated with cardiac and extracardiac organ damage in essential hypertension? J Hypertens 2009; 27: 1277–1283.
Wong TY, Klein R, Klein BEK, Meuer SM, Hubbard LD . Retinal vessel diameters and their associations with age and blood pressure. Invest Ophthalmol Vis Sci 2003; 44: 4644–4650.
Couper DJ, Klein R, Hubbard LD, Wong TY, Sorlie PD, Cooper LS, Brothers RJ, Nieto FJ . Reliability of retinal photography in the assessment of retinal microvascular characteristics: the Atherosclerosis Risk in Communities Study. Am J Ophthalmol 2002; 133: 78–88.
Cheung CY, Tay WT, Mitchell P, Wang JJ, Hsu W, Lee ML, Lau QP, Zhu AL, Klein R, Saw SM, Wong TY . Quantitative and qualitative retinal microvascular characteristics and blood pressure. J Hypertens 2011; 29: 1380–1391.
Cheung CY, Zheng Y, Hsu W, Lee ML, Lau QP, Mitchell P, Wang JJ, Klein R, Wong TY . Retinal vascular tortuosity, blood pressure, and cardiovascular risk factors. Ophthalmology 2011; 118: 812–818.
Sasongko MB, Wong TY, Donaghue KC, Cheung N, Jenkins AJ, Benitez-Aguirre PZ, Wang JJ . Retinal arteriolar tortuosity is associated with retinopathy and early kidney dysfunction in type 1 diabetes. Am J Ophthalmol 2012; 153: 176–183.
Acknowledgements
The European Union (HEALTH-2011.2.4.2-2-EU-MASCARA, HEALTH-F7-305507 HOMAGE and the European Research Council Advanced Researcher Grant-2011-294713-EPLORE) and the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0881.13 and G.088013) currently support the Studies Coordinating Centre in Leuven. We acknowledge the contribution of the nurses working at the examination centre (Linda Custers, Marie-Jeanne Jehoul, Daisy Thijs and Hanne Truyens) and the clerical staff at the Studies Coordinating Centre (Annick De Soete and Renilde Wolfs).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wei, FF., Zhang, ZY., Petit, T. et al. Retinal microvascular diameter, a hypertension-related trait, in ECG-gated vs. non-gated images analyzed by IVAN and SIVA. Hypertens Res 39, 886–892 (2016). https://doi.org/10.1038/hr.2016.81
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.81
Keywords
This article is cited by
-
Perfused boundary region as biomarker for endothelial integrity in former preterms in adolescence
Pediatric Research (2023)
-
Diastolic left ventricular function in relation to the retinal microvascular fractal dimension in a Flemish population
Hypertension Research (2021)
-
Retinal venular tortuosity and fractal dimension predict incident retinopathy in adults with type 2 diabetes: the Edinburgh Type 2 Diabetes Study
Diabetologia (2021)
-
Early detection of microvascular dysfunction in hypertension: the holy grail of cardiovascular prevention and risk assessment?
Hypertension Research (2018)