Abstract
We conducted a retrospective cohort study of adult participants from the China Multicenter Collaborative Study of Cardiovascular Epidemiology to explore the relationship between early adulthood weight status, body weight change from age 25 to middle age and hypertension in the Chinese population. Self-reported weight was used to calculate the body mass index (BMI) at age 25. The association between BMI at age 25, subsequent weight change and hypertension was examined using a logistic regression model. Of the 14 635 study participants sampled in 1998, 3525 were diagnosed with hypertension. After adjusting for age, sex and other potential confounding factors, both the BMI at age 25 and weight gain were positively associated with the risk of hypertension (P for trend <0.001). Weight loss could more effectively reduce the risk of hypertension for participants with a higher BMI (BMI⩾24 kg m−2) at age 25 than for those who experienced a weight change of −2.5–2.5 kg. The odds ratio (OR) and 95% confidence interval (CI) for a weight change of −7.5 to −2.6 kg were 0.63 (0.46–0.86); for a weight change of <−7.5 kg, these statistics were 0.45 (0.32–0.63). For participants who had a lower BMI (18.5–20.9 kg m−2) at age 25, the OR and 95% CI were 0.86 (0.58–1.26) for a weight change of −7.5 to −2.6 kg and 0.95 (0.44–2.05) for a weight change of <−7.5 kg. Being overweight and obesity in early adulthood and adult weight gain were both independently associated with marked increase in the risk of hypertension in middle-aged men and women. Weight loss may be a protective factor against hypertension for people who were overweight or obese in early adulthood.
Similar content being viewed by others
Introduction
In recent decades, the prevalence of overweight and obesity has continued to rise across the globe.1 Hypertension is common in people who are overweight or obese,2, 3 and it is a major risk factor for cardiovascular diseases such as stroke and coronary heart disease.4, 5 Large population studies have shown that obesity is associated with hypertension6, 7, 8, 9 and is an important contributor to the great burden of hypertension in men and women.10, 11, 12 Additional findings based on Western or Japanese populations showed that overweight or obesity in early adulthood and weight gain are positively correlated with the risk of hypertension in middle age.13, 14 In the Chinese population, however, the long-term effects of body weight changes and body weight status in early adulthood on the risk of hypertension have not been well documented. This study evaluated cross-sectional survey data from the China Multicenter Collaborative Study of Cardiovascular Epidemiology to explore the relationship between body weight status in early adulthood and subsequent weight changes and hypertension in middle age.
Methods
Study populations
The participants were from the China Multicenter Collaborative Study of Cardiovascular Epidemiology, which was originally designed as a cross-sectional multicenter comparison of cardiovascular disease risk factors and later evolved into a comprehensive epidemiological study. The cross-sectional survey conducted in 1998 included 15 population samples, of which 9 were from rural residential areas and 6 from urban areas. These populations were selected on the basis of the main population characteristics, such as socioeconomic status and geographical location. Approximately one thousand participants with an age range of 35–59 years, of whom half were men and half women, were included as a random cluster sample (all eligible participants in randomly selected rural or urban areas, the latter including city blocks and factories) from each of the populations and were surveyed for risk factors of cardiovascular disease. Further details about the study populations have been reported elsewhere.15, 16 All participants signed consent forms.
Data collection
The demographic information, lifestyle risk factors and personal medical history were collected through a standardized questionnaire that also asked participants to recall their body weight at age 25. The schematic flow of this study is displayed in Figure 1. All staff involved in administering the survey were trained and certified in advance of the survey according to a uniform protocol and operation manual. In addition to the survey items, body weight, height and blood pressure (BP) were measured. Height was measured to the nearest centimeter using a vertical ruler, and weight was measured to the nearest kilogram with a spring balance. When they were weighed, all participants were required to wear light clothing and no shoes. BP measurements were performed while participants were seated in a quiet room with their legs uncrossed and elbow and forearm resting comfortably on the armrest of the BP measurement chair (or table), with their palms turned upward. The area to which the cuff was applied was free of clothing. Subjects did not eat, smoke, drink alcohol or perform strenuous exercise for half an hour before the BP measurement. BP was measured three times on the right arm. Systolic blood pressure (SBP) was based on the first Korotkoff phase, and diastolic blood pressure (DBP) was based on the fifth Korotkoff phase. The mean of the three measurements was used for the analysis. The body mass index (BMI) at age 25 was calculated as the remembered weight at age 25 (in kilograms) divided by the square of the height (in meters). Hypertension was defined as SBP⩾140 mm Hg and/or DBP⩾90 mm Hg or reported treatment with antihypertensive medications in the past 2 weeks.
Statistical analysis
All data were entered twice into the computers by trained staff at local centers and were then sent to the coordinating center of the Department of Epidemiology, Fuwai Hospital for final processing and analysis. During the analysis, the BMI at age 25 was categorized as underweight (<18.5 kg m−2), normal weight (18.5–23.9 kg m−2), overweight (24–27.9 kg m−2) and obesity (⩾28 kg m−2) based on the Working Group on Obesity in China guidelines.17 To maintain the generalizability of the current analysis, we also categorized the BMI based on the World Health Organization cutoff criteria.18 Weight change was calculated as the difference between the measured weight in 1998 and the recalled weight at age 25 and was grouped into six categories (<−7.5 kg; −7.5 to −2.6 kg; −2.5–2.5 kg; 2.6–7.5 kg; 7.6–12.5 kg and >12.5 kg); the −2.5–2.5 kg group was defined as stable weight. We calculated the mean values and proportions with a one-way analysis of variance for continuous variables and with χ2-tests for categorical variables. In addition, multivariate non-conditional logistic regression models were used to assess the associations between BMI and weight change categories and the risk of hypertension in middle-aged adults. To test for trends, we calculated the median values of BMI at 25 years of age and weight change within each category and then modeled these median values as a continuous variable in all models. Potential covariates, such as age, sex, urbanization, education level, cigarette use, alcohol consumption and family history of hypertension, were included in the multivariate models. In a separate analysis, we mutually adjusted for BMI at age 25 and adult weight change as a continuous variable to examine their independent contributions. A two-tailed P-value <0.05 was considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
A total of 15 573 participants were included in this study, representing a response rate of 85.1%. Nine hundred and thirty-eight participants were excluded, including 935 who could not provide the recalled body weight data at age 25 and 3 whose body weight had not been measured in 1998. In the present analysis, 14 635 participants remained, including 7016 men and 7619 women. Participants had a mean age of 46.7 years, a mean BMI at age 25 of 21.6 kg m−2 and a mean subsequent weight change of +5.7 kg. The baseline characteristics of the study population (in 1998) according to BMI at age 25 are shown in Table 1, in which they are categorized according to the Chinese cutoff. The SBP and DBP levels in middle-aged participants were positively associated with BMI at age 25. The mean SBP values ranged from 119.3 mm Hg for the underweight group to 133.6 mm Hg for the obese group, and the mean DBP values ranged from 76.3 mmHg to 82.5 mm Hg. In addition, significant differences were found between the BMI at age 25 groups in terms of age, sex, urbanization, education level, cigarette use, alcohol consumption and family history of hypertension (all P-values <0.001). We also displayed the baseline characteristics of the study population according to the World Health Organization BMI categories in Table 2; the characteristics of each BMI group were similar to those of the groups categorized according to the Chinese BMI cutoff values.
Table 3 shows the baseline characteristics of the study population (in 1998) according to the weight change categories. Participants who had greater weight gain were more likely to be urban residents, have higher education levels and have a family history of hypertension, but they were less likely to be smokers than those who had moderate weight gain or weight loss. More importantly, both SBP and DBP significantly increased with weight gain from age 25 years to middle age (P for trend <0.001).
Table 4 shows the prevalence and odds ratios (ORs) of hypertension according to BMI at age 25. The prevalence of hypertension for the four BMI categories was 18.0%, 23.4%, 30.3% and 46.0%. In an age- and sex-adjusted analysis (Model 1), BMI at age 25 was significantly associated with the risk of hypertension in middle age. The ORs (95% confidence interval (CI)) for the underweight group, the overweight group and the obesity group relative to the normal weight group were 0.80 (0.69–0.93), 1.38 (1.24–1.54) and 2.63 (1.86–3.74), respectively (P for trend <0.001). This association did not change after adjusting for urbanization, education, cigarette use, alcohol consumption and family history of hypertension (Model 2). The association also remained unchanged after further adjusting for weight change as a continuous variable (Model 3). The relationship holds true when using the World Health Organization cutoff categorization of BMI at age 25.
Table 5 shows the prevalence and ORs of hypertension based on the weight change categories. The prevalence of hypertension for the six weight change categories of <−7.5 kg; −7.5 to −2.6 kg; −2.5 to 2.5 kg; 2.6 to 7.5 kg; 7.6 to 12.5 kg and >12.5 kg was 16.0%, 15.0%, 15.4%, 21.0%, 27.1% and 40.0%, respectively. In an age- and sex-adjusted analysis (Model 1) and multivariate-adjusted analysis (Model 2), weight gain of 2.6 kg or more during adulthood was associated with a higher risk of hypertension than that of the stable weight group. However, weight loss was not significantly associated with risk of hypertension in Model 1 and Model 2. In addition, we adjusted for BMI at age 25 as a continuous variable in Model 3, and the trend was consistent with the trends exhibited in Model 1 and Model 2. In addition, the ORs (95% CI) for the two weight loss groups (−7.5 to −2.6 kg and <−7.5 kg) were 0.77 (0.65–0.91) and 0.58 (0.47–0.72), respectively, indicating that weight loss during adulthood was associated with a lower risk of hypertension.
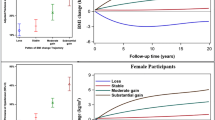
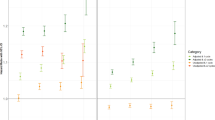
We also present the results stratified by baseline age (Figure 2a and b). The associations between BMI at age 25 and adult weight change, and risk of hypertension were consistent across the age groups (all P-values for trend <0.001).
Odds ratios for hypertension according to BMI at age 25 and weight change since age 25 in each age group (years). Both a and b were adjusted for age, sex, urbanization, education level, smoking status, drinking status and family history of hypertension. a was additionally adjusted for weight change as a continuous variable and b was additionally adjusted for BMI at age 25 as a continuous variable. BMI, body mass index.
We stratified the association between weight change and hypertension by BMI at age 25 (Table 6). We found that weight gain of 2.6–7.5 kg in the normal weight groups (BMI 18.5–20.9 and 21–23.9 kg m−2) and weight gain of more than 7.5 kg in each group were consistently associated with a higher risk of hypertension. We also found that among normal weight participants with BMI 21–23.9 kg m−2 at age 25, weight loss of 7.5 kg or more reduced the risk of hypertension. For overweight or obese participants (BMI⩾24 kg m−2), weight loss of 2.6 kg or more significantly reduced the risk of hypertension. Specifically, the ORs (95% CI) for weight loss of 2.6 to 7.5 kg and >7.5 kg were 0.63 (0.46–0.86) and 0.45 (0.32–0.63), respectively. Notably, however, weight loss was not significantly associated with the risk of hypertension for participants with BMI<21 kg m−2 at age 25.
Discussion
In this large-scale population study, we found that being overweight or obese at age 25 and weight gain were significantly associated with increased risk of hypertension in middle-aged Chinese men and women. Even moderate weight gain from early adulthood to middle age was associated with a higher risk of hypertension. These findings are consistent with the results of The Nurses’ Health Study, which reported that higher BMI at age 18 was associated with an increased risk of hypertension later in life after controlling for age, subsequent weight change and other covariates. Weight gain since age 18 was also associated with a significantly higher risk of hypertension.13 Similarly, Lee et al.14 reported that long-term weight gain increased the risk of developing hypertension independent of age and BP level in Japanese males and females; the ORs (95% CI) were 2.48 (1.54–4.00) for males and 2.19 (1.24–3.87) for females.
In the present study, even moderate weight gain (2.5 to 7.6 kg) was associated with a higher risk of hypertension in middle age (OR, 1.66; 95% CI, 1.43 to 1.91). This result was consistent with the findings of The Nurses’ Health Study, which showed that women who gained 2.1 to 4.9 kg had a 29% increase in risk of hypertension, and women who gained 5.0–9.9 kg had a 74% increase in risk of hypertension.13 Kuwahara et al.19 conducted a long-term follow-up study in a Japanese community and found that steeper increases in BMI during childhood correlate with BP elevation in adolescence.19 Weight gain since early life has been attributed to the accumulation of subcutaneous and visceral fat.20 Possible mechanisms linking obesity to hypertension include the association of overweight and obesity with adipose tissue dysfunction, which is characterized by enlarged hypertrophied adipocytes, increased macrophage infiltration, and higher secretion of adipokines and free fatty acids. These factors result in chronic vascular inflammation, oxidative stress, activation of the renin–angiotensin–aldosterone system and sympathetic overdrive, which eventually lead to hypertension.21, 22, 23
Given the wide range of participants’ ages (35–59 years), the time between age 25 and the baseline survey varied greatly. Therefore, we stratified participants by age (Figure 2a and b). Notably, a positive association between BMI at age 25 and the risk of hypertension was found in all age groups (all P-values for trend <0.001), indicating that the association between weight change and hypertension remained regardless of the time between age 25 and the baseline survey.
In a stratified analysis by BMI at age 25 category, we found that weight gain of 2.6–7.5 kg increased the risk of hypertension for normal weight participants and weight gain of more than 7.5 kg increased the risk of hypertension in each BMI group. These findings indicate that weight gain during adulthood increased the risk of hypertension in middle age regardless of BMI at age 25. In addition, weight loss (even moderate weight loss) could reduce the risk of hypertension for participants who were overweight or obese at age 25. For participants with higher normal weight, weight loss reduced the risk of hypertension only when it was >7.5 kg. By contrast, for participants who were underweight or had a lower normal weight, weight loss did not reduce the risk of hypertension in this study. One possible explanation is that weight loss in participants with a lower BMI may experience a disproportionate reduction of lean mass relative to fat mass.
Our study has several strengths. First, in this retrospective cohort design, we enrolled a large population-based sample, including male and female participants from China. Second, to the best of our knowledge, this is the first study focusing on the relationship between overweight or obesity in early adulthood and long-term adult weight change and hypertension in the Chinese population.
Our study also has several potential limitations. First, our analyses relied on self-reported and recalled weight at 25 years of age instead of measured values. Although some validation studies in other cohorts have shown that self-reported weights are highly correlated with measured weights,24, 25 a previous study suggested that there is a systematic tendency for heavy persons to underestimate their weight and, conversely, for thin persons to overestimate their weight.26 The weight at age 25 and BMI at the time of the survey results in our study could be affected by the 'regression to the mean' phenomenon. Thus, the relationship between overweight or obesity in early adulthood and the risk of hypertension could be underestimated. However, the relationship between weight gain and risk of hypertension may be overestimated. Second, BP was measured three times on a single occasion in our study, which might affect the accuracy of the diagnosis of hypertension. Third, given that end-digit preference is common in BP measurements and may directly influence the diagnosis of hypertension,27 we analyzed the frequency of end-digit preference and found a mild ‘0’ preference in both the SBP and DBP measurements. The percentages of ‘0’ preference were 27.5% for the SBP measurement and 28.5% for the DBP measurement, which deviated by 7.5% and 8.5%, respectively, from the expected 20%. Although, according to Ataman et al.,28 the frequency of the terminal number should not deviate by more than 5% from the expected 20%, the ‘0’ preference in our study is much lower than in other large-scale population studies.27, 29 Finally, we did not collect reasons for weight change during adulthood; as a result, the relationship between weight change, and weight loss in particular, and hypertension cannot be further explained.
In summary, overweight and obesity in early adulthood and adult weight gain were both independently associated with marked increase in the risk of hypertension in the middle-aged Chinese men and women. Long-term weight loss could reduce the risk of hypertension for people with a higher BMI in early adulthood, but it did not reduce the risk of hypertension for people who were underweight or had a lower normal BMI in early adulthood.
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E . Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781.
Nguyen T, Lau DC . The obesity epidemic and its impact on hypertension. Can J Cardiol 2012; 28: 326–333.
Fujii M, Ohnishi H, Saitoh S, Akasaka H, Miura T, Mori M . The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno-Sobetsu study. Hypertens Res 2015; 38: 426–432.
Kannel WB . Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA 1996; 275: 1571–1576.
Grundy SM, Balady GJ, Criqui MH, Fletcher G, Greenland P, Hiratzka LF, Houston-Miller N, Kris-Etherton P, Krumholz HM, LaRosa J . Primary prevention of coronary heart Disease: guidance from Framingham. A Statement for healthcare professionals from the AHA task force on risk reduction. Circulation 1998; 97: 1876–1887.
Cassano PA, Segal MR, Vokonas PS, Weiss ST . Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol 1990; 1: 33–48.
Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA . Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 2001; 161: 1581–1586.
Matsuo T, Sairenchi T, Suzuki K, Tanaka K, Muto T . Long-term stable obesity increases risk of hypertension. Int J Obes (Lond) 2011; 35: 1056–1062.
Lee SK, Kim SH, Cho GY, Baik I, Lim HE, Park CG, Lee JB, Kim YH, Lim SY, Kim H, Shin C . Obesity phenotype and incident hypertension: a prospective community-based cohort study. J Hypertens 2013; 31: 145–151.
Garrison RJ, Kannel WB, Stokes JR, Castelli WP . Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med 1987; 16: 235–251.
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS . Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg 2008; 207: 928–934.
Nagai M, Ohkubo T, Murakami Y, Takashima N, Kadota A, Miyagawa N, Saito Y, Nishi N, Okuda N, Kiyohara Y, Nakagawa H, Nakamura Y, Fujiyoshi A, Abbott RD, Okamura T, Okayama A, Ueshima H, Miura K . Secular trends of the impact of overweight and obesity on hypertension in Japan, 1980–2010. Hypertens Res 2015; 38: 790–795.
Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, Colditz GA . Body weight, weight change, and risk for hypertension in women. Ann Intern Med 1998; 128: 81–88.
Lee JS, Kawakubo K, Kashihara H, Mori K . Effect of long-term body weight change on the incidence of hypertension in Japanese men and women. Int J Obes Relat Metab Disord 2004; 28: 391–395.
Zhou B, Wu Y, Yang J, Li Y, Zhang H, Zhao L . Overweight is an independent risk factor for cardiovascular disease in Chinese populations. Obes Rev 2002; 3: 147–156.
Zhang LF, Yang J, Hong Z, Yuan GG, Zhou BF, Zhao LC, Huang YN, Chen J, Wu YF . Proportion of different subtypes of stroke in China. Stroke 2003; 34: 2091–2096.
Bei Fan Z . Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Asia Pac J Clin Nutr 2002; 11: S685–S693.
WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157–163.
Kuwahara E, Asakura K, Nishiwaki Y, Komatsu H, Nakazawa A, Ushiku H, Maejima F, Nishigaki Y, Hasegawa T, Okamura T, Takebayashi T . Steeper increases in body mass index during childhood correlate with blood pressure elevation in adolescence: a long-term follow-up study in a Japanese community. Hypertens Res 2014; 37: 179–184.
Ginsberg HN, Zhang YL, Hernandez-Ono A . Metabolic syndrome: focus on dyslipidemia. Obesity (Silver Spring) 2006; 14 ((Suppl 1)): 41S–49S.
Hall JE, Do CJ, Da SA, Wang Z, Hall ME . Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res 2015; 116: 991–1006.
Pieterse C, Schutte R, Schutte AE . Leptin links with plasminogen activator inhibitor-1 in human obesity: the SABPA study. Hypertens Res 2015; 38: 507–512.
Kim H, Kim HJ, Shin N, Han M, Park H, Kim M, Kwon H, Choi SY, Heo NJ . Visceral obesity is associated with microalbuminuria in nondiabetic Asians. Hypertens Res 2014; 37: 679–684.
Perry GS, Byers TE, Mokdad AH, Serdula MK, Williamson DF . The validity of self-reports of past body weights by U.S. adults. Epidemiology 1995; 6: 61–66.
Tamakoshi K, Yatsuya H, Kondo T, Hirano T, Hori Y, Yoshida T, Toyoshima H . The accuracy of long-term recall of past body weight in Japanese adult men. Int J Obes Relat Metab Disord 2003; 27: 247–252.
Schlichting P, Hoilund-Carlsen PF, Quaade F . Comparison of self-reported height and weight with controlled height and weight in women and men. Int J Obes 1981; 5: 67–76.
Jie G, Jian W, Qiaowen H, Shanzhu Z . Investigation of end-digit preference in blood pressure records of hospitalized Chinese patients and analysis of risk factors. Postgrad Med 2012; 124: 53–57.
Ataman SL, Cooper R, Rotimi C, McGee D, Osotimehin B, Kadiri S, Kingue S, Muna W, Fraser H, Forrester T, Wilks R . Standardization of blood pressure measurement in an international comparative study. J Clin Epidemiol 1996; 49: 869–877.
de Lusignan S, Belsey J, Hague N, Dzregah B . End-digit preference in blood pressure recordings of patients with ischaemic heart disease in primary care. J Hum Hypertens 2004; 18: 261–265.
Acknowledgements
We thank the participants in this study and all the staff of ChinaMUCA study for their support and assistance. This work was supported by the National Ninth Five-Year Plan Science and Technology Key Projects of the People’s Republic of China (grant 96–906–02–01).
Author contributions
L Zhao, YW and L Zhou designed the study; L Zhao, YL and MG collected the data; and L Zhou performed the data analysis and drafted the manuscript. All authors were involved in writing the paper and gave final approval for the submission of the current version, and L Zhao has primary responsibility for the final manuscript content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhou, L., Li, Y., Guo, M. et al. Relations of body weight status in early adulthood and weight changes until middle age with hypertension in the Chinese population. Hypertens Res 39, 913–918 (2016). https://doi.org/10.1038/hr.2016.80
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.80
Keywords
This article is cited by
-
Hypertension in China: epidemiology and treatment initiatives
Nature Reviews Cardiology (2023)
-
Association between age at menarche and blood pressure in adulthood: is obesity an important mediator?
Hypertension Research (2018)
-
Body mass index, abdominal fatness, and hypertension incidence: a dose-response meta-analysis of prospective studies
Journal of Human Hypertension (2018)
-
The relationship between obesity and hypertension: an updated comprehensive overview on vicious twins
Hypertension Research (2017)