Abstract
Our preclinical study demonstrated that esmolol produces early regression of left ventricular hypertrophy in arterial hypertension. The aim of this study was to assess the effects of short-term esmolol therapy on the regression of left anterior descending artery remodeling in spontaneously hypertensive rats (SHRs), and to determine whether the asymmetric dimethylarginine (ADMA)/dimethylarginine dimethylaminohydrolase (DDAH) pathway, a regulator of nitric oxide (NO) bioavailability, accounted for this regression. Fourteen-month-old male SHRs were treated intravenously with vehicle (SHR, n=15) or esmolol (SHR-E, n=20) (300 μg kg−1 min−1). Age-matched, vehicle-treated male Wistar-Kyoto rats (WKY, n=15) served as controls. SHRs were also treated with nitroglycerin (SHR-N, n=5). After 48 h, the left anterior descending artery structure and morphology were assessed, and dose–response curves for 5-hydroxytryptamine (5-HT, 10−9–3 × 10−5 mol l−1) were constructed. ADMA concentrations in plasma and left ventricle and DDAH activity in tissue were analyzed. Wall thickness and cross-sectional area were significantly lower after treatment with esmolol in SHR-E than in SHR. Media thickness and smooth muscle cell count were lower in SHR-E than in SHR. Esmolol induced a significant reduction in adventitial cell count in SHR-E. The area under the concentration–response curves was significantly higher in SHR than in SHR-E, as were the esmolol normalized coronary artery contracting responses to 5-HT. We found significantly lower ADMA levels and significantly higher DDAH activity in the ventricle in SHR-E than in SHR. The protective effect of esmolol on the regression of left anterior descending artery remodeling may be related to the reduction in ADMA levels.
Similar content being viewed by others
Introduction
Esmolol is an ultrashort-acting cardioselective β-adrenergic blocker that is widely used for the short-term treatment of tachyarrhythmias and hypertension.1, 2 The results of underpowered studies suggested that esmolol reduces perioperative ischemia.3 In a preclinical study, we showed that esmolol produces early regression of left ventricular hypertrophy in arterial hypertension.4 The pharmacodynamic and pharmacokinetic profiles of this drug make it a suitable cardioprotective agent.1, 5 Myocardial infarction is a cause of perioperative morbidity and mortality. The etiology of perioperative myocardial infarction includes prolonged ischemia resulting from tachycardia or hypertension. Some surgical procedures can increase myocardial oxygen demand and aggravate myocardial ischemia.2 Esmolol is a safe and effective agent that reduces myocardial oxygen consumption by decreasing the heart rate (HR) and thus improving coronary perfusion. Therefore, it could be used to decrease the incidence of arrhythmias and myocardial ischemia.3 The rapid onset of action of esmolol (2 min) and its short elimination half-life (approximately 9 min) make it the ideal perioperative agent for the short-term treatment of hypertension and tachycardia and for clinical situations that require easy unblocking of β-receptors because esmolol minimizes the risk of hypotension and bradycardia.2
Structural and functional changes in the arterial vasculature in hypertension could have a critical role in the progression of vascular disease and be reversible with effective drug therapy.6 Appropriate drugs could target mechanisms that appear to contribute to vascular remodeling in hypertension, namely asymmetric dimethylarginine (ADMA).7 As an endogenously-formed nitric oxide (NO) inhibitor, ADMA is associated with essential hypertension.8 Increasing ADMA concentrations are an independent risk factor for cardiovascular death in patients with coronary artery disease.9, 10
Our group previously demonstrated that esmolol produces changes on intramyocardial artery morphology by increasing the bioavailability of NO and superoxide dismutase activity in spontaneously hypertensive rats (SHRs).11 Interestingly, this treatment effect was achieved more quickly with esmolol (48 h) than with classic antihypertensive treatments.12, 13, 14 However, we could not conclude that regression of vascular remodeling occurred because we did not study modifications at the cellular level and markers of smooth muscle proliferation.
The first objective of the present study was to determine the effect of esmolol on artery wall structure, including gross structural differences and modifications at the cellular level, and the contracting pharmacological response in anterior descending coronary artery remodeling in SHR. The second objective was to determine whether the ADMA/dimethylarginine dimethylaminohydrolase (DDAH) pathway, as a regulator of NO bioavailability, could account for the regression of coronary artery remodeling after treatment with esmolol.
Methods
All procedures fulfilled the stipulations of the Guide for the Care and Use of Laboratory Animals (Directive 2010/63/UE and RD 53/2013) and were approved by the Ethics Committee of Hospital General Universitario Gregorio Marañon, Madrid, Spain (PROEX 223/14).
Animals and experimental protocols
The 14-month-old male SHR (n=40) and normotensive control Wistar-Kyoto (WKY) rats (n=15) were bred at the animal house of Universidad Autónoma de Madrid, Madrid, Spain. All rats were supplied with standard rat chow and drinking water ad libitum and were maintained on a 12-h/12-h light/dark cycle. The animals were housed at a constant temperature of 24 °C and a relative humidity of 40%. They were anesthetized with an i.p. injection of diazepam 10 mg kg−1 (Valium 10 mg ml−1; Roche Pharmaceuticals, Madrid, Spain) and ketamine 80 mg kg−1 (Ketolar 50 mg ml−1; Parke-Davis, Madrid, Spain), and a catheter was inserted into the right internal jugular vein. SHRs were divided into two groups: rats treated with esmolol (SHR-E) and rats treated with vehicle (SHR, hypertensive control group). A third group contained SHRs treated with nitroglycerin (SHR-N). SHR-E received an i.v. infusion of esmolol at 300 μg kg−1 min−1 (Breviblock 10 mg ml−1; Baxter, Lessines, Belgium) for 48 h, and SHR-N received an i.v. infusion of nitroglycerin at 0.5 mg h−1 for 48 h as described previously.4 Control SHR and WKY received saline solution (vehicle). After 48 h of treatment, blood samples were taken to study the ADMA levels. Rats were sedated with an i.p. injection of diazepam 10 mg kg−1 and ketamine 80 mg kg−1 and killed by decapitation. The left ventricle was immediately removed to measure the ADMA levels, and the coronary arteries were dissected to perform vascular reactivity experiments and study vascular structure.
Systolic arterial pressure and HR measurements
Systolic arterial pressure (SAP) and HR were measured using the tail-cuff method with a photoelectric sensor (Niprem 546; Cibertec, Madrid, Spain). Several determinations were made, and the findings were considered valid if 10 consecutive measurements were within 10 mm Hg of each other.
Confocal microscopy study of the left anterior descending coronary artery
Each group contained five animals. Confocal microscopy was used to assess wall thickness (intima+media), internal and external perimeter and cross-sectional area (CSA) in left anterior descending coronary artery segments (1 mm in length). We also studied thickness, cell count and cell density in the adventitia and media.
Briefly, the segments were fixed in 4% paraformaldehyde before being washed in 9% saline solution and stained with the nuclear dye DAPI (1:500 of a 5-mg ml−1 stock solution). A ring and two longitudinal sections were cut from each segment and mounted on a slide provided with a small well made of spacers to avoid vessel compression. The well was filled with mounting medium (Citifluor, Aname, Spain). One longitudinal section was mounted with the endothelial side up and the other with the adventitial side up, and they were viewed with a Leica TCS SP2 confocal system (Leica Microsystems, Wetzlar, Germany) at excitation 405 nm/emission 410–475 nm to visualize the cell nuclei. In each artery, three randomly selected regions were visualized with a × 20 objective at zoom 8. In each of these regions, stacks of 1 μm serial optical sections were captured from the adventitial and media layers. The rings were visualized with a × 20 objective at the 488-nm/515-nm line, and an image was captured to quantify the internal and external diameters. Several images were also captured with a × 20 objective at zoom 2 to quantify the thickness in the ring section.
Quantitative analysis was performed using the MetaMorph Image Analysis Software (Universal Imaging, Wokingham, UK) as previously described.15 The thickness of each layer in μm was determined by the number of planes between the first image showing an adventitial cell and the last image showing a smooth muscle cell (SMC) at their maximum intensities, as well as between the first image showing the first SMC and the last image showing the first endothelial cell. Adventitial cells and SMCs were counted in a specific volume defined by the image area (8731.03 μm2 for a × 20 objective at zoom 8) and the layer thickness of each particular vessel. Data are expressed as adventitial and media cellular density. The CSA (intima+media) of each vessel was calculated from the internal and external perimeters measured from images captured with the × 20 objective.
Contracting responses of the left anterior descending coronary artery
We analyzed five animals from each group. The heart was removed and maintained in cold (4 °C) oxygenated Krebs-Henseleit solution (KHS, in mmol l−1: 115 NaCl, 25 NaHCO3, 4.7 KCl, 1.2 MgSO4⋅7H2O, 2.5 CaCl2, 1.2 KH2PO4, 11.1 glucose and 0.01 Na2EDTA). Segments of the left anterior descending coronary artery were isolated, and the surrounding cardiac tissue was cleaned under a dissecting microscope. Segments of coronary arteries of 2 mm in length were mounted on a wire myograph (Multi Myograph System, model 610M; Danish Myo-Technology, Atlanta, GA, USA) coupled to a Powerlab data acquisition system (AD Instruments, Castle Hill, NSW, Australia) and studied as described previously.16 Briefly, the vessel was mounted in oxygenated KHS and set to a normalized internal circumference of 0.9L100, which was considered the effective lumen diameter that represented the basal tone of the artery. After an equilibration period in KHS at 37 °C and pH 7.4, segments were stretched to their optimal lumen diameter to develop active tension. Coronary arteries were exposed to 120 mmol l−1 K+-KHS to ensure their functional integrity. After a washout period of 60 min, concentration–response curves after application of 5-hydroxytryptamine (5-HT, 10−9–3 × 10−5 mol l−1) were plotted for the same arteries. Contraction with 5-HT was expressed as a percentage of the maximum response of the arteries to K+-KHS.
Determination of ADMA and symmetric dimethylarginine concentrations in plasma and left ventricle and DDAH activity in tissue
We analyzed 5 animals for each control group (WKY and SHR) and 10 animals treated with esmolol. Blood (2.4 ml) was collected from each animal in Vacutainer tubes (BD, Plymouth, UK) containing citrate (300 μl). Samples were centrifuged at 900 g and 4 °C for 10 min to obtain plasma, which was aliquoted and stored at –80 °C for further analysis. We studied ADMA and symmetric dimethylarginine (SDMA) concentrations in serum and the left ventricle, whereas DDAH activity was measured only in the left ventricle.
Measurement of ADMA and SDMA
Mass spectrometry of ADMA and SDMA was performed as previously described using a fully-validated high-throughput liquid chromatography/tandem mass spectrometry (LC-MS/MS) assay.17, 18 In brief, samples were analyzed using a 96-well 0.20-μm microfiltration plate pre-coated with internal standards. After conversion to their butyl ester derivatives, analytes were evaluated on a Varian 1200L Triple Quadrupole mass spectrometer (Varian, Walnut Creek, CA, USA) in the positive electrospray ionization mode.
Measurement of DDAH activity in tissue
DDAH activity in rat ventricles was determined as previously described.19 In brief, to minimize possible interference by endogenously-formed ADMA, tissue samples were homogenized in PBS buffer with protease inhibitor. The homogenate was centrifuged (4 °C) for 5 min at 12 000 g. Fifty microliter aliquots of the resulting supernatant were added to 50 μl aliquots of PBS buffer containing 20 μm [2H6]-ADMA. After incubation at 37 °C for 60 min, the reactions were stopped, and the remaining [2H6]-ADMA was measured using LC-MS/MS as described above.
Statistical analysis
The results were expressed as the mean±s.e.m. The parameters were compared using repeated measures analysis of variance (physiological and concentration–response curves parameters) and the t-test for independent samples. To compare the contracting responses of 5-HT in coronary segments, some results were expressed as differences in the area under the concentration–response curves (AUC) among the experimental groups. P-values <0.05 were considered as statistically significant. The statistical analysis was performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp, Armonk, NY, USA) and S-PLUS 6.1.
Results
Blood pressure, HR and weight
Weight was significantly higher in WKY than in SHR (414.21±17.02 g vs. 382.15±14.02 g, P<0.05), although no statistically significant differences were detected between SHR, SHR-E and SHR-N (382.15±14.02 g vs. 371.48±15.24 g vs. 375.21±11.31 g).
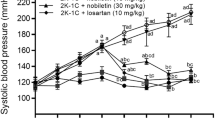
SAP was significantly higher in SHR than in WKY controls. Esmolol significantly reduced SAP in SHR-E (Figure 1a). SHR-N showed the same reduction in SAP as SHR-E. HR remained unchanged in SHR, SHR-N and WKY, but decreased after treatment in SHR-E compared with SHR, SHR-N and WKY (Figure 1b).
Changes in systolic arterial pressure (a) and heart rate (b) from Wistar-Kyoto control rats (WKY, n=10), spontaneously hypertensive control rats (SHR, n=10), spontaneously hypertensive rats treated with esmolol (SHR-E, n=10) and spontaneously hypertensive rats treated with nitroglycerin (SHR-N, n=5). Data were obtained at 0, 12, 24, 36 and 48 h of treatment. Data are expressed as the mean±s.e.m. The parameters were compared using repeated measures analysis of variance. Statistically significant differences between WKY, SHR, and SHR-E and SHR-N are shown (∗P<0.05 vs. WKY; ∗∗P<0.01 vs. WKY; #P<0.05 vs. SHR; ##P<0.01 vs. SHR; §§P<0.01 vs. SHR-E).
Effect of esmolol on vascular structure
Figure 2 shows the structural parameters of the left anterior descending coronary artery for WKY, SHR and SHR-E. The external diameter of the coronary artery was greater in SHR than in WKY. Esmolol administered to SHR-E caused a significant decrease in external diameter compared with SHR (Figure 2b). The internal diameter was similar in SHR and SHR-E, although it was higher in both than in WKY (Figure 2b). The wall thickness (tunica intima+media) of this artery was greater in SHR than in WKY. Wall thickness was significantly lower after 48 h of treatment with esmolol in SHR-E than in SHR and showed no differences with respect to WKY (Figures 2a and b). Arterial CSA was larger in the SHR than in the WKY. However, after treatment with esmolol, CSA was significantly smaller in SHR-E than in SHR (Figure 2b). There were no significant differences in external diameter, internal diameter, wall thickness or CSA in either SHR or SHR-N. Administration of esmolol to SHR-E caused a decrease in wall thickness, external diameter and CSA in comparison with SHR-N (Figures 2a and b).
Medial thickness (tunica intima+media) of the left anterior descending artery rings (representative examples of projections obtained from confocal microscopy images, × 20, zoom 2) (a) and structural parameters (tunica intima+media) in the left anterior descending artery (b) from Wistar-Kyoto control rats (WKY, n=5), spontaneously hypertensive control rats (SHR, n=5), spontaneously hypertensive rats treated with esmolol (SHR-E, n=5) and spontaneously hypertensive rats treated with nitroglycerin (SHR-N, n=5). Data are expressed as the mean±s.e.m. Between-group comparisons were based on the t-test for independent samples. Statistically significant differences between WKY, SHR, and SHR-E and SHR-N are shown (∗P<0.05 vs. WKY; ∗∗P<0.01 vs. WKY; ∗∗∗P<0.001 vs. WKY; #P<0.05 vs. SHR; §P<0.05 vs. SHR-E; §§P<0.01 vs. SHR-E).
Effect of esmolol on vascular wall morphology
Figure 3 shows the morphology parameters of the left anterior descending coronary artery wall. The media was significantly thicker in SHR than in WKY. This parameter was significantly lower after 48 h of treatment in SHR-E than in SHR (Figure 3a). The SMC count was significantly higher in the media layer in SHR than in WKY, although esmolol led to a lower SMC count in SHR-E than in SHR (Figures 3a and b). Consequently, no significant differences in cell density were detected between SHR-E and SHR (Figure 3a). No differences in media thickness, SMC count or SMC density were found between the SHR-E and the WKY. There were no significant differences in the media layer (wall thickness, SMC count and cell density) between SHR and SHR-N. In comparison with SHR-N, administration of esmolol to SHR-E caused a decrease in media thickness and SMC count.
Media thickness, media cell number and media cell density (a) in left anterior descending artery segments from Wistar-Kyoto control rats (WKY, n=5), spontaneously hypertensive control rats (SHR, n=5), spontaneously hypertensive rats treated with esmolol (SHR-E, n=5) and spontaneously hypertensive rats treated with nitroglycerin (SHR-N, n=5). Representative examples of projections of the media layer obtained from confocal microscopy images (× 20, zoom 8) (b). Adventitial thickness, adventitial cell count and adventitial cell density (c) in left descending anterior artery segments from Wistar-Kyoto control rats (WKY, n=5), spontaneously hypertensive control rats (SHR, n=5), spontaneously hypertensive rats treated with esmolol (SHR-E, n=5) and spontaneously hypertensive rats treated with nitroglycerin (SHR-N, n=5). Representative examples of projections of the adventitial layer obtained from confocal microscopy images (× 20, zoom 8) (d). Data are expressed as the mean±s.e.m. Between-group comparisons were based on the t-test for independent samples. Statistically significant differences between WKY, SHR, SHR-E and SHR-N are shown (∗P<0.05 vs. WKY; ∗∗P<0.01 vs. WKY; ∗∗∗P<0.001 vs. WKY; #P<0.05 vs. SHR; ##P<0.01 vs. SHR; ###P<0.001 vs. SHR; §P<0.05 vs. SHR-E; §§P<0.01 vs. SHR-E).
No significant differences in adventitial thickness were observed between the experimental groups (Figure 3c). The adventitia contained significantly more cells in SHR than in WKY. However, treatment with esmolol induced a significant reduction in the cell count in SHR-E compared with SHR. No differences in this respect were observed between SHR-E and WKY (Figures 3c and d). Consequently, adventitial cell density was higher in SHR than in WKY, although esmolol decreased this parameter in SHR-E with respect to SHR. No differences in adventitial cell density were found between SHR-E and WKY (Figure 3c). There were no significant differences between SHR and SHR-N in the adventitial layer (wall thickness, cell count and cell density). In comparison with SHR-N, the administration of esmolol to SHR-E caused a decrease in cell count. No significant differences in wall thickness were found between SHR-E and SHR-N.
Effect of esmolol on contracting responses
Effective lumen diameter at 0.9L100 was significantly smaller in the WKY coronary arteries than in those of SHR and SHR-E (Figure 4a). The contractile response to 5-HT (10−7–3 × 10−5 mol l−1) in the left anterior descending coronary artery was higher in SHR than in WKY. Interestingly, esmolol reduced the contraction (10−7–3 × 10−5 mol l−1) of this artery in SHR-E compared with SHR. Coronary artery contracting responses induced by 5-HT returned to normal values after treatment with esmolol at all concentrations (Figure 4b).
Effective lumen diameter (a) and 5-hydroxytryptamine (5-HT, 10−9–3 × 10−5 mol l−1) responses (b) in the left descending anterior artery from Wistar-Kyoto control rats (WKY, n=5), spontaneously hypertensive control rats (SHR, n=5) and spontaneously hypertensive rats treated with esmolol (SHR-E, n=5). Contraction to 5-HT was expressed as a percentage of the maximum response of the arteries to K+-KHS. Data are expressed as the mean±s.e.m. The parameters were compared using repeated measures analysis of variance. Statistically significant differences between WKY, SHR and SHR-E are shown (∗P<0.05 vs. WKY; ∗∗P<0.01 vs. WKY; ∗∗∗P<0.001 vs. WKY; #P<0.05 vs. SHR; ##P<0.01 vs. SHR; ###P<0.001 vs. SHR).
The AUC was significantly larger in SHR than in WKY (AUC SHR=269.36±23 vs. AUC WKY=47.99±19, P=0.00001). AUC was significantly higher in SHR than in SHR-E (AUC SHR=269.36±23 vs. AUC SHR-E=22.14±1, P=0.00003). No differences were observed between SHR-E and WKY.
Effect of esmolol on left ventricle concentrations of ADMA, SDMA and DDAH
A significantly higher ADMA concentration and decreased DDAH activity was observed in SHR compared with WKY. Importantly, we found a significantly lower ADMA concentration (Figure 5a) and a significantly higher DDAH concentration in the left ventricle in SHR-E than in SHR (Figure 5c). Ventricular ADMA and DDAH values returned to normal after treatment with esmolol. No significant differences were found for SDMA between SHR, WKY and SHR-E (Figure 5b).
ADMA (a), SDMA (b) and DDAH activity (c) in the left ventricles of Wistar-Kyoto control rats (WKY, n=4), spontaneously hypertensive control rats (SHR, n=4) and spontaneously hypertensive rats treated with esmolol (SHR-E, n=6). ADMA (d) and SDMA (e) in plasma from Wistar-Kyoto control rats (WKY, n=5), spontaneously hypertensive control rats (SHR, n=5) and spontaneously hypertensive rats treated with esmolol (SHR-E, n=10). Data are expressed as the mean±s.e.m. Between-group comparisons were based on the t-test for independent samples. Statistically significant differences between WKY, SHR and SHR-E are shown (∗P<0.05 vs. WKY; #P<0.05 vs. SHR; ##P<0.01 vs. SHR; ###P<0.001 vs. SHR).
Effect of esmolol on serum concentrations of ADMA and SDMA
Serum concentrations of ADMA were higher in SHR than in WKY. Treatment with esmolol significantly decreased serum concentrations of ADMA (Figure 5d). There were no significant differences in SDMA concentrations between SHR, WKY and SHR-E (Figure 5e).
Discussion
In the present study, we show that short-term (48 h) i.v. infusion of esmolol (300 μg kg−1 min−1) in adult SHR induces early regression of coronary artery remodeling, and this effect may be associated with the ADMA/DDAH pathway. Although previous studies have demonstrated that antihypertensive drugs can reverse coronary artery remodeling, they have all been conducted with long-term drug administration.12, 13, 14 Ours is the first study to show early regression in coronary artery remodeling by decreased ADMA with short-term administration of a β-blocker.
Several studies show changes in coronary artery remodeling (structure and morphology) with antihypertensive therapy.12, 13, 14, 20 Administration of lizard's over 5 weeks reduced wall thickness and CSA in SHR.12 Amlodipine and enalapril led to a reduction in media thickness, media CSA and number of SMCs in SHR after 12 weeks.13 Perindopril and indapamide led to a reduction in coronary artery CSA and vessel diameter in SHR after 8 weeks.14 The administration of lisinopril reduced the thickness of the intramyocardial coronary artery media in SHR after 12 weeks.20 No differential effects of esmolol (lower wall thickness and CSA, lower media thickness, decreased SMC count in media and decreased adventitial cell count) on coronary artery remodeling were observed compared with other antihypertensive agents, although a difference was found in the time of administration. Changes in structure and morphology were observed with esmolol after only 48 h.
Arterial hypertension could be responsible for the increase in media thickness and SMC growth, and these changes may mark differences in the vasoconstrictor responses.21 We suggest that the reduction in SMCs after treatment with esmolol might contribute to decreased contractile function. On the other hand, administration of esmolol to SHR corrected the adventitial cellular hyperplasia observed in SHR. This is important because the adventitia has a key role in vascular remodeling leading to cell proliferation.22
Vascular remodeling by antihypertensive therapy implies not only structural changes in the coronary artery but also changes in vascular reactivity, including a reduction in contracting responses. The response of the coronary artery to serotonin was less pronounced in WKY than in SHR, in agreement with the findings of other authors.23 It has also been suggested that responses to vasoconstrictors in the coronary artery are diminished24 in SHR or are similar in both SHR and WKY.25 The difference could be related to the contractile agent used, artery type and size, methodology and age.26 Vascular function (vasoconstrictor responses) was improved after treatment with esmolol. Other studies have demonstrated similar results, though after long-term antihypertensive therapy.27, 28
The early structural alterations in the coronary artery (decreased media thickness) produced by esmolol could be explained by a reduction in media SMCs. Esmolol led to morphological alterations in the coronary artery (reduction in the SMC count in the media layer) after only 48 h of treatment. These data correlate with the findings of other investigators, who demonstrated a reduction in aortic SMCs after 48 h of treatment with simvastatin29 and after 3 days of treatment with amlodipine30 in SHR. Simvastatin produced disturbing Ca2+ influx and RhoA activity and induced apoptosis of vascular SMCs.29 Reduced Akt-associated survival signaling (reduction in Akt phosphorylation from days 1 to 3) and activation of the extrinsic caspase-8-associated apoptotic pathway explain the regression of aortic remodeling with amlodipine in SHR immediately after the loss of medial SMCs via apoptosis (SMC apoptosis was rapid and massive).30 Therefore, antihypertensive therapy may contribute to the rapid regression of vascular remodeling via activation of a pro-apoptotic mechanism. In the present study, we do not know whether esmolol activated a pro-apoptotic mechanism, although the activation of the ADMA/DDAH/NO pathway could explain the early regression of vascular remodeling, with esmolol inhibiting the proliferation of SMCs. Based on a comparison with a group treated with nitroglycerin, our findings exclude the blood pressure-lowering effect of esmolol on vascular remodeling.
The ADMA/DDAH pathway is a critical regulator of NO signaling in vascular disease.31 NO is an important regulator of vascular remodeling, inhibiting SMC proliferation and producing vasodilatation. ADMA levels reduce NO production by inhibiting the activity of NOS, and therefore increasing the proliferation of vascular SMCs.32, 33 Previous studies have suggested that ADMA inhibits NO production, resulting in activation of RhoA and stress fibers through inhibition of PKG activity and reduction of RhoA phosphorylation at Ser 188, which in turn leads to angiogenic dysfunction.31
ADMA levels are regulated by DDAH, and DDAH2 is the isoform that is expressed in the vascular endothelium and heart. More than 90% of ADMA are eliminated by the action of DDAH. ADMA concentrations are elevated by impairment of DDAH activity, resulting in reduced NO generation on the one hand and the overexpression of DDAH activity on the other.34 To investigate the molecular mechanism underlying the reduction in ADMA levels after treatment with esmolol, we investigated DDAH levels in plasma and tissue. We observed lower DDAH levels in SHR than in WKY. Therefore, the impaired metabolism of ADMA as a result of reduced DDAH levels is a causal factor for the elevation of ADMA in SHR. We found that esmolol increased DDAH in SHR. We recently demonstrated that esmolol normalized endothelium-dependent relaxation in the left anterior descending coronary artery owing to increased bioavailability of NO and superoxide dismutase.11 Other drugs illustrate the key role of NO in cardioprotection through the increase in coronary blood flow by vasodilation.35 ADMA levels could also account for this improved bioavailability of NO. Nevertheless, a similar effect of esmolol on ADMA and DDAH2 has been reported for antihypertensive agents such as losartan and nebivolol in other vascular beds in SHR.36, 37 Nebivolol, a β1-receptor blocker antihypertensive drug that needs additional pharmacological actions to reduce blood pressure in the short term,38 reduces plasma ADMA levels in SHR by increasing its hydrolysis by DDAH2 and reducing its generation by reduced PRMT1 expression.37 Nebivolol reduces ADMA in endothelial cells by increasing DDAH2 activity, and this effect may be mediated by estradiol receptors, as nebivolol has estradiol-agonistic action in SHR and estradiol increases NOS by increasing DDAH2 activity and ADMA metabolism.39 The mechanism by which DDAH2 activity is increased by esmolol is unclear and warrants further examination.
The availability of esmolol, an ultrashort-acting parenteral β-adrenergic antagonist with a rapid onset and short elimination half-life that enables the rapid discontinuation of therapy, brings obvious advantages to the perioperative management of hypertension and tachycardia. Clinical studies performed during the perioperative period reveal that esmolol is safe and effective in this setting.1 Clinically, it is used in situations where brief adrenergic blockade is required, such as tracheal intubation and extubation and surgical stimuli, to prevent potentially serious complications in patients with cardiovascular disease40 and in critically ill or unstable patients where clinical conditions change rapidly and where early initiation of therapy, dosage changes and discontinuation of therapy may be necessary.2, 41 The efficacy of esmolol has also been established in patients with unstable angina, myocardial ischemia and supraventricular arrhythmias.2, 3
Remodeling of the coronary artery compromises organ function, thus increasing the cardiovascular morbidity and mortality of hypertension.42 The benefits of regression of structural and functional alterations in the coronary artery in patients with hypertension are important factors in the selection of antihypertensive therapy.43 In this study, we demonstrate the regression of coronary artery remodeling using a short course of therapy with esmolol in an experimental model with hypertension. If these results are confirmed in humans, then esmolol could be used for the treatment of coronary artery remodeling in patients with arterial hypertension in critical care units.
The present study is subject to limitations. This study was designed to analyze the effect of esmolol on ADMA in the regression of coronary artery remodeling in SHR. Endothelial disease is highly variable in SHR owing to differences in age, sex, artery type and methodology used for determination of vascular function.26 However, the results of our study apply only to the left anterior descending coronary artery in 14-month-old male SHR.
In summary, our results show that esmolol produces early regression of coronary artery remodeling, and this effect may be associated with the reduction in plasma and ventricular ADMA concentrations. Improved vascular wall structure (lower wall thickness and CSA) and morphology (lower media thickness, decreased SMC count in media and decreased adventitial cell count) and normalized contracting responses were observed in SHR-E compared with the control SHR. This is the first study to show the regression of coronary artery remodeling through the influence of the short-term administration of a β-blocker on ADMA.
References
Garnock-Jones KP . Esmolol: a review of its use in the short-term treatment of tachyarrhythmias and the short-term control of tachycardia and hypertension. Drugs 2012; 72: 109–132.
Wiest DB, Haney JS . Clinical pharmacokinetics and therapeutic efficacy of esmolol. Clin Pharmacokinet 2012; 51: 347–356.
Landoni L, Turi S, Biondi-Zoccai G, Bignami E, Testa V, Belloni L, Cornero G, Zangrillo A . Esmolol reduces perioperative ischemia in noncardiac surgery: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth 2010; 24: 219–229.
Quintana-Villamandos B, Delgado-Martos MJ, Sanchez-Hernandez JJ, Gómez de Diego JJ, Fernández-Criado MC, Canillas F, Martos-Rodríguez A, Delgado-Baeza E . Early regression of left ventricular hypertrophy after treatment with esmolol in an experimental rat model of primary hypertension. Hypertens Res 2013; 36: 408–413.
Yu SK, Tait G, Karkouti K, Wijeysundera D, McCluskey S, Beattie S . The safety of perioperative esmolol: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg 2011; 112: 267–281.
Rehman A, Schiffrin EL . Vascular effects of antihypertensive drug therapy. Curr Hypertens Rep 2010; 12: 226–232.
Feihl F, Liaudet L, Levy BI, Waeber B . Hypertension and microvascular remodelling. Cardiovas Res 2008; 78: 274–285.
Perticone F, Sciacqua A, Maio R, Perticone M, Maas R, Boger RH, Tripepi G, Tech S, Sesti G, Zoccali C . Asymmetric dimethylarginine, L-Arginine, and endothelial dysfunction in essential hypertension. J Am Coll Cardiol 2005; 46: 518–523.
Meinitzer A, Kielstein JT, Pilz S, Drechsler C, Ritz E, Boehm BO, Winkelmann BR, März W . Symmetrical and asymmetrical dimethylarginine as predictors for mortality in patients referred for coronary angiography: the Ludwigshafen Risk and Cardiovascular Health study. Clin Chem 2011; 57: 112–121.
Siegerink B, Maas R, Vossen CY, Schwedhelm E, Koenig W, Böger R, Rothenbacher D, Brenner H, Breitling LP . Asymmetric and symmetric dimethylarginine and risk of secondary cardiovascular disease events and mortality in patients with stable coronary heart disease: the KAROLA follow-up study. Clin Res Cardiol 2013; 102: 193–202.
Arnalich-Montiel A, González MC, Delgado-Baeza E, Delgado-Martos MJ, Condezo-Hoyos L, Martos-Rodríguez A, Rodríguez-Rodríguez P, Quintana-Villamandos B . Short-term esmolol improves coronary artery remodeling in spontaneously hypertensive rats through increased nitric oxide bioavailability and superoxide dismutase activity. Biomed Res Int 2014; 2014: 531087.
Koprdova R, Cebova M, Kristek F . Long-term effect of losartan administration on blood pressure, heart and structure of coronary artery of young spontaneously hypertensive rats. Physiol Res 2009; 58: 327–335.
Sharifi AM, Li JS, Endemann D, Schiffrin EL . Effects of enalapril and amlodipine on small-artery structure and composition, and on endothelial dysfunction in spontaneously hypertensive rats. J Hypertens 1998; 16: 457–466.
Neglia D, Fommei E, Varela-Carver A, Mancini M, Ghione S, Lombardi M, Pisani P, Parker H, D'amati G, Donato L, Camici PG . Perindopril and indapamide reverse coronary microvascular remodelling and improve flow in arterial hypertension. J Hypertens 2011; 29: 364–372.
Conde MV, Gonzalez MC, Quintana-Villamandos B, Abderrahim F, Briones AM, Condezo-Hoyos L, Regadera J, Susin C, Gomez de Diego JJ, Delgado-Baeza E, Diaz-Gil JJ, Arribas SM . Liver growth factor treatment restores cell-extracellular matrix balance in resistance arteries and improves left ventricular hypertrophy in SHR. Am J Physiol Heart Circ Physiol 2011; 301: H1153–H1165.
Conde MV, Marín J, Balfagón G . Superoxide anion and K+ channels mediate electrical stimulation-induced relaxation in the rat basilar artery. Eur J Pharmacol 1999; 372: 179–186.
Schwedhelm E, Tan-Andresen J, Maas R, Riederer U, Schulze F, Böger RH . Liquid chromatography-tandem mass spectrometry method for the analysis of asymmetric dimethylarginine in human plasma. Clin Chem 2005; 51: 1268–1271.
Schwedhelm E, Maas R, Tan-Andresen J, Schulze F, Riederer U, Böger RH . High-throughput liquid chromatographic-tandem mass spectrometric determination of arginine and dimethylated arginine derivatives in human and mouse plasma. J Chromatogr B Analyt Technol Biomed Life Sci 2007; 851: 211–219.
Maas R, Tan-Andreesen J, Schwedhelm E, Schulze F, Böger RH . A stable-isotope based technique for the determination of dimethylarginine dimethylaminohydrolase (DDAH) activity in mouse tissue. J Chromatogr B Analyt Technol Biomed Life Sci 2007; 851: 220–228.
Brilla CG, Janicki JS, Weber KT . Impaired diastolic function and coronary reservein genetic hypertension: Role of interstitial fibrosis and medial thickening of intramyocardial coronary arteries. Circ Res 1991; 69: 107–115.
Hüsken BC, van der Wal AC, Teeling P, Mathy MJ, Mertens MJ, Pul AJ, Pfaffendorf M, van Zwieten PA . Heterogeneity in morphological characteristics of coronary arteries and aortae in various models of hypertension. Blood Press 1997; 6: 242–249.
Rey FE, Pagano PJ . The reactive adventicia: fibroblast oxidase in vascular function. Arterioescler Thromb Vasc Biol 2002; 22: 1962–1971.
Su W, Guo Z, Deschepper CF, Randall DC, Gong MC . Dissociation of coronary artery contractile hyperreactivity from hypertension. Am J hypertens 2003; 16: 570–576.
Roque FR, Briones AM, García-Redondo AB, Galán M, Martínez-Revelles S, Avendaño MS, Cachofeiro V, Fernandes T, Vassallo DV, Oliveira EM, Salaices M . Aerobic exercice reduces oxidative stress and improves vascular changes of small mesenteric and coronary arteries in hypertension. Br J Pharmacol 2013; 168: 686–703.
Vázquez-Pérez S, Navarro-Cid J, de las Heras N, Cediel E, Sanz-Rosa D, Ruiloque LM, Cachofeiro V, Lahera V . Relevance of endothelium-derived hyperpolarizing factor in the effects of hypertension on rat coronary relaxations. J Hypertens 2001; 19: 539–545.
Bernatova I . Endothelial dysfunction in experimental models of arterial hypertension: Cause or consequence? Biomed Res Int 2014; 2014: 598271.
Miki S, Takeda K, Hatta T, Harada S, Kido H, Oguni A, Moriguchi J, Morimoto S, Kawa T, Sasaki S, Nakagawa M . Comparative effects of candesartan and enalapril on augmented vasoconstrictive responses to endothelin-1 in coronary vessels of spontaneously hypertensive rats. Am J Hypertens 2002; 15: 286–290.
Brilla CG, Janicki JS, Weber KT . Cardioreparative effects of lisinopril in rats with genetic hypertension and left ventricular hypertrophy. Circulation 1991; 83: 1771–1779.
Kang S, Woo HH, Kim K, Lim KM, Noh JY, Lee MY, Bae YM, Bae ON, Chung JH . Dysfunction of vascular smooth muscle and vascular remodeling by simvastatin. Toxicol Sci 2014; 138: 446–556.
Duguay D, deBlois D . Differential regulation of Akt, caspases and MAP kinases underlies smooth muscle cell apoptosis during aortic remodelling in SHR treated with amlodipine. Br J Pharmacol 2007; 151: 1315–1323.
Fiedler L . The DDAH/ADMA pathway is a critical regulator of NO signalling in vascular homeostasis. Cell Adh Migr 2008; 2: 149–150.
Sibal L, Agarwal SC, Home PD, Boger RH . The role of asymmetric dimethylarginine (ADMA) in endothelial dysfunction and cardiovascular disease. Curr Cardiol Rev 2010; 6: 82–90.
Cooke JP . ADMA: its role in vascular disease. Vasc Med 2005; 10 (Suppl 1): S11–S17.
Bai Y, Hui R . Dimethylarginine dimethylaminohydrolase (DDAH)-A critical regulator of hypertensive left ventricular hypertrophy? Med Hypotheses 2008; 70: 962–966.
Asanuma H, Sanada S, Asakura M, Asano Y, Kim J, Shinozaki Y, Mori H, Minamino T, Takashima S, Kitakaze M . Carperitide induces coronary vasodilation and limits infarct size in canine ischemic hearts: role of NO. Hypertens Res 2014; 37: 716–723.
Li D, Xia K, Li NS, Luo D, Wang S, Jiang DJ, Deng HW, Li YJ . Reduction of asymmetric dimethylarginine involved in the cardioprotective effect of losartan in spontaneously hypertensive rats. Can J Physiol Pharmacol 2007; 85: 783–789.
Wang Y, Zhang M, Liu Y, Liu Y, Chen M . The effect of nebivolol on asymmetric dimethylarginine system in spontaneously hypertensive rats. Vasc Pharmacol 2011; 54: 36–43.
Bertera FM, Del Mauro JS, Lovera V, Chiappetta D, Polizio AH, Taira CA, Höcht C . Enantioselective pharmacokinetics and cardiovascular effects of nebivolol in L-NAME hypertensive rats. Hypertens Res 2014; 37: 194–201.
Garbin U, Pasini AF, Stranieri C, Manfro S, Boccioletti V, Cominacini L . Nebivolol reduces asymmetric dimethylarginine in endothelial cells by increasing dimethylarginine dimethylaminohydrolase 2 (DDAH2) expression and activity. Pharmacol Res 2007; 56: 515–521.
Benfield P, Sorkin EM . Esmolol. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy. Drug 1987; 33: 392–412.
Schwartz M, Michelson EL, Sawin HS, MacVaugh H 3rd . Esmolol: safety and efficacy in postoperative cardiothoracic patients with supraventricular tachyarrhythmias. Chest 1988; 93: 705–711.
Intengan HD, Schiffrin EL . Vascular remodeling in hypertension: roles of apoptosis, inflammation, and fibrosis. Hypertension 2001; 38: 581–587.
Agabiti-Rosei E . Structural and functional changes of the microcirculation in hypertension: influence of pharmacological therapy. Drugs 2003; 63: 19–29.
Acknowledgements
This study was supported by a grant from the Spanish Health Ministry (Fondo de Investigaciones Sanitarias) under contract FIS 13/01261 and Fondos Feder.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Quintana-Villamandos, B., Arnalich-Montiel, A., Arribas, S. et al. Early regression of coronary artery remodeling with esmolol and DDAH/ADMA pathway in hypertensive rats. Hypertens Res 39, 692–700 (2016). https://doi.org/10.1038/hr.2016.57
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.57
Keywords
This article is cited by
-
Dronedarone induces regression of coronary artery remodeling related to better global antioxidant status
Hypertension Research (2019)