Abstract
Histone acetylation/deacetylation plays a key role in the epigenetic regulation of multiple pro-fibrotic genes. Here we investigated the effects of histone deacetyltransferase (HDAC) inhibition on angiotensin (Ang)-II-induced pro-fibrotic changes in adult mouse cardiac fibroblasts (CF). CF express class I HDACs 1 and 2, and Ang-II induces their activation. Notably, silencing HDAC1 or HDAC2 attenuated Ang-II induced CF proliferation and migration. Under basal conditions, HDAC1 dimerizes with HDAC2 in CF and Ang-II reversed this interaction. Treatment with Trichostatin A (TSA), a broad-spectrum HDAC inhibitor, restored their physical association, and attenuated Ang-II-induced MMP9 expression, IL-18 induction, and extracellular matrix (collagen I, collagen III and fibronectin) production. Further, TSA inhibited Ang-II-induced MMP9 and Il18 transcription by blocking NF-κB and AP-1 binding to their respective promoter regions. By inhibiting Sp1 binding to RECK promoter, TSA reversed Ang-II-induced RECK suppression, collagen and fibronectin expression, and CF migration and proliferation. The class I-specific HDAC inhibitor Mocetinostat (MGCD) recapitulated TSA effects on Ang-II-treated CF. Together, these results demonstrate that targeting HDACs attenuates the pro-inflammatory and pro-fibrotic effects of Ang-II on CF.
Similar content being viewed by others
Introduction
Acetylation of histone proteins contributes to chromatin condensation, blocks the binding of various transcriptional proteins to their cognate response elements in gene promoters and inhibits target gene induction. Acetylation/deacetylation of histones is regulated by the opposing activities of the histone acetyltransferases (HATs) and histone deacetyltransferases (HDACs). Mechanisms favoring histone acetyltransferases result in increased acetylation and downregulation of target gene expression. In most cases, deacetylation enhances transcription and gene induction.
Among the four major classes of HDACs, cardiac fibroblasts (CF) express class I HDACs 1 and 2.1 Several genes involved in the development and progression of fibrosis are regulated by acetylation, and the roles of HDAC inhibitors in cardiac fibrosis have been studied.2, 3, 4, 5, 6, 7 For example, induction of MMP9, which plays a role in extracellular matrix (ECM) degradation and cardiac fibrosis, is regulated by acetylation, and the broad-spectrum HDAC inhibitor Trichostatin A (TSA) and the class I HDAC inhibitor Mocetinostat (hereafter referred to as MGCD) each downregulate MMP9 expression in post-infarct myocardium.8
The proinflammatory cytokine interleukin (IL)-18 exerts both mitogenic and migratory effects on CF.9, 10, 11, 12 IL-18 is a potent inducer of MMP9,13 and this response is attenuated by mutations in NF-κB and AP-1 binding sites in its promoter region, demonstrating that MMP9 is an NF-κB and AP-1 responsive gene. Interestingly, NF-κB and AP-1 also induce Il18 transcription.14 However, whether HDAC inhibitors downregulate IL-18 and MMP9 expression in CF by blocking NF-κB and/or AP-1 binding to their regulatory elements has not been demonstrated.
Reversion-Inducing-Cysteine-Rich Protein with Kazal Motifs (RECK) is a membrane-anchored MMP regulator.15 It inhibits MMP9 activation and induction.15, 16 In many malignant cells, RECK expression is markedly downregulated,17 and restoring its expression inhibits their metastatic potential. Histone acetylation downregulates RECK expression, and HDAC inhibitors restore its expression in cancer cells by blocking Sp1 binding.18 We have previously reported that IL-18 suppresses RECK expression in CF by inducing Sp1 activation.12 Whether HDAC inhibitors regulate RECK expression in CF has not been investigated.
A sustained increase in systemic angiotensin (Ang)-II levels mediates chronic hypertension that eventually leads to cardiac hypertrophy and fibrosis. Further, blockade of angiotensin II type I receptor (AT1), or downregulation of AT1, has been shown to inhibit the activation of multiple pro-fibrotic pathways in heart and kidney.19, 20, 21 We have previously reported that chronic infusion of Ang-II induces IL-18 and MMP9 expression in hypertrophied mouse myocardium, but suppresses RECK expression.22 Analogous results were obtained in cultured CF.23 Such observations in vivo and in vitro prompted us to hypothesize that HDAC inhibitors will blunt Ang-II-induced NF-κB/AP-1 and Sp-1 binding to their cognate response elements, thereby suppressing IL-18 and MMP9, but restoring RECK expression.
Materials and methods
Materials
Human angiotensin II (Ang-II; #A9525), anti-β-actin (#A5441), fluorescein isothiocyanate (FITC)-conjugated monoclonal anti-β-actin (#F3022), smooth muscle actin antibodies (#F3777), antibodies against the MMP9 that detect both pro and active forms (#M9570), α-tubulin (T5168), Cell Death Detection ELISAPLUS kit (#11920685001), lentiviral shRNA against HDAC1 (TRC#TRCN0000229438) and HDAC2 (TRC#TRCN0000375947), and all other chemicals were purchased from Sigma-Aldrich (St Louis, MO, USA). Mocetinostat (MGCD0103, #S1122) was from Selleckchem (Houston, TX, USA). Anti-platelet-endothelial cell adhesion molecule-1 (PECAM-1 or CD-31; #10R-CD31jMSP) antibodies used in fibroblast characterization were purchased from Fitzgerald Industries International (Acton, MA, USA). Anti-vimentin (#sc-373717) antibodies used in fibroblast characterization, anti-caspase-3 (35 kDa, #sc-136219) antibodies and lentiviral GFP shRNA (#sc-45924-V) were from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA). IL-18 antibodies (#D043–3) were purchased from R&D Systems (Minneapolis, MN, USA). Antibodies against RECK (#3433), phospho-p65 (p-p65, Ser536; #3033), phospho-c-Jun (p-c-Jun, Ser73; #9261), HDAC antibody sampler kit (#9928), cleaved caspase-3 (#9661) and α-tubulin (#2144) were purchased from Cell Signaling Technology, Inc. (Beverly, MA, USA). Antibodies against collagen type Iα1 (ColIα1; #ab34170) and collagen type IIIα1 (ColIIIα1; #ab7778) were from Abcam (Cambridge, MA, USA). Anti-mouse fibronectin (FBN) antibodies (#CL54951AP) were from Cedarlane (Burlington, NC, USA). Chromatin Immunoprecipitation (ChIP) Assay Kit (#17-295) was from EMD Millipore, Inc (Billerica, MA, USA). TaqMan probes for MMP9 (Mm00442991_m1), IL-18 (Mm00434226_m1), RECK (Mm01299530_m1), and 18S (Hs03003631_g1), Restore Western blot Stripping Buffer (#21059), CyQUANT Cell Proliferation Assay (#C7026), and Corning BioCoat Matrigel Invasion Chambers with 8.0 μm PET Membrane (#11563570) were from ThermoFisher Scientific (Grand Island, NY, USA). Nuclear Extraction Kit (#AY2002) and mouse IL-18 ELISA kit (#BMS618/2) were from Affymetrix eBioscience (San Diego, CA, USA). Colorimetric HDAC assay kit (# 56210) was purchased from Active Motif (Carlsbad, CA, USA). Dual-Luciferase Reporter Assay System (#E1910) and CellTiter 96 Non-radioactive Cell Proliferation Assay kit (#G4000) were from Promega (Madison, WI, USA). Cell Death Detection ELISAPLUS kit (#11920685001) was from Roche Applied Science. MMP9 Biotrak Activity Assay kit (#RPN2634) was from GE Healthcare Biosciences (Piscataway, NJ, USA).
Isolation and culture of adult mouse cardiac fibroblasts
This investigation conforms to the Guide for the Care and Use of Laboratory Animals, published by the National Institutes of Health (DRR/National Institutes of Health, 1996), and all protocols were approved by the Institutional Animal Care and Use Committee of Tulane University (New Orleans, LA, USA). CF were isolated from normotensive adult male C57Bl/6 mice (∼3 m of age, ∼25 g; The Jackson Laboratory) as previously described,24 and used between passages 2–3. At 70% confluency, the cells were made quiescent by incubating in a conditioning medium (RPMI 1640 medium with 5 mM glucose, 0.5% BSA and antibiotics; pH 7.3) for 48 h. At the end of the experimental period, culture supernatants were collected and snap frozen. Cells were harvested, snap frozen and stored at –80 °C.
Lentiviral transduction
CF were trasduced with lentiviral HDAC1, HDAC2 or GFP shRNA (multiplicity of infection (moi) 0.5) for 48 h as described earlier.25 Transfection efficiency (Green Fluorescent Protein) was near 100%, and under the conditions used, the viral vectors had no significant effect on cell shape, adherence or viability (data not shown).
Fibroblast proliferation, migration and death
CF proliferation by CyQUANT assay, CF migration using BioCoat Matrigel invasion chambers and 8.0-μm pore polyethylene terephthalate membranes with a thin layer of Matrigel basement membrane matrix, and cell viability using the Cell Death Detection ELISAPLUS kit have all been previously described.26
Promoter-reporter analysis
A 726-bp fragment of the MMP9 gene promoter, constructs with mutations in NF-κB- and AP-1-binding sites, and cloning into the pGL3-Basic reporter vector have all been previously described13. A RECK proximal promoter reporter construct in pGL3-Basic vector, and constructs with mutations in one or both Sp1 binding sites have also been previously described 27. The inducible (−2505 to +61 nt and κB-less −438 to +61 nt) and basal (−540 to +61 nt) Il18 promoter-reporter constructs have also been described 14. CF were transiently transfected with reporter vectors (2 μg), with pRL-Renilla (100 ng) serving as an internal control. Twenty four hours later, cells were treated with Ang-II (10−7 M) for 24 h. Firefly and Renilla luciferase activities were analyzed using the Dual-Luciferase Reporter Assay System. The ratio of firefly to Renilla luciferase was determined, and the results expressed as fold change from untreated controls.
Chromatin immunoprecipitation assay
CF at 70% confluency were made quiescent by incubating in medium containing 0.5% BSA for 16 h, and then treated with Ang-II (10−7 M) for 1 h. Chromatin immunoprecipitation (ChIP) assays were carried out as described.14 Immune complexes were prepared using anti-p-p65, anti-p-c-Jun or anti-Sp1 antibodies. Normal IgG served as a control. Supernatants of immunoprecipitation reactions carried out without antibody were used as the total input DNA controls. PCR was carried out on 1 μl of a 1:100 dilution of each sample using the primers described below for MMP9 (NF-κB, 295nt, sense, 5′-AGTGGTAAGACATTTGCCCGA-3′ and antisense, 5′-TGCAACACCCCCTCCCAGGTCAG-3; AP-1, 227 nt, sense, 5′-TGGGGTCTTGCCTGACTTGGCA-3, and antisense, 5′-AGAGGTGTCTGACTGCAGCTG-3′), and followed by analysis on 2% agarose gels. Primers from the MMP9 open reading frame (ORF, 294 nt, sense, 5′-TGTGGAATCGGTCATGGGCAG-3′ and antisense, 5′-TGCCAGCACCAGCTCCTGGTT-3′) were used as PCR control. For RECK (both Sp1 sites included, 165nt), primers: sense, 5′-ATAACAAAGAGCCAGGGTCCA-3′ and antisense, 5′-TCGGACCCAGCCTGGCCGTAG-3′ were used. Primers from the RECK ORF (236nt, sense, 5′-AGTGTTTTCTCGAAAGCTCACAGT-3′ and antisense, 5′-AGCCAGACATGTCAGCATGGACAC-3′) were used as the PCR control. For the inducible Il18 promoter region containing the NF-κB binding site: sense, 5′-CTAGACATTCCTTGCTCTTCTTTGGTA-3′ and antisense, 5′-AGTATTTATAATTCATGCGTATCTAGT-3′ primers were used.
mRNA expression-real-time quantitative PCR
DNA-free total RNA was isolated using the RNAqueous-4 PCR kit (Ambion). mRNA levels were analyzed by RT-qPCR using TaqMan probes. 18S rRNA served as internal control. The results are expressed as fold increase from untreated after normalizing to 18S.
HDAC activity assays
Nuclear proteins were extracted using the Nuclear Extraction Kit from Affymetrix, and 100 μg of the extract was incubated overnight at 4 °C with protein A/G agarose complex and antibodies against HDAC1 or HDAC2. Immune complexes were centrifuged, washed three times and deacetylase activity measured using the colorimetric HDAC assay kit and absorbance at 405 nm. Deacetylase activity was measured in pmoles min−1 mg−1. Activity was normalized to the untreated controls, and the results expressed as fold change. Results are representative of six independent experiments.
Co-immunoprecipitation and immunoblotting
Co-immunoprecipitation and immunoblotting (Co-IP/IB) was performed as previously described.28 For IP, equal amounts of nuclear extracts were incubated overnight with HDAC1- or HDAC2-specific antibodies attached to agarose beads at 4 °C under slow rotation. After washing three times in buffer (50 mM Tris-Cl, 150 mM NaCl, 0.1% Nonidet P-40), the bound proteins were eluted by boiling the beads in SDS sample buffer for subsequent SDS-PAGE and immunoblotting.
Immunoblotting, ELISA, Biotrak activity assays
Preparation of whole cell homogenates, immunoblotting, detection by enhanced chemiluminescence (ECL Plus; GE Healthcare) and densitometry were described previously.11, 24, 25, 28 Although a representative immunoblot is shown in the figures, densitometric data from three independent experiments are shown whenever the results are less clear. Secreted IL-18 levels in culture supernatants were analyzed by ELISA according to manufacturer's instructions. MMP9 activity in concentrated culture supernatants containing 1 μg of total protein was analyzed using the MMP9 Biotrak Activity Assay kit.
Statistical analysis
All data are expressed as mean±s.e. Since the sample size was not equal in all studies. and comparisons were made between groups of 3 or 4 (untreated vs. Ang-II with and without inhibitors or solvent control), we performed analysis of variance followed by Tukey-Kramer post hoc test. Differences are considered significant if the P value is less than or equal to 0.05.
Results
Silencing HDAC1 or HDAC2 attenuates Ang-II-induced CF proliferation and migration
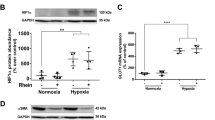
CF express both HDAC 1 and 2 (Figure 1a), and Ang-II enhanced their activation in a dose-dependent manner, with peak levels of activation detected at 10−7 M concentration (Figure 1b). Further, Ang-II at 10−7 M induced significant increases in both proliferation (Figure 1c) and migration (Figure 1d) of CF. These responses were attenuated by the knockdown of HDAC1 or HDAC2 (knockdown was confirmed by immunoblotting; Figure 1e). However, simultaneous knockdown of both HDACs resulted in cell death (Figure 1f). These results demonstrate that HDAC1 and HDAC2 play critical roles in the mitogenic and migratory effects of Ang-II in CF (Figure 1).
Silencing HDAC1 and HDAC2 inhibits Ang-II-induced cardiac fibroblast proliferation and migration. (a) Expression of HDAC1 and HDAC2 at basal conditions was analyzed by immunoblotting. CF1, CF2: two independent cultures of primary cardiac fibroblasts. Cell extracts from human epithelial cells (HeLa) and mouse embryonic fibroblasts (NIH3T3) served as positive controls (n=3). (b) Effect of Ang-II dose on activation of HDAC1 and HDAC2 in quiescent CF as analyzed by a colorimetric assay using nuclear protein extracts (100 μg) immunoprecipitated with HDAC1- or HDAC2-specific antibodies. Deacetylase activity was calculated in pmoles min−1 mg−1. Results are expressed as fold change from controls (n=6). (c) Silencing HDAC1 or HDAC2 attenuates Ang-II-induced CF proliferation. CF transduced with lentiviral HDAC1 or HDAC2 shRNA (moi 0.5 for 24) were treated with Ang-II (10−7 M) for 48 h, and proliferation analyzed by CyQUANT assay. (d) Silencing HDAC1 or HDAC2 inhibits Ang-II (10−7 M for 12 h) -induced CF migration. Migration was analyzed using BioCoat Matrigel invasion chambers and MTT assay. (e) Knockdown of HDAC1 and HDAC2 was confirmed by immunoblotting (n=3). Akt served as an off-target. (f) Silencing HDAC1 or HDAC2 failed to induce cell death. Forty-eight hours after lentiviral transduction, cell death was analyzed by an ELISA that quantifies mono and oligonucleosomal fragmented DNA in cytoplasmic extracts. (b, c, d, f) *P<at least 0.01 vs. untreated, †P<at least 0.05 vs. Ang-II (n=6-12).
TSA inhibits Ang-II-induced HDAC 1 and 2 activation in CF, and restores their association
In pilot experiments, we tested the efficacy of various doses of TSA (0, 100, 200, 400 and 800 nM) on HDAC1 activity. At 400 nM, TSA was highly effective in reducing Ang-II-mediated HDAC1 activity, but increasing its concentration to 800 nM induced cell death (data not shown). Therefore, in all subsequent experiments, TSA was used at 400 nM. TSA at this concentration inhibited Ang-II-induced activation of both HDAC1 and HDAC2 in CF (Figure 2a). Further, co-IP/IB demonstrated physical association between HDAC1/HDAC2 in unstimulated CF (Figure 2b, left and right panels, lane 1), and this interaction decreased following Ang-II treatment (Figure 2b, lane 2). Notably, TSA restored their interaction (Figure 2b, lane 3).
TSA reverses Ang-II-induced HDAC activity and restores HDAC1 and HDAC2 dimerization. (a) TSA inhibits Ang-II-induced HDAC1 and HDAC2 activity. Quiescent CF treated with TSA (400 nM for 24 h) and Ang-II (10−7 M for 24 h) were analyzed for HDAC1 or HDAC2 activity as described in Figure 1b (n=6). *P<0.01 vs. untreated, †P<at least 0.05 vs. Ang-II (n=12). (b) TSA restores HDAC1 and 2 dimerization. CF treated or not with TSA (400 nM for 24 h) and Ang-II (10−7 M for 24 h) were analyzed for HDAC1 and HDAC2 binding by co-immunoprecipitation and immunoblotting (n=3).
TSA differentially regulates Ang-II-induced MMP9, IL-18 and RECK expression by modulating NF-κB, AP-1 or Sp1 binding to their regulatory regions
Ang-II significantly increased MMP9 promoter-dependent reporter gene activity, and this effect was reduced by mutation of the NF-κB or AP-1 binding site (Figure 3a). Further, ChIP analysis using p-p65 and p-c-Jun antibodies, and primer pairs that separately amplify the regions containing the NF-κB and AP-1 binding sites, revealed low levels of amplified DNA in the control unstimulated CF (Figure 3b—upper panels), whereas increased levels were found after Ang-II treatment (Figure 3b—middle panels). TSA markedly inhibited this response (Figure 3b—bottom panels). Consistently, TSA also inhibited Ang-II-induced MMP9 mRNA expression (Figure 3c), protein levels (Figure 3d—upper panel), secretion and activity (Figure 3d—lower panel).
TSA reverses Ang-II-induced MMP9 expression and RECK suppression by targeting their transcriptional regulation. (a) Ang-II-induced MMP9 promoter-dependent reporter gene activation is mediated in part via NF-κB and AP-1. CF transfected with wild type and mutant MMP9 promoter reporter constructs for 24 h were incubated with Ang-II (10−7 M) for 12 h. pRL-TK vector was used as transfection control. (b) TSA inhibits NF-κB and AP-1 binding to MMP9 promoter region. Quiescent CF were treated with TSA (400 nM for 24 h) before Ang-II (10−7 M) addition for 1 h and ChIP analysis carried out. Amplification of the MMP9 gene region containing NF-κB (left hand panel) or AP-1 (right hand panel) binding sites is shown. No specific DNA was amplified with control IgG (lane 1), but amplification was observed with anti-p65 or c-Jun antibody (lane 3). Amplification of input DNA is shown in the middle panel (n=3). (c, d) TSA (400 nM) suppresses Ang-II-induced MMP9 mRNA (1 h; RT-qPCR; c) and protein expression (2 h; immunoblotting; d, n=3) and secretion (d, lower panel, n=6). (e) Ang-II suppresses RECK promoter-dependent reporter gene activation in part via Sp1. CF transfected with wild type and mutant RECK promoter reporter constructs for 24 h were incubated with Ang-II (10−7 M) for 12 h. (f) TSA inhibits Sp1 binding to RECK promoter region. Quiescent CF were treated with TSA (400 nM for 24 h) prior to Ang-II (10−7 M) addition for 1 h. The ChIP analysis was carried out as in b. Amplification of the RECK gene region containing both Sp1 binding sites is shown (n=3). (g, h) TSA suppresses RECK mRNA (g) and protein (h) expression. Quiescent CF were incubated with TSA (400 nM) and Ang-II (10−7 M) for 6 h. RECK mRNA expression was analyzed by RT-qPCR and its protein levels by immunoblotting (n=3). (a, c, e, g) *P<at least 0.01, †P<at least 0.05 (n=12).
RECK is a MMP regulator, and contains two Sp1 binding sites in its proximal promoter region.15, 27 Although Ang-II suppressed RECK promoter-dependent reporter gene activation, mutation in either of the two Sp1 sites enhanced its activity (Figure 3e). Mutating both sites further enhanced this induction, demonstrating that Sp1 appears to mediate the inhibitory effects of Ang II on RECK gene transcription. ChIP analysis using anti-Sp1 antibodies, and primer pairs that amplify the region containing both Sp1 binding sites, revealed low levels of amplified DNA in the control unstimulated CF (Figure 3f—upper panel), whereas increased levels were found following Ang-II treatment (Figure 3f—middle panel). TSA not only inhibited Ang-II-induced Sp1 binding to RECK promoter region (Figure 3f—lower panel), but also reversed Ang-II-induced suppression of RECK mRNA expression (Figure 3g) and protein levels (Figure 3h).
Our results also show that Ang-II increased activation of both inducible (I) and basal (B) Il18 promoter regions in the CF (Figure 4a), and deletion of κB-binding sites in either region reduced this activity. However, the stimulatory effects of Ang-II appeared to be more pronounced on the inducible form. Moreover, the ChIP analysis revealed increased p65 binding to the inducible Il18 promoter region, and TSA inhibited this effect (Figure 4b). Further, TSA inhibited Ang-II-induced IL-18 mRNA expression (Figure 4c), protein levels (Figure 4d) and secretion (Figure 4e), indicating that TSA exerts anti-fibrotic effects in CF, that is, it inhibits the pro-fibrotic MMP9 and IL-18 expression, but restores the anti-fibrotic RECK (Figures 3 and 4).
TSA blunts Ang-II-induced IL-18 expression by suppressing NF-κB binding to its promoter regions. (a) Ang-II induces Il18 promoter-dependent reporter gene activation in part via NF-κB. CF were transfected with full length or deletion constructs lacking the NF-κB binding sites in inducible (I) or basal (B) promoter regions together with pRL-TK, and then treated with Ang-II (10−7 M) for 12 h. Firefly and Renilla luciferase activities were determined after 24 h of incubation. (b) TSA suppresses NF-κB binding to inducible Il18 promoter region. Quiescent CF were treated or not with TSA (400 nM) and Ang-II (10−7 M) for 1 h, and ChIP assay carried out with anti-p65 antibodies prior to amplification of the Il18 promoter region containing the NF-κB site. No specific DNA was seen in the chromatin immunoprecipitated with control IgG (lane 1). Specific DNA bands obtained with anti-p65 antibody are shown in lanes 3. Amplification of the input DNA is shown in the middle panel (n=3). (c, d, e) TSA suppresses IL-18 MMP9 mRNA expression (c), protein levels (d) and secretion (e). Quiescent CF incubated with TSA (400 nM) and Ang-II (10−7 M) for 1 (mRNA), 2 (protein), or 24 h (secretion) were analyzed by RT-qPCR, immunoblotting (data from three independent experiments is summarized in the lower panel), and ELISA (secreted levels in equal amounts of culture supernatants). (a, c, d, e) *P<at least 0.01, †P<at least 0.05 (n=12).
TSA suppresses Ang-II- induced ECM expression, and CF proliferation and migration
TSA inhibited not only Ang-II-induced ColIα1, ColIIIα1 and FBN expression (Figure 5a), but also CF proliferation (Figure 5b) and migration (Figure 5c). Importantly, TSA exerted these anti-fibrotic effects without affecting cell viability, as evidenced by the low levels of mono- and oligonucleosomal fragmented DNA in cytoplasmic extracts (Figure 5d—left panel) and low levels of active caspase-3 (Figure 5d, right panel). These results suggest the anti-fibrotic potential of HDAC inhibitors in hypertensive heart disease (HHD) (Figure 5).
TSA inhibits ECM production, and CF proliferation and migration. (a) TSA (400 nM for 24 h) inhibits Ang-II (10−7 M for 6 h)-induced ColIα1, ColIIIα1 and fibronectin (FBN) expression in CF as analyzed by immunoblotting. Densitometric analysis from three independent experiments is summarized on the right. (b) TSA inhibits Ang-II-induced CF proliferation as analyzed by the CyQUANT assay. (c) TSA inhibits Ang-II-induced CF migration as analyzed using BioCoat Matrigel invasion chambers and MTT assay. (d) TSA fails to induce CF death or activation of caspase-3. H2O2 (100 μM for 12 h) served as a positive control. Cell death was analyzed as in Figures 1a. (b, c) *P<0.001 vs. untreated, †P<at least 0.01 vs. Ang-II (n=12). D, *P<0.001 vs. untreated or TSA (n=12).
MGCD (Mocetinostat) inhibits cardiac fibroblast proliferation and migration
MGCD is a class I HDAC inhibitor. In pilot experiments, we tested the efficacy of various doses of MGCD (0, 0.01, 0.1, 1 and 10 μM) on HDAC1 activity. At 1 μM concentration, MGCD effectively reduced Ang-II-induced HDAC1 activity, but increasing its concentration to 10 μM induced cell death (data not shown). Therefore, in all subsequent experiments, MGCD was used at 1 μM. Similar to TSA, MGCD not only inhibited Ang-II-induced activation of HDAC 1 and 2 (Figure 6a), it also restored their association (Figure 6b). Further, MGCD inhibited Ang-II-induced MMP9, IL-18 and ECM expression (Figure 6c), and similar to TSA, reversed RECK suppression (Figure 6c). MGCD also attenuated Ang-II-induced CF proliferation (Figure 6d) and migration (Figure 6e), without compromising cell viability (data not shown). These results support a therapeutic potential for HDAC inhibitors in cardiac fibrosis (Figure 6).
Mocetinostat (MGCD) attenuates Ang-II-induced cardiac fibroblast proliferation and migration. (a) MGCD inhibits Ang-II-induced increases in HDAC1 and HDAC2 enzyme activities. Activation was analyzed as in Figure 1b (n=3). (b) MGCD inhibits HDAC1/HDAC2 dimerization. Quiescent CF treated as in A were analyzed for HDAC1/2 domerization by IP/IB (n=3). (c) MGCD reverses Ang-II-mediated MMP9, IL-18, ColIα1, ColIIIα1, and FBN expression, and RECK suppression. CF treated with MGCD (1 μM in DMSO for 24 h) before Ang-II addition for up to 6 h were analyzed by immunoblotting using cleared whole cell homogenates. Densitometric analysis from three independent experiments is summarized on the right. (d) MGCD inhibits Ang-II (10−7 M for 48 h)-induced CF proliferation as quantified by the CyQUANT assay. (e) MGCD inhibits Ang-II-induced CF migration as analyzed using BioCoat Matrigel invasion chambers and MTT assay. (a, c, d, e) *P< at least 0.01 vs. untreated, †P<at least 0.01 vs. Ang-II±DMSO (n=12).
Discussion
HDACs play a key role in the epigenetic regulation of multiple genes involved in cardiac fibrosis and adverse remodeling.2, 3, 4, 5, 6, 7 A sustained increase in systemic Ang-II levels contributes to progressive cardiac fibrosis, adverse remodeling and contractile dysfunction. TSA is a broad-spectrum HDAC inhibitor. MGCD specifically targets class I HDACs. Here we show that both TSA and MGCD attenuate Ang-II-induced increases in HDAC1 and HDAC2 activity in cultured CF. Further, association between HDAC1 and HDAC2 decreases during mitosis.29 Our results show that while Ang-II inhibits HDAC1/HDAC2 interaction, both TSA and MGCD reverse this effect (Figure 2b). Moreover, these HDAC inhibitors while inhibiting pro-fibrotic MMP9 and IL-18 expression (Figures 3c and d; 4c and d), restore anti-fibrotic RECK levels (Figure 3g and h). TSA achieves these effects by modulating their transcription. TSA inhibits Ang-II-mediated transcriptional upregulation of MMP9 and Il18 by blocking NF-κB and/or AP-1 binding to their 5′-cis regulatory regions (Figures 3b, 4b). TSA reverses Ang-II-induced RECK suppression by blocking Sp1 binding to its proximal promoter region (Figure 3f). Importantly, both TSA and MGCD inhibit Ang-II-induced ECM production, and CF proliferation and migration (Figures 5 and 6). These results demonstrate the anti-fibrotic effects of HDAC inhibitors, and suggest their therapeutic potential in HHD.
HHD is characterized by sustained expression and activation of various MMPs. CF express multiple MMPs, including MMPs 2, 9 and 14, and MMP14 and TIMP2 play a role in MMP2 maturation. While MMPs 2 and 9 are gelatinases, MMP14 is a transmembrane type MMP, and their persistent activation contributes to cardiac fibrosis and adverse remodeling. Here we demonstrate that TSA inhibits MMP9 expression by blocking NF-κB (p65) and AP-1 (c-Jun) binding to its promoter region. However, it appears that the inhibitory effects of TSA on MMP9 expression are cell type-dependent. For example, in HeLa cells, the MMP9 promoter region appears to be occupied by HDAC1 and 3 at basal conditions, and treatment with TSA upregulates its expression by removing both the HDACs.30 Similarly, TSA inhibits MMP2 expression in NIH3T3 fibroblasts, but not in the fibrosarcoma cell line HT1080.31 TSA also fails to affect MMP14 and TIMP2 expression in these cells. In contrast, HDAC inhibitors attenuate MMP1 expression,32 a collagenase also expressed in human CF that plays a role in their migration.33 Thus, it appears that the inhibitory effects of HDAC inhibitors on MMPs are stimulus-specific and cell type-dependent. However, in CF, both TSA and MGCD exert anti-fibrotic effects and inhibit MMP9 expression and activation.
Inflammation plays a critical role in HHD. IL-18 is a proinflammatory cytokine, and chronic Ang-II infusion induces its sustained expression in hypertrophied myocardium.22 It also exerts mitogenic and migratory effects on isolated CF,9 and Ang-II positively regulates its expression in CF. Importantly, both TSA and MGCD inhibited IL-18 expression in CF, demonstrating that HDAC inhibitors also exert anti-inflammatory effects. Interestingly, HDAC inhibitors have also been shown to block IL-18 signaling. For example, both TSA and CBHA (m-Carboxycinnamic acid bis-hydroxamide), a HDAC1/HDAC3 inhibitor, attenuate IL-18-induced cardiomyocyte hypertrophy both in vivo and in vitro.34, 35 In contrast, in a myeloid leukemia cell line, HDAC inhibitors increased IL-18 expression.36 In that study, TSA induced IL-18 expression by inducing activation of full length and a 1357 bp Il18 gene promoter. However, Valproate, a class I HDAC inhibitor and an FDA approved drug, failed to affect Il18 promoter activity in these cells,36 suggesting that effects of HDAC inhibitors on IL-18 expression are cell type-specific. However, in heart, IL-18 amplifies inflammatory signaling and induces hypertrophy, fibrosis and dysfunction. In vitro, it induces CF activation, proliferation and migration. Since both TSA and MGCD suppress IL-18 expression and its downstream signaling, HDAC inhibitors may have a therapeutic potential in inflammatory cardiac diseases, including HHD.
In contrast to its stimulatory effects on MMP9 and IL-18, Ang-II suppresses RECK expression in CF via Sp1 activation. Both TSA and MGCD reversed Ang-II-induced RECK suppression. TSA attenuated Sp1 binding to RECK proximal promoter region, and restored its expression. Consistent with our results, the role of Sp1 in RECK downregulation and its reversal by HDAC inhibitors have been previously reported in cancer cells.18, 37 Thus it is possible that HDAC inhibitors exert anti-fibrotic effects by suppressing pro-fibrotic MMP9 and IL-18, and restoring the anti-fibrotic RECK expression in CF.
RECK exerts multiple anti-fibrotic effects. In addition to targeting MMPs, it also blocks expression and/or signaling of other pro-fibrotic factors. For example, IL-6 is a potent inducer of cardiomyocyte hypertrophy and CF proliferation,38 and Ang-II enhances its secretion by CF.38 Since RECK has been shown to bind the ligand binding IL-6R and gp130, the signal transducing subunit of the IL-6 receptor heterodimer,39 it may interfere with IL-6 signaling by blocking IL-6 interaction with the IL-6R/gp130 heterodimer. RECK also blocks Epidermal Growth Factor Receptor transactivation,40 which is known to contribute to CF proliferation.41 Thus, it is possible that HDAC inhibitors can blunt cardiac fibrosis and adverse remodeling through two different mechanisms: that is, by directly targeting MMP9 and IL-18 induction, and indirectly by restoring RECK expression.
In summary, we have demonstrated that Ang-II exerts pro-inflammatory and pro-fibrotic effects in primary cardiac fibroblasts. Using two independent approaches-gene silencing and pharmacological inhibition (Trichostatin A and Mocetinostat), we further demonstrated that targeting HDACs reverses Ang-II induced (i) IL-18 and MMP9 induction, (ii) RECK suppression and (iii) CF proliferation and migration. These novel results suggest a therapeutic potential for HDAC inhibitors in cardiac fibrosis and adverse remodeling in inflammatory cardiac diseases, including HHD.
References
Montgomery RL, Davis CA, Potthoff MJ, Haberland M, Fielitz J, Qi X, Hill JA, Richardson JA, Olson EN . Histone deacetylases 1 and 2 redundantly regulate cardiac morphogenesis, growth, and contractility. Genes Dev 2007; 21: 1790–1802.
Williams SM, Golden-Mason L, Ferguson BS, Schuetze KB, Cavasin MA, Demos-Davies K, Yeager ME, Stenmark KR, McKinsey TA . Class I HDACs regulate angiotensin II-dependent cardiac fibrosis via fibroblasts and circulating fibrocytes. J Mol Cell Cardiol 2014; 67: 112–125.
Pang M, Zhuang S . Histone deacetylase: a potential therapeutic target for fibrotic disorders. J Pharmacol Exp Ther 2010; 335: 266–272.
Kang SH, Seok YM, Song MJ, Lee HA, Kurz T, Kim I . Histone deacetylase inhibition attenuates cardiac hypertrophy and fibrosis through acetylation of mineralocorticoid receptor in spontaneously hypertensive rats. Mol Pharmacol 2015; 87: 782–791.
Schuetze KB, McKinsey TA, Long CS . Targeting cardiac fibroblasts to treat fibrosis of the heart: focus on HDACs. J Mol Cell Cardiol 2014; 70: 100–107.
Xie M, Hill JA . HDAC-dependent ventricular remodeling. Trends Cardiovasc Med 2013; 23: 229–235.
McKinsey TA . Targeting inflammation in heart failure with histone deacetylase inhibitors. Mol Med 2011; 17: 434–441.
Mani SK, Kern CB, Kimbrough D, Addy B, Kasiganesan H, Rivers WT, Patel RK, Chou JC, Spinale FG, Mukherjee R, Menick DR . Inhibition of class I histone deacetylase activity represses matrix metalloproteinase-2 and -9 expression and preserves LV function postmyocardial infarction. Am J Physiol Heart Circ Physiol 2015; 308: H1391–H1401.
Fix C, Bingham K, Carver W . Effects of interleukin-18 on cardiac fibroblast function and gene expression. Cytokine 2011; 53: 19–28.
Yu Q, Vazquez R, Khojeini EV, Patel C, Venkataramani R, Larson DF . IL-18 induction of osteopontin mediates cardiac fibrosis and diastolic dysfunction in mice. Am J Physiol Heart Circ Physiol 2009; 297: H76–H85.
Valente AJ, Sakamuri SS, Siddesha JM, Yoshida T, Gardner JD, Prabhu R, Siebenlist U, Chandrasekar B . TRAF3IP2 mediates interleukin-18-induced cardiac fibroblast migration and differentiation. Cell Signal 2013; 25: 2176–2184.
Siddesha JM, Valente AJ, Sakamuri SS, Gardner JD, Delafontaine P, Noda M, Chandrasekar B . Acetylsalicylic acid inhibits IL-18-induced cardiac fibroblast migration through the induction of RECK. J Cell Physiol 2014; 229: 845–855.
Chandrasekar B, Mummidi S, Mahimainathan L, Patel DN, Bailey SR, Imam SZ, Greene WC, Valente AJ . Interleukin-18-induced human coronary artery smooth muscle cell migration is dependent on NF-kappaB- and AP-1-mediated matrix metalloproteinase-9 expression and is inhibited by atorvastatin. J Biol Chem 2006; 281: 15099–15109.
Chandrasekar B, Marelli-Berg FM, Tone M, Bysani S, Prabhu SD, Murray DR . Beta-adrenergic stimulation induces interleukin-18 expression via beta2-AR, PI3K, Akt, IKK, and NF-kappaB. Biochem Biophys Res Commun 2004; 319: 304–311.
Takahashi C, Sheng Z, Horan TP, Kitayama H, Maki M, Hitomi K, Kitaura Y, Takai S, Sasahara RM, Horimoto A, Ikawa Y, Ratzkin BJ, Arakawa T . Regulation of matrix metalloproteinase-9 and inhibition of tumor invasion by the membrane-anchored glycoprotein RECK. Proc Natl Acad Sci USA 1998; 95: 13221–13226.
Takagi S, Simizu S, Osada H . RECK negatively regulates matrix metalloproteinase-9 transcription. Cancer Res 2009; 69: 1502–1508.
Noda M, Takahashi C . Recklessness as a hallmark of aggressive cancer. Cancer Sci 2007; 98: 1659–1665.
Hsu MC, Chang HC, Hung WC . HER-2/neu represses the metastasis suppressor RECK via ERK and Sp transcription factors to promote cell invasion. J Biol Chem 2006; 281: 4718–4725.
Mikami D, Kimura H, Kamiyama K, Torii K, Kasuno K, Takahashi N, Yoshida H, Iwano M . Telmisartan activates endogenous peroxisome proliferator-activated receptor-delta and may have anti-fibrotic effects in human mesangial cells. Hypertens Res 2014; 37: 422–431.
Zhang Y, Shao L, Ma A, Guan G, Wang J, Wang Y, Tian G . Telmisartan delays myocardial fibrosis in rats with hypertensive left ventricular hypertrophy by TGF-beta1/Smad signal pathway. Hypertens Res 2014; 37: 43–49.
Yu C, Chen J, Guan W, Han Y, Wang WE, Wang X, Wang H, Jose PA, Zeng C . Activation of the D4 dopamine receptor attenuates proliferation and migration of vascular smooth muscle cells through downregulation of AT1a receptor expression. Hypertens Res 2015; 38: 588–596.
Siddesha JM, Valente AJ, Sakamuri SS, Yoshida T, Gardner JD, Somanna N, Takahashi C, Noda M, Chandrasekar B . Angiotensin II stimulates cardiac fibroblast migration via the differential regulation of matrixins and RECK. J Mol Cell Cardiol 2013; 65: 9–18.
Siddesha JM, Valente AJ, Yoshida T, Sakamuri SS, Delafontaine P, Iba H, Noda M, Chandrasekar B . Docosahexaenoic acid reverses angiotensin II-induced RECK suppression and cardiac fibroblast migration. Cell Signal 2014; 26: 933–941.
Valente AJ, Yoshida T, Gardner JD, Somanna N, Delafontaine P, Chandrasekar B . Interleukin-17A stimulates cardiac fibroblast proliferation and migration via negative regulation of the dual-specificity phosphatase MKP-1/DUSP-1. Cell Signal 2012; 24: 560–568.
Valente AJ, Clark RA, Siddesha JM, Siebenlist U, Chandrasekar B . CIKS (Act1 or TRAF3IP2) mediates Angiotensin-II-induced Interleukin-18 expression, and Nox2-dependent cardiomyocyte hypertrophy. J Mol Cell Cardiol 2012; 53: 113–124.
Somanna NK, Valente AJ, Krenz M, Fay WP, Delafontaine P, Chandrasekar B . The Nox1/4 Dual Inhibitor GKT137831 or Nox4 Knockdown Inhibits Angiotensin-II-Induced Adult Mouse Cardiac Fibroblast Proliferation and Migration. AT1 Physically Associates With Nox4. J Cell Physiol 2015; 231: 1130–1141.
Sasahara RM, Takahashi C, Noda M . Involvement of the Sp1 site in ras-mediated downregulation of the RECK metastasis suppressor gene. Biochem Biophys Res Commun 1999; 264: 668–675.
Valente AJ, Yoshida T, Izadpanah R, Delafontaine P, Siebenlist U, Chandrasekar B . Interleukin-18 enhances IL-18R/Nox1 binding, and mediates TRAF3IP2-dependent smooth muscle cell migration. Inhibition by simvastatin. Cell Signal 2013; 25: 1447–1456.
Khan DH, He S, Yu J, Winter S, Cao W, Seiser C, Davie JR . Protein kinase CK2 regulates the dimerization of histone deacetylase 1 (HDAC1) and HDAC2 during mitosis. J Biol Chem 2013; 288: 16518–16528.
Ma Z, Shah RC, Chang MJ, Benveniste EN . Coordination of cell signaling, chromatin remodeling, histone modifications, and regulator recruitment in human matrix metalloproteinase 9 gene transcription. Mol Cell Biol 2004; 24: 5496–5509.
Ailenberg M, Silverman M . Differential effects of trichostatin A on gelatinase A expression in 3T3 fibroblasts and HT-1080 fibrosarcoma cells: implications for use of TSA in cancer therapy. Biochem Biophys Res Commun 2003; 302: 181–185.
Kaneko F, Saito H, Saito Y, Wakabayashi K, Nakamoto N, Tada S, Suzuki H, Tsunematsu S, Kumagai N, Ishii H . Down-regulation of matrix-invasive potential of human liver cancer cells by type I interferon and a histone deacetylase inhibitor sodium butyrate. Int J Oncol 2004; 24: 837–845.
Cortez DM, Feldman MD, Mummidi S, Valente AJ, Steffensen B, Vincenti M, Barnes JL, Chandrasekar B . IL-17 stimulates MMP-1 expression in primary human cardiac fibroblasts via p38 MAPK- and ERK1/2-dependent C/EBP-beta, NF-kappaB, and AP-1 activation. Am J Physiol Heart Circ Physiol 2007; 293: H3356–H3365.
Majumdar G, Johnson IM, Kale S, Raghow R . Epigenetic regulation of cardiac muscle-specific genes in H9c2 cells by Interleukin-18 and histone deacetylase inhibitor m-carboxycinnamic acid bis-hydroxamide. Mol Cell Biochem 2008; 312: 47–60.
Majumdar G, Rooney RJ, Johnson IM, Raghow R . Panhistone deacetylase inhibitors inhibit proinflammatory signaling pathways to ameliorate interleukin-18-induced cardiac hypertrophy. Physiol Genomics 2011; 43: 1319–1333.
Koyama N, Koschmieder S, Tyagi S, Nürnberger H, Wagner S, Böcker U, Hoelzer D, Gerhard Ottmann O, Kalina U . Differential effects of histone deacetylase inhibitors on interleukin-18 gene expression in myeloid cells. Biochem Biophys Res Commun 2002; 292: 937–943.
Chang HC, Liu LT, Hung WC . Involvement of histone deacetylation in ras-induced down-regulation of the metastasis suppressor RECK. Cell Signal 2004; 16: 675–679.
Fredj S, Bescond J, Louault C, Delwail A, Lecron JC, Potreau D . Role of interleukin-6 in cardiomyocyte/cardiac fibroblast interactions during myocyte hypertrophy and fibroblast proliferation. J Cell Physiol 2005; 204: 428–436.
Walsh LA, Roy DM, Reyngold M, Giri D, Snyder A, Turcan S, Badwe CR, Lyman J, Bromberg J, King TA, Chan TA . RECK controls breast cancer metastasis by modulating a convergent, STAT3-dependent neoangiogenic switch. Oncogene 2015; 34: 2189–2203.
Kitajima S, Miki T, Takegami Y, Kido Y, Noda M, Hara E, Shamma A, Takahashi C . Reversion-inducing cysteine-rich protein with Kazal motifs interferes with epidermal growth factor receptor signaling. Oncogene 2011; 30: 737–750.
Murasawa S, Mori Y, Nozawa Y, Gotoh N, Shibuya M, Masaki H, Maruyama K, Tsutsumi Y, Moriguchi Y, Shibazaki Y, Tanaka Y, Iwasaka T, Inada M, Matsubara H . Angiotensin II type 1 receptor-induced extracellular signal-regulated protein kinase activation is mediated by Ca2+/calmodulin-dependent transactivation of epidermal growth factor receptor. Circ Res 1998; 82: 1338–1348.
Acknowledgements
BC is a recipient of the Department of Veterans Affairs Research Career Scientist award, and is supported by the US Department of Veterans Affairs, Office of Research and Development-Biomedical Laboratory Research and Development (ORD-BLRD) Service Award VA-I01-BX002255. The contents of this report do not represent the views of the Department of Veterans Affairs or the US government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Somanna, N., Valente, A., Krenz, M. et al. Histone deacetyltransferase inhibitors Trichostatin A and Mocetinostat differentially regulate MMP9, IL-18 and RECK expression, and attenuate Angiotensin II-induced cardiac fibroblast migration and proliferation. Hypertens Res 39, 709–716 (2016). https://doi.org/10.1038/hr.2016.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.54
Keywords
This article is cited by
-
Lysine acetyltransferases and lysine deacetylases as targets for cardiovascular disease
Nature Reviews Cardiology (2020)
-
Glycemic control by the SGLT2 inhibitor empagliflozin decreases aortic stiffness, renal resistivity index and kidney injury
Cardiovascular Diabetology (2018)
-
Modulation of cardiac stem cell characteristics by metoprolol in hypertensive heart disease
Hypertension Research (2018)
-
Organ memory: a key principle for understanding the pathophysiology of hypertension and other non-communicable diseases
Hypertension Research (2018)