Abstract
High blood viscosity is associated with increased peripheral resistance and high blood pressure (BP). Prehypertension refers to a systemic BP of 120–139 mm Hg systolic (SBP) and/or 80–89 mm Hg diastolic (DBP). Subjects with prehypertension have an increased risk of overt hypertension and incident cardiovascular disease compared with subjects who have optimal BP. In the present study, we investigated the hemorheological profiles of subjects with prehypertension. A total of 418 apparently healthy subjects were enrolled. BP, plasma lipids and glucose were measured using routine methods. Blood and plasma viscosity were measured using a cone-plate viscometer. The participants were grouped according to BP into the following categories: ‘normotensive’ (n=100), ‘prehypertensive’ (n=172), and ‘hypertensive’ (n=146). The blood viscosity, plasma viscosity and hematocrit of the prehypertensive subjects were higher than those of the normotensive subjects (P<0.01), but they were comparable to those of the hypertensive subjects. In simple correlation analyses, SBP and DBP were directly and significantly correlated with age, body mass index (BMI), blood glucose, hematocrit, plasma viscosity and blood viscosity. In multiple regression analyses, age, fasting blood glucose and plasma viscosity were independently related with SBP, whereas blood viscosity, fasting blood glucose and BMI significantly predicted DBP. These data demonstrate that BP in the range of so-called prehypertension is accompanied by important hemorheological changes, which are similar to those observed in people with overt hypertension. These results could explain the increased cardiovascular risk observed in these subjects as well as their susceptibility to hypertension.
Similar content being viewed by others
Introduction
Viscosity is a physical property of fluids, such as blood and plasma, and represents intrinsic resistance opposed to flow.1 Blood viscosity alterations have been associated with a number of cardiovascular disorders.2, 3, 4 In particular, hyperviscosity has been associated with increased peripheral resistances and hypertension.5
Hypertension is one of the most important challenges for public health because hypertensive subjects show an increased risk of cardiovascular disease, stroke and renal failure.6, 7 Current guidelines define hypertension as systolic blood pressure (SBP)/diastolic blood pressure (DBP) ⩾140/90 mm Hg.8 Interestingly, observational studies and meta-analyses suggest that individuals with blood pressure (BP) within a normal range and >120/80 mm Hg have an increased risk of cardiovascular disease and incident hypertension.9, 10, 11 The Seventh Report of the Joint National Committee on Prevention, Diagnosis, Evaluation and Treatment of High BP (JNC7) introduced the term ‘prehypertension’ for subjects with BP values ranging from 120 to 139 mm Hg systolic and/or from 80 to 89 mm Hg diastolic, whereas a BP level <120/80 mm Hg was defined ‘optimal’.12 Currently, no pharmacological treatment is recommended for prehypertension in the absence of comorbidity; however, studies have highlighted the importance of lifestyle changes to prevent progression to hypertension.12, 13 The JNC8 did not specifically address prehypertension, but in recent years, many clinical investigations and meta-analyses exploring this important topic have highlighted the potential implications of this condition for the risk of cardiovascular events.14, 15, 16, 17, 18
Based on this evidence, in the present study, we aimed to investigate the hemorheological profiles of subjects with prehypertension.
Materials and methods
Subjects and study design
The subjects were adult participants (age >18 years) in a primary prevention cardiovascular screening. For the present study, the following exclusion criteria were applied: premenopausal females, cigarette smoking, diabetes, plasma triglycerides >4.52 mmol l−1, and pharmacological treatment (including either chronic treatment or drugs occasionally taken during the week before enrollment in the study). Pharmacological agents and/or physiological or pathological conditions listed as exclusion criteria can directly or indirectly interfere with viscosity values.19, 20, 21
Eligible participants who provided informed consent were recruited. The protocol was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee. A total of 418 participants were enrolled.
Clinical examination and anthropometric measurements
All subjects were examined in the morning in a room at 22 °C after having fasted overnight. Subjects underwent both a clinical examination and blood sample withdrawal. Well-trained personnel measured BP, height and weight by routine methods. A questionnaire was administered to evaluate smoking habits. Body mass index (BMI) was computed as weight (in kilograms) divided by height (in squared meters).
BP measurements and classification
BP measurements were performed according to current guidelines.22 Before measurement, the subjects remained at rest in a sitting position for 5 min in a quiet room. BP was then measured in both arms and the higher value was recorded.
Subjects with SBP<120 mm Hg and DBP<80 mm Hg were classified as normotensive. Prehypertension was defined as SBP ranging from 120 to 139 mm Hg and/or DBP ranging from 80 to 89 mm Hg. Hypertension was defined as SBP⩾140 mm Hg and/or DBP⩾90 mm Hg.
Laboratory measurements
Fasting blood lipids (total cholesterol, high-density lipoprotein cholesterol, triglycerides) and glucose were measured with commercially available kits. Subjects with plasma glucose ⩾7 mmol l−1 were recalled to repeat the blood glucose measurement, and if both values were ⩾7 mmol l−1, these subjects were classified as diabetics. Low-density lipoprotein cholesterol was calculated according to the Friedewald formula.
Hemorheological variable measurements
Blood and plasma viscosity were measured within 2 h of blood withdrawal; the blood specimen was mixed with heparin (35 IU ml−1). Viscosity measurements were performed at 37 °C with a cone-plate viscometer (Wells-Brookfield DV-III, Middleboro, MA, USA) equipped with a cp-40 spindle. Blood viscosity was recorded at different shear rates. In the present manuscript, data obtained at 225 s−1 were used for the analysis, but the results were similar when data collected at different shear rates was used. For plasma viscosity, the average of measurements collected at shear rates of 225 and 90 s−1 was calculated. The coefficient of variation for blood and plasma viscosity was <3%. Micro-hematocrit was measured without correction for plasma trapping. The coefficient of variation for micro-hematocrit was ~1%.
Statistical analyses
Statistical analyses were performed using PASW 18.0 (SPSS Inc., Chicago, IL, USA) for Windows. The normality of the distribution was assessed by Shapiro–Wilk test. All studied variables had normal distributions, except triglycerides, which were log-transformed before analysis. An analysis of variance and Kruskal–Wallis test were applied to compare means among groups. The Pearson or Spearman correlation coefficient was used, as appropriate, to test the correlation between continuous variables. Tukey's post-hoc test was used. Statistical significance was set at P<0.05.
Results
A total of 418 subjects were recruited; the mean age of participants was 52±8 years and 55% were male (n=230). Participants were grouped into three categories according to their BP values: ‘normotensive’ (n=100), ‘prehypertensive’ (n=172), and ‘hypertensive’ (n=146). The clinical, biochemical and anthropometric parameters are reported in Table 1. As shown, normotensive individuals had significantly lower blood glucose and triglyceride levels. No differences concerning the other parameters were observed.
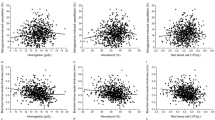
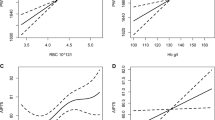
Hemorheological parameters are displayed in Figures 1,2,3. The blood viscosity, plasma viscosity and hematocrit of the prehypertensive subjects were higher than those of the normotensive subjects (P<0.01), but they were comparable to those of the hypertensive subjects.
All subjects were then grouped to evaluate possible correlations between SBP/DBP and clinical and hemorheological variables. The simple correlation analyses (Table 2) showed a direct and significant correlation between both SBP and DBP and age (r=0.19 for SBP; r=0.12 for DBP), BMI (r=0.11 for SBP; r=0.19 for DBP), fasting blood glucose (r=0.19 for SBP; r=0.21 for DBP), hematocrit (r=0.11 for SBP; r=0.17 for DBP), plasma viscosity (r=0.14 for SBP; r=0.10 for DBP) and blood viscosity (r=0.15 for SBP; r=0.23 for DBP). No correlation was found between BP and gender or blood lipids.
Variables that significantly correlated with BP in the simple correlation analysis were entered in a stepwise multiple regression analysis (Table 3). Age, fasting blood glucose and plasma viscosity were independently related with SBP, whereas blood viscosity, fasting blood glucose and BMI significantly predicted DBP.
Discussion
In this study, we investigated the hemorheological profiles of subjects with prehypertension. The main finding is that the subjects with prehypertension exhibited hematocrit, blood and plasma viscosity levels comparable to those of the hypertensive subjects and significantly higher than those of the normotensive subjects.
The term prehypertension was first introduced by Robinson and Brucer23 in 1939. In that study, the authors demonstrated that individuals with BP values ranging from 120 to 139 mm Hg systolic and/or from 80 to 89 mm Hg diastolic had an increased risk of developing overt hypertension. The prevalence of prehypertension varies depending on the type of population examined.17 Generally, the prevalence of prehypertension ranges from 25% to 50%, with black race showing a greater probability of a faster progression to hypertension.24
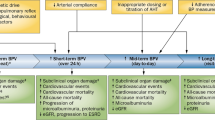
Furthermore, prehypertension is also associated with an increased risk of coronary heart disease (CHD), chronic kidney disease and type 2 diabetes.14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 In detail, individuals with prehypertension have an increased risk of stroke (relative risk (RR)=1.66) and chronic kidney disease (RR=1.59) compared with subjects having optimal BP. In a recent meta-analysis that included 17 studies, the association between prehypertension and CHD in Asian and Western populations was evaluated. Again, the RR of CHD was 1.43 in prehypertensive subjects compared with individuals with optimal BP. However, the risk of CHD was higher in Western than in Asian participants (RR=1.70 vs. 1.25, respectively). In addition, subjects with baseline prehypertension were at a higher risk of developing diabetes than normotensive subjects (RR=1.27) after 8 years of observation.25
The data of our study clearly show that the subjects with prehypertension exhibited hemorheological values similar to those of the hypertensive subjects and higher than those of the normotensive subjects. The relationship between blood viscosity and atherosclerosis is still much debated. Blood viscosity is an estimate of the force that opposes blood flow in blood vessels; it is strongly influenced by the number of RBCs, their deformability and the amount of plasma protein.26 Accordingly, any increase in blood viscosity may cause a reduction of blood flow. In addition, blood viscosity also contributes to wall shear stress, which is the tangential force that the blood exerts on vessel walls. Specifically, any increase in wall shear stress induces the release of nitric oxide (NO) and arterial vasodilation.27 The delicate balance between blood viscosity, shear stress and NO production ensures adequate blood flow to tissues. However, an undue and sustained increase in blood viscosity, as well as an inability of the endothelium to produce a sufficient amount of NO, can cause an increase in peripheral resistance. Peripheral resistance is a measure of the degree of resistance to blood flow within the vessels, and it is affected by factors, such as blood viscosity and vessel diameter and length.28, 29 Increases in blood viscosity or reductions in vessel diameter lead to a greater degree of friction between the flowing blood and the vessel wall; consequently, peripheral resistance increases. To guarantee adequate tissue perfusion, there is an increase in systemic BP to overcome this friction for flow progression.28 Conversely, low blood viscosity might affect vascular tone by reducing the amount of shear stress on the arterial wall.30
Therefore, low blood viscosity could have negative consequences by reducing the amount of shear stress and high blood viscosity could have negative consequences through increasing peripheral resistance.
The relationship between blood viscosity and BP has been investigated in previous studies with different results.31, 32, 33, 34, 35 In a recent paper, Gori et al.32 found a linear and positive correlation between BP and blood viscosity in a large German population. Jae et al.33 demonstrated that hematocrit, even within the normal range, predicted the incidence of hypertension after a 5-year follow-up. However, in other studies, a U-shaped relationship between blood viscosity and BP has been described, thus demonstrating that not only higher values but also lower values of viscosity and hematocrit have negative effects on vascular physiology.34, 35 To date, a physiological range for blood viscosity has not been established.
Our findings suggest that a small increase in blood viscosity, by ~5% over the values found in subjects with optimal BP, is associated with increased BP and might, at least in part, contribute to the excess incidence of cardiovascular events in these subjects.
There can be many reasons for an increase in blood viscosity, including aging, lipid profile, cigarette smoking and inflammatory diseases, among others.19, 20, 21, 36 Some of these conditions can be reasonably excluded as the cause of our findings, such as cigarette smoking (all participants were nonsmokers) and chronic inflammatory diseases (none of the participants were taking medication). For other variables, there were no statistically significant differences among the three groups. However, the individuals with prehypertension were slightly older and had slightly higher values of blood glucose, low-density lipoprotein cholesterol, triglycerides and BMI compared with the individuals with optimal BP. Taken together, these different factors may be responsible for higher blood viscosity and consequently for higher BP.37
It must be emphasized that high blood viscosity might have further negative effects on the cardiovascular system because the heart is overloaded pumping blood in the vascular bed.
The choice of a threshold value for continuous variables, such as BP, is always very difficult, as subjects slightly under a threshold likely have the same risk as those slightly above a threshold, but they have a real risk of being under-treated. In some health systems, antihypertensive drugs are dispensed free of charge to those that exceed the cutoff identified by the guidelines, whereas payment is required from those who do not reach the cutoff. In these situations, precise estimates of risks and benefits are essential in terms of equity of care and sustainability of the health system. Our data, which need to be confirmed in other populations, seem to indicate clearly that the current cutoff for the diagnosis of hypertension excludes a large proportion of the population with high cardiovascular risk caused by hemorheological alterations. Such individuals probably require a more appropriate therapeutic approach to reduce their cardiovascular risk.
These findings may have important clinical implications, which could potentially be useful in daily practice. In recent years, there has been a renewed interest in the topic of prehypertension. Our study adds important information about the increased cardiovascular risk observed in this condition. The present results, as well as the data available in the literature, provide evidence that the treatment (including pharmacological treatment) of prehypertension might be an appropriate strategy to control the burdens of hypertension and future cardiovascular disease.
However, this study leaves some questions open for further investigation. It is difficult to distinguish whether hemorheological alterations are causes or consequences of prehypertension. The observational design of this study does not allow the determination of whether increased viscosity is a cause of increased BP or a consequence of an intrinsic mechanism to regulate blood volume in this condition. It is known that many factors are involved in the pathophysiology of prehypertension, that is, the synthesis of different molecules, such as reactive oxygen species, cytokines, prostaglandins and C-reactive protein, as well as the activation of the renin–angiotensin system. All these factors can impair the synthesis and release of NO, causing endothelial dysfunction.38 NO regulates vascular tone to meet the metabolic demand and also exhibits antiatherosclerotic and antithrombotic properties. Furthermore, NO seems to affect RBC and platelet deformability as well as platelet adhesion and aggregation.26 This mechanism is reinforced by the finding that treatments lowering BP (for example, angiotensin-converting-enzyme inhibitors, calcium-channel-blocking agents and beta or alpha-receptor blockers) lead to significant improvements of endothelial function and blood rheology.39 Thus, based on this evidence, we hypothesize that increased blood viscosity might cause prehypertension, and endothelial dysfunction might increase blood viscosity. In both instances, the impairment of NO availability has a pivotal role.
In conclusion, our findings demonstrate that the values of BP in the range of so-called prehypertension are accompanied by important hemorheological changes, which are similar to those observed in people with overt hypertension. This result could explain the increased cardiovascular risk observed in these subjects as well as their susceptibility to hypertension. These observations could help redefine the thresholds of therapeutic interventions in individuals with high BP.
References
Baskurt OK, Meiselman HJ . Blood rheology and hemodynamics. Semin Thromb Hemost 2003; 29: 435–450.
Tzoulaki I, Murray GD, Lee AJ, Rumley A, Lowe GD, Fowkes FG . Relative value of inflammatory, hemostatic, and rheological factors for incident myocardial infarction and stroke: the Edinburgh Artery Study. Circulation 2007; 115: 2119–2127.
Tzoulaki I, Murray GD, Lee AJ, Rumley A, Lowe GD, Fowkes FG . Inflammatory, haemostatic, and rheological markers for incident peripheral arterial disease: Edinburgh Artery Study. Eur Heart J 2007; 28: 354–362.
Lee AJ, Mowbray PI, Lowe GD, Rumley A, Fowkes FG, Allan PL . Blood viscosity and elevated carotid intima-media thickness in men and women: the Edinburgh Artery Study. Circulation 1998; 97: 1467–1473.
Linde T, Sandhagen B, Hägg A, Mörlin C, Wikström B, Danielson BG . Blood viscosity and peripheral vascular resistance in patients with untreated essential hypertension. J Hypertens 1993; 11: 731–736.
Stergiou GS, Asayama K, Thijs L, Kollias A, Niiranen TJ, Hozawa A, Boggia J, Johansson JK, Ohkubo T, Tsuji I, Jula AM, Imai Y, Staessen JA . International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators. Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 2014; 63: 675–682.
Brown DW, Giles WH, Greenlund KJ . Blood pressure parameters and risk of fatal stroke, NHANES II mortality study. Am J Hypertens 2007; 20: 338–341.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Prospective Studies Collaboration. Lancet 2002; 360: 1903–1913.
Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, Levy D . Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291–1297.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D . Assessment of frequency of progression to hypertension in nonhypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001; 358: 1682–1686.
Erbel R, Lehmann N, Möhlenkamp S, Churzidse S, Bauer M, Kälsch H, Schmermund A, Moebus S, Stang A, Roggenbuck U, Bröcker-Preuss M, Dragano N, Weimar C, Siegrist J, Jöckel KH,, Heinz Nixdorf Recall Study Investigators. Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension: result of the Heinz Nixdorf Recall Study. Hypertension 2012; 59: 44–53.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ,, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–1252.
Beck DT, Martin JS, Casey DP, Braith RW . Exercise training improves endothelial function in resistance arteries of young prehypertensives. J Hum Hypertens 2014; 28: 303–309.
Huang Y, Cai X, Zhang J, Mai W, Wang S, Hu Y, Ren H, D . Prehypertension and Incidence of ESRD: a systematic review and meta-analysis. Am J Kidney Dis 2014; 63: 76–83.
Huang Y, Cai X, Li Y, Su L, Mai W, Wang S, Hu Y, Wu Y, Xu D . Prehypertension and the risk of stroke: a meta-analysis. Neurology 2014; 82: 1153–1161.
Huang Y, Cai X, Liu C, Zhu D, Hua J, Hu Y, Peng J, Xu D . Prehypertension and the risk of coronary heart disease in Asian and Western populations: a meta-analysis. J Am Heart Assoc 2015; 19: 1–11.
Egan BM, Stevens-Fabry S . Prehypertension—prevalence, health risks, and management strategies. Nat Rev Cardiol 2015; 12: 289–300.
Habib GB, Virani SS, Jneid H . Is 2015 the primetime year for prehypertension? Prehypertension: a cardiovascular risk factor or simply a risk marker? J Am Heart Assoc 2015; 19: 4.
Carallo C, Irace C, De Franceschi MS, Esposito T, Tripolino C, Scavelli F, Merante V, Gnasso A . The effect of HDL cholesterol on blood and plasma viscosity in healthy subjects. Clin Hemorheol Microcirc 2013; 55: 223–229.
Shimada S, Hasegawa K, Wada H, Terashima S, Satoh-Asahara N, Yamakage H, Kitaoka S, Akao M, Shimatsu A, Takahashi Y . High blood viscosity is closely associated with cigarette smoking and markedly reduced by smoking cessation. Circ J 2011; 75: 185–189.
Gyawali P, Richards RS, Bwititi PT, Nwose EU . Association of abnormal erythrocyte morphology with oxidative stress and inflammation in the metabolic syndrome. Blood Cells Mol Dis 2015; 54: 360–363.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE . ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Robinson SC, Brucer M . Range of normal blood pressure: a statistical and clinical study of 11383 persons. Arch Intern Med 1939; 69: 409–444.
Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM . Progression is accelerated from prehypertension to hypertension in blacks. Hypertension 2011; 58: 579–587.
Kim MJ, Lim NK, Choi SJ, Park HY . Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertens Res 2015; 38: 783–789.
Gori T, Forconi S. Endothelium and hemorheology. In: Baskurt OK, Hardeman M, Rampling MW, Meiselman HJ (eds). Handbook of Hemorheology and Hemodynamics, 1st edn. IOS Press: Amsterdam, The Netherlands, 2007, pp 339–350.
Gnasso A, Carallo C, Irace C, De Franceschi MS, Mattioli PL, Motti C, Cortese C . Association between wall shear stress and flow mediated vasodilation in healthy men. Atherosclerosis 2001; 156: 171–176.
Whittemore S, Cooley DA (eds). The Circulatory System (The Human Body: How It Works) 2nd edn. Chelsea House Publishers: New York, NY, USA. 2009, 74–87.
Hall JE, Guyton AC (eds). Guyton and Hall Textbook of Medical Physiology 13th edn. Elsevier Health Sciences: Philadelphia, PA, USA. 2015, 161–170.
Martini J, Carpentier B, Chávez Negrete A, Cabrales P, Tsai AG, Intaglietta M . Beneficial effects due to increasing blood and plasma viscosity. Clin Hemorheol Microcirc 2006; 35: 51–57.
de Simone G, Devereux RB, Chinali M, Best LG, Lee ET, Welty TK . Strong Heart Study Investigators. Association of blood pressure with blood viscosity in American Indians: the Strong Heart Study. Hypertension 2005; 45: 625–630.
Gori T, Wild PS, Schnabel R, Schulz A, Pfeiffer N, Blettner M, Beutel ME, Forconi S, Jung F, Lackner KJ, Blankenberg S, Münzel T . The distribution of whole blood viscosity, its determinants and relationship with arterial blood pressure in the community: cross-sectional analysis from the Gutenberg Health Study. Ther Adv Cardiovasc Dis 2015; 9: 354–365.
Jae SY, Kurl S, Laukkanen JA, Heffernan KS, Choo J, Choi YH, Park JB . Higher blood hematocrit predicts hypertension in men. J Hypertens 2014; 32: 245–250.
Salazar Vázquez BY, Martini J, Chávez Negrete A, Tsai AG, Forconi S, Cabrales P, Johnson PC, Intaglietta M . Cardiovascular benefits in moderate increases of blood and plasma viscosity surpass those associated with lowering viscosity: experimental and clinical evidence. Clin Hemorheol Microcirc 2010; 44: 75–85.
Branigan T, Bolster D, Vázquez BY, Intaglietta M, Tartakovsky DM . Mean arterial pressure nonlinearity in an elastic circulatory system subjected to different hematocrits. Biomech Model Mechanobiol 2011; 10: 591–598.
Carallo C, Irace C, De Franceschi MS, Coppoletta F, Tiriolo R, Scicchitano C, Scavelli F, Gnasso A . The effect of aging on blood and plasma viscosity. An 11.6 years follow-up study. Clin Hemorheol Microcirc 2011; 47: 67–74.
Takiwaki M, Tomoda F, Koike T, Taki T, Inoue H, Kigawa M, Kitajima I, Uji Y . Increased levels of small dense low-density lipoprotein cholesterol associated with hemorheological abnormalities in untreated, early-stage essential hypertensives. Hypertens Res 2014; 37: 1008–1013.
Albarwani S, Al-Siyabi S, Tanira MO . Prehypertension: underlying pathology and therapeutic options. World J Cardiol 2014; 6: 728–743.
Sumino H, Nara M, Seki K, Takahashi T, Kanda T, Ichikawa S, Goto-Onozato K, Koya S, Murakami M, Kurabayashi M . Effect of antihypertensive therapy on blood rheology in patients with essential hypertension. J Int Med Res 2005; 33: 170–177.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tripolino, C., Gnasso, A., Carallo, C. et al. Hemorheological profiles of subjects with prehypertension. Hypertens Res 39, 519–523 (2016). https://doi.org/10.1038/hr.2016.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.20
Keywords
This article is cited by
-
White blood cell and platelet distribution widths are associated with hypertension: data mining approaches
Hypertension Research (2024)
-
Prevalence of prehypertension and left ventricular hypertrophy
Hypertension Research (2017)