Abstract
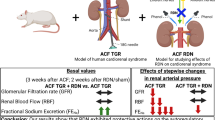
Chronic activation of the sympathetic nervous system (SNS) contributes to cardiac remodeling and the transition to heart failure (HF). Renal sympathetic denervation (RDN) may ameliorate this damage by improving renal function and sympathetic cardioregulation in hypertensive HF patients with renal injury. The efficacy may be comparable to that of chronic β-blocker treatment. Dahl salt-sensitive hypertensive rats were subjected to RDN in the hypertrophic stage. Another group of Dahl rats were subjected to sham operations and treated chronically with vehicle (CONT) or β-blocker bisoprolol (BISO). Neither RDN nor BISO altered the blood pressure; however, BISO significantly reduced the heart rate (HR). Both RDN and BISO significantly prolonged survival (22.2 and 22.4 weeks, respectively) compared with CONT (18.3 weeks). Echocardiography revealed reduced left ventricular (LV) hypertrophy and improved LV function, and histological analysis demonstrated the amelioration of LV myocyte hypertrophy and fibrosis in the RDN and BISO rats at the HF stage. Tyrosine hydroxylase and β1-adrenergic receptor (ADR) expression levels in the LV myocardium significantly increased only in the RDN rats, whereas the α1b-, α1d- and α2c-ADR expression levels increased only in the BISO rats. In both groups, renal damage and dysfunction were also reduced, and this reduction was accompanied by the suppression of endothelin-1, renin and angiotensin-converting enzyme mRNAs. RDN ameliorated the progression of both myocardial and renal damage in the hypertensive rats independent of blood pressure changes. The overall effects were similar to those of β-receptor blockade with favorable effects on HR and α-ADR expression. These findings may be associated with the restoration of the myocardial SNS and renal protection.
Similar content being viewed by others
Introduction
Chronic overactivation of the neurohormonal systems, including the sympathetic nervous system (SNS) and the rennin–angiotensin–aldosterone system, causes progressive cardiac remodeling and participates in the development and deterioration of heart failure (HF).1 Thus, the neurohormonal systems are major targets of established treatments for human HF, and blockade by angiotensin-converting enzyme inhibitors, aldosterone receptor blockers and β-blockers can improve prognoses. β-blocker therapy is an established treatment for chronic HF, the benefits of which include improvements of systolic and diastolic functions, reversal of remodeling, reduction of heart rate (HR) and blood pressure, inhibition of the rennin–angiotensin–aldosterone system, prevention of arrhythmia and anti-ischemic effects.2 Recently, additional strategies for the control of the SNS, such as spinal cord, vagal nerve, carotid artery pressoreceptive stimulation and renal sympathetic nerve denervation (RDN), have received much focus.3
The functions of the heart and kidney are closely related. HF is frequently associated with renal dysfunction/damage, whereas combined cardiac and renal dysfunction (cardiorenal syndrome) amplifies the progression of multiorgan failure and leads to extremely poor prognosis.4 Thus, improving renal function may help ameliorate cardiac dysfunction and thereby prevent cardiac remodeling and improve long-term prognosis.5, 6 Efferents of the renal sympathetic nerve reach the juxtaglomerular apparatus, renal tubules and vascular beds, where they promote renin secretion from the juxtaglomerular apparatus, increase sodium reabsorption by the renal tubule cells and decrease renal blood flow via the contraction of the renal artery.7 RDN is thus an effective treatment for drug-resistant hypertension and associated renal damage/function in chronic kidney diseases.8, 9 Furthermore, when the afferents of the renal sympathetic nerve are stimulated by nephropathy or renal ischemia, the central sympathetic system is activated along with an increase in SNS activity within the myocardium. The effects of SNS activation are mediated by nine different adrenergic receptors (ADRs; that is, α1a-, α1b-, α1d-, α2a-, α2b-, α2c-, β1-, β2- and β3-ADR). However, the pathophysiological significance and inter-relationship of presynaptic and postsynaptic ADR subtype diversities have not been fully resolved during the blockade of SNS in HF.10, 11
Given the influence of the renal sympathetic nerve on central sympathetic activity, we examined whether RDN can improve both kidney and heart function in Dahl salt-sensitive (DS) hypertensive rats, which develop concentric left ventricular (LV) hypertrophy (LVH) followed by HF with renal damage. In addition, we compared the efficacy of this treatment to that of β-receptor blockade and attempted to clarify the mechanism, particularly in terms of alteration of ADRs in the myocardium and kidney during HF.
Materials and methods
Animal model and experimental design
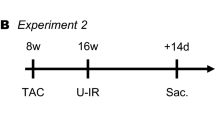
Male inbred DS rats were fed an 8% high-salt diet after the age of 6 weeks.12 These rats were randomized to either an RDN group (n=23) or a sham surgery group at 10–11 weeks of age, which corresponds to the LVH stage. Bilateral RDN was performed as previously described.13 Under anesthesia with 3% isoflurane, the renal arteries and veins were exposed through an abdominal incision and isolated from the surrounding connective tissue. The nerves were stripped by painting with 10% phenol in 95% ethanol. The sham surgery was performed using identical procedures with the exception that the renal nerves were left intact. The efficacy of the procedure was confirmed by reduced renal noradrenaline (NAd) content at 2 weeks after surgery. The sham-treated rats were then started on chronic treatment with bisoprolol (BISO group: n=22) or vehicle (CONT group: n=23). Bisoprolol was administered at 0.01% in the diet based on a previous study.14 A separate low-salt group (LS group: n=6) was fed a 0.3% salt diet throughout the course of the experiments. These rats did not exhibit hypertension or LVH throughout this time course.
In the first series of experiments, the animals (n=32) were monitored, and deaths were recorded every day for 23 weeks. In the second experiment, the animals (n=42) were killed at 17–18 weeks of age, which corresponded to the HF stage, to collect serum samples and to harvest cardiac and renal tissues for histological examinations and measurements of mRNA and protein expressions.
The animals were treated in accordance with the ‘Position of the American Heart Association on Research Animal Use’ adopted by the Association in November of 1984 and in accordance with the institutional guidelines of the Kinki University Faculty of Medicine.
Hemodynamic and echocardiographic studies
HR and systolic blood pressure were closely measured with the tail–cuff method at 10, 15 and 17 weeks. In addition, to measure the BP and HR in conscious animals over 24 h, a telemetry technique was also used in the rats (n=6 in each group) that were ~15-week old (4 weeks after treatment) as described previously.9 In brief, the telemetry catheter of a radiofrequency transmitter (TA11PA-C10, Data Sciences International, St Paul, ML, USA) was positioned into the abdominal aorta, and data were continuously collected for 4 days and analyzed using LabChart 7 pro (AD Instruments, Bella Vista, NSW, Australia). In vivo LV geometry and contractility were assessed by transthoracic echocardiography at 17 weeks as previously reported.12 The short axis view of the LV was recorded to measure the end-diastolic dimension, end-systolic dimension, posterior wall thickness and intraventricular septal wall thickness. The LV fractional shortening, LV mass, cardiac output and systolic wall stress were calculated.12
Urine, serum and tissue measurements
The rats were individually placed in metabolic cages, and urine samples were collected for 24 h at 10 weeks and at 15 or 17 weeks. The collected urine was used for measurements of urinary parameters (that is, urine sodium, potassium, nitrogen, creatinine, total protein and albumin or NAd). At 17–18 weeks, the rats were killed, and the collected serum was used for the measurement of serum parameters (that is, sodium, potassium, urea nitrogen, creatinine, aldosterone, plasma renin activity and NAd) using commercially available kits. The kidney cortex and LV tissues were homogenized in 0.4 N perchloric acid containing EDTA and L-ascorbic acid, and the NAd concentrations in the homogenates were measured using automated high-performance liquid chromatography.
Histological analysis
The excised hearts were separated into the right ventricle and LV and fixed in formalin. After paraffin embedding, the LV tissue was sliced into 5-μm sections. The sections were stained with hematoxylin–eosin, and the myocyte diameters were measured by two independent observers using the ImageJ software (NIH, Bethesda, MD, USA). Among 100 myocardial cells, the shortest diameters of the transversely cut fibers were measured at the level of the nucleus. Alternatively, to determine the level of myocardial interstitial fibrosis, the sections were stained with Picrosirius red as previously described.15 Immunohistochemical staining for tyrosine hydroxylase (TH) was performed using the UltraTek HRP Anti-Polyvalent (DAB) Staining System (Scytek Laboratories, Logan, UT, USA) according to the manufacturer’s instructions. The primary antibody used was a rabbit anti-TH antibody (1:750 Abcam, Cambridge, UK).
The excised kidneys were separated into upper and lower poles and fixed. The fixed tissues were sliced, and the sections were stained with either hematoxylin–eosin, Masson-trichrome, anti-desmin antibody or Picrosirius red. Glomerular sclerosis (GS) was graded semiquantitatively in each glomerulus, and the individual scores (GS scores) were calculated using a scale that ranged from 0 to 4 (0, no GS; 1, segmental GS in <25% of the glomeruli; 2, segmental GS in 25 –50% of the glomeruli; 3, segmental GS in 50–75% of the glomeruli; and 4, segmental GS in >75% of the glomeruli). These scores were averaged more than 60 glomeruli per animal.16 Immunohistochemical staining for desmin was performed using a mouse monoclonal against human desmin (D33, DAKO, Glostrup, Denmark). In addition, the tubulointerstitial fibrosis was quantified (% fibrotic area) in six randomly chosen high-power fields per kidney in the Picrosirius red sections using the ImageJ software.
Quantitative real-time polymerase chain reaction
Total RNA was extracted using TRIzol and treated with DNase I (Invitrogen, Carlsbad, CA, USA). Single-strand cDNAs were generated by reverse transcription of the RNA samples using the SuperScript first-strand synthesis system kit (Invitrogen) and then subjected to quantitative real-time polymerase chain reaction (PCR) with Power SYBR green PCR Master Mix using a StepOnePlus real-time PCR system (Applied Biosystems, Carlsbad, CA, USA). The mRNA levels (Supplementary Table) were normalized to those of GAPDH (endogenous control).
Western blot analysis
The total cytosolic proteins were extracted from 40 mg of the LV myocardium using the Mem-PER Plus Membrane Protein Extraction Kit (Thermo Scientific, Waltham, MA, USA), separated on 4–12% Bis-tris gels (8 μg per lane), and transferred to polyvinylidene fluoride membranes. The membranes were incubated with specific rabbit anti-TH antibody (1:10 000, Abcam) or rabbit anti-GAPDH (1:10 000, CST, Danvers, MA, USA) followed by horseradish peroxidase (HRP)-conjugated goat anti-rabbit antibody. The immune complexes were detected with a chemiluminescence kit (ECL Prime, GE Healthcare, Little Chalfont, UK).
Statistical analysis
All data are expressed as the means±s.d.'s. The group means were compared with one-way analysis of variance with post hoc Tukey’s honestly significant difference tests. Two-way repeated-measures analyses of variance were used to compare the HR, systolic blood pressure and urinary parameters between the groups. The group survivals (RDN vs. CONT group and BISO vs. CONT) were compared with standard Kaplan–Meier analysis and log-rank tests. P<0.05 was considered statistically significant.
Results
Prolonged survival of DS hypertensive rats due to RDN and β-blocker treatment
Ten rats in the untreated hypertensive CONT group died of pulmonary congestion with severe LV dysfunction after 15 weeks (median survival: 18.3 weeks). Kaplan–Meier analysis revealed significantly prolonged survival (P<0.01) in the RDN group (22.2 weeks) and the BISO group (22.4 weeks) compared with the CONT group (Figure 1). There was no significant difference in survival between the RDN and BISO groups, which suggested that the RDN and β-blockade exhibited equal efficacies.
Hemodynamic and pathological changes in the heart structures
Both the RDN and BISO groups exhibited significantly increased body weights (BWs; P<0.01 vs. the CONT group). There were no differences in the systolic blood pressure between the three groups during this study. The RDN group exhibited an HR reduction only at 15 weeks (during the pre-HF phase), whereas the BISO group exhibited a significantly reduced HR over the entire study period (P<0.01 vs. both the CONT and RDN groups; Figure 2a). In the animals at ~15 weeks, telemetric analysis also demonstrated no significant differences in the mean blood pressures over 24 h between the three groups (Figure 2b). The difference between the daytime and nighttime mean blood pressures was restored only in the RDN group. An HR reduction was observed only in the BISO group, and no differences between the daytime and nighttime mean HRs were observed between the three groups. Echocardiography revealed significant suppressions of LV enlargement (LV diastolic dimension), hypertrophy (LV mass), systolic wall stress and improved LV fractional shortening in the HF stage (17 weeks) in both the RDN and BISO rats compared with the CONT hypertensive rats. Although cardiac output was significantly decreased in the CONT group compared with the LS group, no significant difference was observed between the three treatment groups (Figure 2c and Supplementary Table 2).
Changes in (a) body weight, heart rate and systolic blood pressure at 10–17 W, (b) 24-h mean heart rate, mean blood pressure at 15 W, (c) echocardiographic parameters at 17 W and (d, e) urinary parameters at 10–15 W. BISO, bisoprolol group; BP, blood pressure; CONT, control group; Dd, dimension at diastole; FS, fractional shortening; HR, heart rate; LS, low-salt group; LV, left ventricle; RDN, renal denervation group; W, weeks. The values are presented as the means±s.d.'s. *P<0.05.
Serum and urine chemistries
There were no differences in the urine volumes or total sodium excretions between the groups. The daily sodium/water balance did not vary between the three treatment groups (Table 1). However, the RDN and BISO groups demonstrated significantly lower total urine protein and urine albumin excretions compared with the CONT group (Figure 2d), which suggested an amelioration of renal dysfunction. As expected based on sympathetic hyperactivity, the urine NAd was significantly higher in the CONT group compared with the LS groups at 15 weeks, whereas the RDN (but not the BISO) group exhibited significantly reduced serum NAd (Figure 2e). At 17 weeks, both treatment groups also exhibited lower creatinine clearance compared with the CONT group (P<0.05, Table 1), which is again consistent with the preservation of renal function.
The increased serum NAd concentration in the CONT group was significantly suppressed in both the RDN and BISO groups. The decrease in LV NAd content in the CONT group was significantly reversed by RDN, which was suggestive of the preservation of heart sympathetic function. In contrast, the NAd content in the kidneys was significantly suppressed in both RDN and BISO groups; however, the suppression was greater in the RDN group (P<0.05).
Reduced LV and renal histopathological damage in the HF stage due to the RDN and β-blocker treatments
Both treatment groups exhibited significantly lower lung/BW ratios compared with the CONT group, which indicated a suppression of lung congestion (Table 1) and significant decreases in both the LV/BW ratio and the kidney/BW ratio. No differences in lung/BW, LV/BW or kidney/BW ratios were observed between the RDN and BISO groups.
Histological analysis revealed significantly smaller mean ventricular myocyte diameters in the RDN and BISO groups compared with the CONT group (P<0.05). Both treatment groups also exhibited significantly smaller myocardial fibrotic areas (P<0.05; Figure 3a). In the kidney, focal segmental or global glomerulosclerosis were less frequently observed in the CONT group than in the treatment groups as expressed by the GS scores (Figure 3b). The desmin scores were also significantly lower in the RDN and BISO groups than in the CONT group, which indicated that the podocyte cytoskeletal damage was ameliorated by these treatments. In addition, the treatment groups exhibited reduced fibrosis in the tubulointerstitium around the sclerosing glomeruli and arterioles (lower % of fibrotic area) compared with the CONT group.
Histological analysis of the left ventricular myocardium and kidney. (a) Representative images of the myocardial sections stained with hematoxylin–eosin or Picrosirius red and the quantitative analyses of myocyte cell diameter and fibrotic area. (b) Representative images of the glomerular sections with hematoxylin–eosin or anti-desmin staining and the tubulointerstitial sections with Picrosirius red staining. Semiquantitative analysis of the glomerular sclerosis (GS) score and quantitative analysis of the anti-desmin staining and fibrotic area. BISO, bisoprolol group; CONT, control group; LS, low-salt group; RDN, renal denervation group. The scale bar indicates 50 μm. The values represent the means±s.d.'s. *P<0.05.
Changes in mRNA and TH protein expression in the LV myocardium
Figure 4 summarizes the changes in the various mRNA expression levels in the LV myocardia. The myocardial mRNA levels of atrial natriuretic peptide, arginine vasopressin and galectin-3 were significantly suppressed by the NDR and BISO treatments compared with the CONT group. The expression of angiotensin-converting enzyme mRNA was significantly suppressed only in the RDN group. No significant differences were observed in the mRNA expression levels of β-myosin heavy chain between the groups (Figure 4a).
Changes in left ventricular myocardium mRNA and protein expressions. (a, b) mRNA levels expressed relative to the low-salt (LS) group rats. (c) Representative images of TH with anti-TH staining. (d) Quantification of TH protein using western blot analysis. ADR, adrenergic receptor; ANP, atrial natriuretic peptide; AVP, arginine vasopressin; BISO, bisoprolol group; β-MHC, β-myosin heavy chain; CONT, control group; GAPDH, glyceraldehyde-3-phosphate dehydrogenase; GRK2, G-coupled protein receptor kinase 2; TH, tyrosine hydroxylase; RDN, renal denervation group. The protein levels are expressed relative to the LS group rats. The scale bar indicates 50 μm. The data are presented as the means±s.d.'s. *P<0.05.
Although there was no difference in the β1-adrenergic receptor (ADR) mRNA expression between the LS and CONT groups, a significant increase was observed in the RDN group (P<0.05). The increased expression levels of β2-ADR and G-protein-coupled receptor kinase 2 were not suppressed by the RDN or BISO treatments. The suppressions of α1b and α1d adrenergic mRNAs in the CONT rats were significantly reversed only by the BISO treatment, and only the BISO treatment enhanced α2c mRNA expression (Figure 4b).
Representative images of the TH immunohistochemistry are presented in Figure 4c. The TH-positive nerve cell density was decreased in the CONT group compared with the LS group. This expression level was restored in the RDN group. Western blot analysis revealed significantly decreased expression of TH in the CONT group, and only the RDN group demonstrated a significant reversal in this TH underexpression, which suggest that the sympathetic nerve dysfunction in the LV was restored by RDN treatment (Figure 4d).
Changes in mRNA in the kidney
Figure 5 summarizes the changes in mRNA expression in the kidney. The overexpressions of endothelin-1, renin and angiotensin-converting enzyme mRNAs in the CONT group were significantly suppressed by both treatments. Alternatively, Col1a1 overexpression was not affected by either treatment, and CTGF overexpression was suppressed only by BISO (P<0.05; Figure 5a).
Changes in (a, b) kidney mRNA expression. The mRNA levels are expressed relative to the LS group rats (1.0). ACE, angiotensin-converting enzyme; ADR, adrenergic receptor; BISO, bisoprolol group; Col1a1, collagen type Ia; CONT, control group; ET-1, endothelin-1; GRK2, G-coupled protein receptor kinase 2; LS, low-salt group; RDN, renal denervation group. The data are presented as the means±s.d.'s. *P<0.05.
The expression levels of the β1-, β2-, α1b- and α1d-ADRs were not affected by either treatment. The expression levels of the α1a and α2a mRNAs were suppressed by BISO, and α2c expression was suppressed by both RDN and BISO (Figure 5b).
Discussion
In hypertensive rats, RDN mitigated the development of LV hypertrophy and the transition to HF and protected against glomerular and tubular damage in the kidney independent of blood pressure changes and thus resulted in prolonged survival. Compared with chronic β-blocker treatment with bisoprolol, which also reduced heart and kidney damage, RDN exerted greater protective effects in the LV sympathetic system. In contrast, bisoprolol treatment caused persistent HR reduction and affected the expressions of α-ADRs in both the LV and kidney. These findings suggest that RDN may have therapeutic potential, especially in patients with HF and progressive renal impairment (so-called cardiorenal syndrome).
Absence of a blood pressure-lowering effect
In the present study, RDN did not exhibit a blood pressure-lowering effect as indicated by the tail–cuff method and telemetric analysis. Currently, the mechanisms by which RDN attenuates any form of HT are the subject of great debate, and the reason that RDN did not reduce blood pressure in this model remains uncertain. The present study suggests that sympathetic overactivity itself was implicated in heart and kidney damage, but did not mediate hypertension in this Dahl rat model. Indeed, RDN is not equally effective in each patient with HT, and previous studies have also suggested that renal nerves do not provide a major contribution to the development of HT and that the SNS might not be associated with hypertension in this animal model.
The renal pressure–natriuresis relationship is critical for salt-sensitive blood pressure regulation. Indeed, in other hypertensive animal models, RDN may cause a leftward shift of the pressure–natriuresis curve and increase sodium excretion ability.17 Theoretically, reduced sympathetic innervation of the kidney and the prevention of rennin–angiotensin–aldosterone system activation by RDN may be associated with blood pressure changes and increases in urinary sodium excretion. However, we did not observe any changes in renal sodium excretion or daily sodium/water balance due to RDN. These findings are also consistent with other previous studies in Dahl rats.9, 18, 19 In addition, we assessed cardiac output via echocardiography, but RDN did not affect the results or the consequent vascular resistance (Supplementary Table 2). These findings may be the reasons that RDN did not reduce blood pressure in this Dahl rat model.
In the present study, RDN and not a beta-blocker improved blood pressure variability; RDN decreased the mean blood pressure only during the daytime (corresponding to nighttime in humans). This finding may correspond to an improvement in the non-dipper phenomenon in hypertension that is associated with end-organ damage and worsened clinical outcomes. By reducing sympathetic activity, RDN might have improved the alteration/imbalance in the autonomic nervous function and decreased the mean blood pressure in the daytime.20 Interestingly, based on a substudy of the SYMPLICITY HTN-3 trial, Bakris et al.21 reported that the nocturnal BP dropped significantly from baseline because of RDN, and a trend was noted toward a greater nighttime BP reduction in the denervation group compared with the sham control group. These results suggest the need for further research on the physiological effects of RDN.
Effects of RDN on cardiac hypertrophy and HF: comparison with β-blockade
The benefits of RDN have been examined in experimental HF animals. Schiller et al.22 and Hu et al.23 reported that RDN improves cardiac autonomic imbalances by reducing sympathetic tone in pacing-induced HF and postmyocardial infarcted HF models, respectively. In untreated Dahl hypertensive HF model rats, the NAd content of the LV was significantly reduced in the HF stage possibly because of depletion, decreased reuptake and/or increased spillover following prolonged sympathetic activation. Reduced myocardial NAd content, which is indicative of cardiac sympathetic denervation, has been linked to death because of progressive HF in humans.24 In the present study, RDN significantly decreased urine NAd excretion, which was suggestive of the alleviation of central SNS, and restored NAd content and TH protein expression and increased β1-receptor expression in the LV myocardium. RDN may block the activation of the central SNS by disrupting renal afferents, and increases in the LV NAd concentration may further alleviate the activation of the central SNS by negative feedback.25 Blood pressure-independent effects of sympathectomy on LV hypertrophy have been described in an abdominal aortic-banding model in which blood pressure is unaffected by sympathectomy but LV hypertrophy is significantly decreased.17 In contrast, Linz et al.26 reported that RDN attenuated the blood pressure increase, the progression of renal injury and cardiac remodeling in obese spontaneously hypertensive rats. Eriguchi et al.27 reported that, although RDN did lower blood pressure in rats that were administered L-NAME, the protective effects against heart and kidney damage were greater than those of hydralazine when blood pressure was maintained. Collectively, RDN may mitigate cardiac or renal damage, at least partially, independent of blood pressure change.
Chronic bisoprolol treatment did not restore the NAd content or TH protein or increase β1-receptor expression in the LV myocardium in contrast to RDN. Alternatively, bisoprolol at the dose (≈3 mg kg−1 per day) used in the present study caused a persistent HR reduction of ~17% without lowering blood pressure. In dogs with LV dysfunction, the favorable effects of β-blockers on ventricular remodeling disappear when HR reduction is prevented by electrical pacing.28 Moreover, in HF patients, the reduction in oxygen expenditure that results from the negative chronotropic effect has been suggested to be an important mechanism that accounts for the salutary effect of β-blockade therapy.29
Cardiomyocytes express α1-ADRs but not α2-ADRs. Although α1-ADRs are not generally considered to be major regulators of cardiac function under physiological conditions, they have been thought to exert greater influence under some pathological circumstances. In contrast, α2-ADRs exist in both the brainstem (central sympathoinhibition) and presynaptically on peripheral sympathetic nerves (where they regulate NE release). In animal studies, double-knockout mice lacking myocardial α1a- and α1b-ADRs have been found to exhibit deceased responsiveness to β-ADR stimulation and a pathophysiological phenotype that included some (but not all) of the features of failing hearts.30 α2a- and α2c-ADRs are essential in the control of the circulating levels of NAd, and the dysfunction of these receptors is associated with HF progression in knockout mice.31 Moreover, in humans, peripheral sympathoneural α2-ADRs have been demonstrated to be functionally important in the inhibition of NE release, and this function is lost in HF.32 In the present study, in addition to HR reduction, the restorations of α1b- and α1d-ADR expressions and the increase in α2c-ADR were only observed in the BISO group. It is possible that the unique effects of β-blockade or bisoprolol contributed to the prevention of HF progression.
Benefits of RDN for kidney diseases
The renoprotective effects of RDN have been demonstrated in several experimental models of progressive kidney disease. The suppression of efferent renal sympathetic nerve activity may decrease renin secretion and sodium reabsorption or increase renal blood flow.33, 34 Our study suggests that RDN has direct renal effects that are independent of any changes in blood pressure and are possibly related to the suppression of local neurohormonal factors such as endothelin-1, renin and angiotensin-converting enzyme. Nagasu et al.9 reported protective effects of RDN against GS that were mediated via the suppression of reactive oxygen species in the same DS hypertensive rat model. These authors suggested that these effects may stem from the suppression of NAD(P)H oxidase activation via β1-receptors.
The kidney expresses both α1 - and α2-ADRs; however, the roles of renal α1- and α2-ADRs, particularly under pathologic conditions, remain poorly understood. Recently, Kim et al.35 reported that RDN prevents both fibrogenesis and the inflammatory cascade in a ureteral obstruction model. These authors showed that NAd and calcitonin gene-related peptide (CGRP) act through α2-ADR and CGRP receptors, respectively, to drive renal fibrosis and that RDN blocks both pathways. These mechanisms may also underlie the effects of RDN observed in the present study. RDN decreased the NAd and CGRP contents in the kidney and may suppress ROS production in the glomeruli via β1-receptor blockade and fibrosis in the interstitium through α2-ADR and CGRP receptor blockade. Although the decrease in renal NAd content was modest in the bisoprolol treatment group, similar protective mechanisms may be operative because both the α2a and α2c expression levels were significantly suppressed.
Study limitations
This study has several limitations. This study was performed in a specific disease model of inbred DS hypertensive rats with both progressive myocardial and renal damages. The effects of RDN and bisoprolol treatment need to be compared as do the underlying mechanisms that have been investigated in other HF models that are associated with relatively mild renal damage, such as postmyocardial infarction, myocarditis and postaortic banding models. It is possible that renal nerve regeneration occurs following RDN.36 Although the renal nerves have been reported to be fully reinnervated within 8 weeks in rats, RDN was observed to be persistently effective over ~8 weeks in the present study. Future studies need to examine whether repeated RDN further improves renal and cardiac damage/dysfunction.
Perspectives/clinical implications
RDN involved the complete denervation of both the afferent and efferent renal nerves in the present animal study. In the recent SYMPLICITY HTN-3 trial, the issue of procedural competency and suboptimal denervation was raised in terms of why this procedure resulted in negative findings.8 Specifically, the current radiofrequency RDN may not be the most effective method for delivering deeper and more circumferential spread to achieve better sympathetic nerve destruction. However, the techniques and tools for complete denervation in humans are improving, and many companies are now working on different RDN methods, such as ultrasound and the local pharmacologic injection of neurotoxic agents.37 It is now more important than ever that the basic mechanisms underlining RDN are clarified.
The present data suggest that RDN ameliorates the development of LV hypertrophy and HF independent of blood pressure changes in hypertensive rats with LV hypertrophy. Recently, RDN has been reported to improve LV hypertrophy and diastolic function in patients with drug-resistant hypertension without significantly affecting systolic blood pressure or HR.38 These findings suggest that a direct effect of altered sympathetic activity also occurs in diseased human hearts. RDN may thus have therapeutic potential for patients with HF and progressive renal impairment, even in the absence of a blood pressure-reducing effect (Figure 6).
References
Schrier RW, Abraham WT . Hormones and hemodynamics in heart failure. N Engl J Med. 1999; 341: 577–585.
Barrese V, Taglialatela M . New advances in beta-blocker therapy in heart failure. Front Physiol 2013; 4: 323.
Singh JP, Kandala J, Camm AJ . Non-pharmacological modulation of the autonomic tone to treat heart failure. Eur Heart J 2014; 35: 77–85.
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R . Cardiorenal syndrome. J Am Coll Cardiol 2008; 52: 1527–1539.
Hillege HL, Nitsch D, Pfeffer MA, Swedberg K, McMurray JJ, Yusuf S, Granger CB, Michelson EL, Ostergren J, Cornel JH, de Zeeuw D, Pocock S, van Veldhuisen DJ, Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) Investigators. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation 2006; 113: 671–678.
Schiffrin EL, Lipman ML, Mann JF . Chronic kidney disease: effects on the cardiovascular system. Circulation 2007; 116: 85–97.
DiBona GF, Esler M . Translational medicine: the antihypertensive effect of renal denervation. Am J Physiol Regul Integr Comp Physiol 2010; 298: R245–R253.
Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL, SYMPLICITY HTN-3 Investigators. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014; 370: 1393–1401.
Nagasu H, Satoh M, Kuwabara A, Yorimitsu D, Sakuta T, Tomita N, Kashihara N . Renal denervation reduces glomerular injury by suppressing NAD(P)H oxidase activity in Dahl salt-sensitive rats. Nephrol Dial Transplant 2010; 25: 2889–2898.
Jensen BC, O'Connell TD, Simpson PC . Alpha-1-adrenergic receptors in heart failure: the adaptive arm of the cardiac response to chronic catecholamine stimulation.. J Cardiovasc Pharmacol 2014; 63: 291–301.
Baker AJ . Adrenergic signaling in heart failure: a balance of toxic and protective effect. Pflugers Arch 2014; 466: 1139–1150.
Inoko M, Kihara Y, Morii I, Fujiwara H, Sasayama S . Transition from compensatory hypertrophy to dilated, failing left ventricles in Dahl salt-sensitive rats. Am J Physiol 1994; 267: H2471–H2482.
Pires NM, Igreja B, Moura E, Wright LC, Serrão MP, Soares-da-Silva P . Blood pressure decrease in spontaneously hypertensive rats following renal denervation or dopamine β-hydroxylase inhibition with etamicastat. Hypertens Res 2015; 38: 605–612.
Iwanaga Y, Kihara Y, Takenaka H, Kita T . Down-regulation of cardiac apelin system in hypertrophied and failing hearts: possible role of angiotensin II-angiotensin type 1 receptor system. J Mol Cell Cardiol 2006; 41: 798–806.
Iwanaga Y, Hoshijima M, Gu Y, Iwatate M, Dieterle T, Ikeda Y, Date MO, Chrast J, Matsuzaki M, Peterson KL, Chien KR, Ross J Jr . Chronic phospholamban inhibition prevents progressive cardiac dysfunction and pathological remodeling after infarction in rats. J Clin Invest 2004; 113: 727–736.
Adhikary LP, Yamamoto T, Isome M, Nakano Y, Kawasaki K, Yaoita E, Kihara I . Expression profile of extracellular matrix and its regulatory proteins during the process of interstitial fibrosis after antiglomerular basement membrane antibody-induced glomerular sclerosis in Sprague-Dawley rats. Pathol Int 1999; 49: 716–725.
Perlini S, Palladini G, Ferrero I, Tozzi R, Fallarini S, Facoetti A, Nano R, Clari F, Busca G, Fogari R, Ferrari AU . Sympathectomy or doxazosin, but not propranolol, blunt myocardial interstitial fibrosis in pressure-overload hypertrophy. Hypertension 2005; 46: 1213–1218.
Osborn JL, Roman RJ, Ewens JD . Renal nerves and the development of Dahl salt-sensitive hypertension. Hypertension 1988; 11: 523–528.
Foss JD, Fink GD, Osborn JW . Reversal of genetic salt-sensitive hypertension by targeted sympathetic ablation. Hypertension 2013; 61: 806–811.
Kohara K, Nishida W, Maguchi M, Hiwada K . Autonomic nervous function in non-dipper essential hypertensive subjects. Evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808–814.
Bakris GL, Townsend RR, Liu M, Cohen SA, D'Agostino R, Flack JM, Kandzari DE, Katzen BT, Leon MB, Mauri L, Negoita M, O'Neill WW, Oparil S, Rocha-Singh K, Bhatt DL, SYMPLICITY HTN-3 Investigators. Impact of renal denervation on 24-hour ambulatory blood pressure: results from SYMPLICITY HTN-3. J Am Coll Cardiol 2014; 64: 1071–1078.
Schiller AM, Haack KK, Pellegrino PR, Curry PL, Zucker IH . Unilateral renal denervation improves autonomic balance in conscious rabbits with chronic heart failure. Am J Physiol Regul Integr Comp Physiol 2013; 305: R886–R892.
Hu J, Yan Y, Zhou Q, Ji M, Niu C, Hou Y, Ge J . Effects of renal denervation on the development of post-myocardial infarction heart failure and cardiac autonomic nervous system in rats. Int J Cardiol 2014; 172: e414–e416.
Brunner-La Rocca HP, Esler MD, Jennings GL, Kaye DM . Effect of cardiac sympathetic nervous activity on mode of death in congestive heart failure. Eur Heart J 2001; 22: 1136–1143.
Malpas SC . Sympathetic nervous systemoveractivity and its role in the development of cardiovascular disease. Physiol Rev 2010; 90: 513–557.
Linz D, Hohl M, Schütze J, Mahfoud F, Speer T, Linz B, Hübschle T, Juretschke HP, Dechend R, Geisel J, Rütten H, Böhm M . Progression of kidney injury and cardiac remodeling in obese spontaneously hypertensive rats: the role of renal sympathetic innervation. Am J Hypertens 2015; 28: 256–265.
Eriguchi M, Tsuruya K, Haruyama N, Yamada S, Tanaka S, Suehiro T, Noguchi H, Masutani K, Torisu K, Kitazono T . Renal denervation has blood pressure-independent protective effects on kidney and heart in a rat model of chronic kidney disease. Kidney Int 2015; 87: 116–127.
Nagatsu M, Spinale FG, Koide M, Tagawa H, DeFreitas G, Cooper G 4th, Carabello BA . Bradycardia and the role of beta-blockade in the amelioration of left ventricular dysfunction. Circulation 2000; 101: 653–659.
Yamakawa H, Takeuchi M, Takaoka H, Hata K, Mori M, Yokoyama M . Negative chronotropic effect of beta-blockade therapy reduces myocardial oxygen expenditure for nonmechanical work. Circulation 1996; 94: 340–345.
McCloskey DT, Turnbull L, Swigart P, O'Connell TD, Simpson PC, Baker AJ . Abnormal myocardial contraction in alpha(1A)- and alpha(1B)-adrenoceptor double-knockout mice. J Mol Cell Cardiol 2003; 35: 1207–1216.
Brede M, Wiesmann F, Jahns R, Hadamek K, Arnolt C, Neubauer S, Lohse MJ, Hein L . Feedback inhibition of catecholamine release by two different alpha2-adrenoceptor subtypes prevents progression of heart failure. Circulation 2002; 106: 2491–2496.
Aggarwal A, Esler MD, Socratous F, Kaye DM . Evidence for functional presynaptic alpha-2 adrenoceptors and their down-regulation in human heart failure. J Am Coll Cardiol 2001; 37: 1246–1251.
DiBona GF . Neural control of renal function: cardiovascular implications. Hypertension 1989; 13: 539–548.
Clayton SC, Haack KK, Zucker IH . Renal denervation modulates angiotensin receptor expression in the renal cortex of rabbits with chronic heart failure. Am J Physiol Renal Physiol 2011; 300: F31–F39.
Kim J, Padanilam BJ . Renal nerves drive interstitial fibrogenesis in obstructive nephropathy. J Am Soc Nephrol 2013; 24: 229–242.
Kline RL, Mercer PF . Functional reinnervation and development of supersensitivity to NE after renal denervation in rats. Am J Physiol 1980; 238: R353–R358.
Reddy VY, Olin JW . Renal denervation for resistant hypertension: not dead yet. J Am Coll Cardiol 2014; 64: 1088–1091.
Brandt MC, Mahfoud F, Reda S, Schirmer SH, Erdmann E, Böhm M, Hoppe UC . Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol 2012; 59: 901–909.
Acknowledgements
We thank Kumi Ohmi, Shigeaki Yamanaka and Nobuyuki Mizukuchi for technical assistance. The bisoprolol was graciously supplied by the Mitsubishi Tanabe Pharma Corporation of Tokyo, Japan. This work was supported in part by a Grant-in-aid from the Japan Society for the Promotion of Science (22590815).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Watanabe, H., Iwanaga, Y., Miyaji, Y. et al. Renal denervation mitigates cardiac remodeling and renal damage in Dahl rats: a comparison with β-receptor blockade. Hypertens Res 39, 217–226 (2016). https://doi.org/10.1038/hr.2015.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.133
Keywords
This article is cited by
-
Comparison of the effects of renal denervation at early or advanced stages of hypertension on cardiac, renal, and adipose tissue pathology in Dahl salt-sensitive rats
Hypertension Research (2024)
-
Increased Renal Dysfunction, Apoptosis, and Fibrogenesis Through Sympathetic Hyperactivity After Focal Cerebral Infarction
Translational Stroke Research (2022)
-
Renal sympathetic nerve activity regulates cardiovascular energy expenditure in rats fed high salt
Hypertension Research (2020)
-
Renal denervation reduces sympathetic overactivation, brain oxidative stress, and renal injury in rats with renovascular hypertension independent of its effects on reducing blood pressure
Hypertension Research (2019)
-
Modulation of cardiac stem cell characteristics by metoprolol in hypertensive heart disease
Hypertension Research (2018)