Abstract
Hypertension prevalence is increasing globally, yet little is known about the occurrence of masked hypertension (MHT) in young, sub-Saharan African adults, and how it relates to elevated cardiovascular risk. The African-PREDICT study (recruitment based on normotensive clinic blood pressure (BP)) determined the frequency of MHT and its relationship with arterial stiffness and biochemical markers of inflammation and endothelial activation. We included men and women (n=352), 20–30 years, screened for normotensive clinic BP (54% white, 40% men). Clinic BP, ambulatory blood pressure monitoring (ABPM), central systolic pressure, aortic pulse wave velocity (aPWV), augmentation index, anthropometry, physical activity and biochemical markers of cardiovascular risk were assessed (lipids, glucose, insulin, markers of endothelial activation and inflammation). Eighteen percent of the study population had MHT (60% white, 68% men). Those with MHT had increased adiposity, clinic-, ABPM- (24-h, day and night) and central-BP (within normal ranges), heart rate, aPWV and biochemical markers of cardiovascular risk, compared with normotensives (all P<0.05). Using multivariable adjusted odds ratios, we found that MHT was associated with increased likelihood for higher aPWV (odds ratio (OR)=1.567, P=0.010), insulin (OR=1.499, P=0.049), monocyte chemoattractant protein-1 (OR=1.499, P=0.026), vascular cellular adhesion molecule (OR=1.409, P=0.042) and C-reactive protein (OR=1.440, P=0.044). In a young adult (supposedly healthy) cohort, the occurrence of MHT is alarming, especially since MHT further demonstrated elevated cardiovascular risk via increased adiposity, arterial stiffness, endothelial activation and inflammation. Detection of MHT is crucial to increase awareness of elevated cardiovascular risk, and to ensure the required lifestyle and/or pharmaceutical interventions.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the main cause of death globally, and more than 80% of CVD deaths occur in low- and middle-income countries.1 South Africa is a country undergoing rapid urbanization, and in a recent study conducted in six developing countries worldwide, South Africa had the highest levels of hypertension in adults over the age of 50 years.2 Earlier detection and effective treatment of hypertension in this population are therefore imperative. Hypertension is primarily diagnosed by clinic blood pressure (BP) measurement, which does not allow for the detection of masked hypertension (MHT).
MHT is a risk factor for CVD and is a condition where a patient presents as normotensive in clinic, but is hypertensive when BP is measured over 24-h using ambulatory blood pressure monitoring (ABPM).3, 4, 5, 6 The more commonly known white coat hypertension is in contrast to MHT and results in patients being unnecessarily pharmaceutically treated for hypertension.7 MHT is a concern as patients are less easily diagnosed and are therefore untreated and unaware of their elevated cardiovascular risk.8 Studies conducted in white and Japanese populations identified MHT as an important cardiovascular risk factor9, 10 and suggested MHT to have a higher prevalence than white coat hypertension.11
The underlying pathology of MHT is not entirely understood. The prevalence of MHT has mostly been determined in diseased, older populations12, 13 and has not been determined in sub-Saharan African adults. It may therefore be of particular value to determine the frequency of MHT in young black and white adults, who are expected to be healthy and normotensive. Whether other cardiovascular risk markers besides BP are elevated in such a population is unknown. Factors such as arterial stiffness, lipids, markers of inflammation and endothelial activation are associated with increased cardiovascular risk, morbidity and mortality.14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 It may increase our understanding of MHT to determine whether such markers are increased in young adult, masked hypertensives.
Therefore, we explored whether MHT occurs in young, black and white South Africans who were recruited on the basis of normotensive clinic BP. We reviewed several hemodynamic (peripheral clinic BP, ABPM BP, central systolic pressure, aortic pulse wave velocity (aPWV) and augmentation index (AIx)), biochemical (lipids, glucose, insulin, endothelial activation markers (intracellular adhesion molecules (I-CAM), vascular cellular adhesion molecules (V-CAM), monocyte chemoattractant protein-1 (MCP-1))) and inflammatory markers (interleukin-6 (IL-6), C-reactive protein (CRP), tumor necrosis factor-α (TNF-α) and reactive oxygen species (ROS))) of cardiovascular risk in participants with MHT compared with normotensive participants.
Methods
Study population
Participants were recruited as part of the African-PREDICT (PRospective study on the Early Detection and Identification of Cardiovascular disease and hyperTension) longitudinal study. The aim of this project is to follow young, healthy, normotensive adults over a 20-year period in order to identify novel markers of early cardiovascular risk in an apparently healthy population. The current sub-study initially included cross-sectional data from the first 403 participants.
The study complied with all applicable requirements of the US and International Regulations, in particular, the Helsinki Declaration of 1975 (as revised in 2008), for investigation of human participants. The study was approved by the Health Research Ethics Committee of the North-West University (Potchefstroom Campus). All participants provided written, informed consent.
Active participant recruitment takes place on a continuous basis. Participants are invited from Potchefstroom and surrounding areas in South Africa via different routes, such as active contact via field workers, access through the workplace and advertisements by means of radio and local newspapers. Participants who are recruited firstly undergo screening to determine eligibility for participation in the African-PREDICT study. The participants therefore constitute a convenience or availability sample, stratified into different ethnic (black and white), sex and socio-economic class groups (low, mid, high). Of the 642 participants screened, n=403 (63%) were eligible and took part in the primary project.
Young (20–30 years of age), apparently healthy, black and white men and women, with normal clinic BP (that is, <140/90 mm Hg), no known CVD, not on any BP medication, no chronic disease (or treatment thereof), HIV-free, tuberculosis-free and not pregnant or breast feeding were recruited from the Potchefstroom area (in the North-West Province of South Africa).
Screening for eligibility of participation in African-PREDICT
Eligibility criteria, based on HIV status and BP, were assessed during a screening session that took place on a separate day, before the primary project day. HIV testing was performed using the South African Provider Initiated Counseling and Testing protocols, by trained counselors. HIV status was determined with the ABON HIV 1/2/O Tri-Line Rapid Test (ABON Biopharm, Hangzhou, China) using whole blood. If positive, the test was repeated with a First Response (PMC Medical, Nani Daman, India) rapid HIV test. If positive, participants were not eligible for the study.
BP eligibility was determined by BP measurement twice on each arm with a 5-min rest period between measurements, using a semi-automatic BP device (M3W-HEM7202, OMRON Healthcare, Kyoto, Japan) and appropriate sized BP cuffs. If the mean of four readings was >140 mm Hg and/or 90 mm Hg, participants were not eligible to continue through to the primary African-PREDICT project. All screening measurements and primary project day measurements took place in the morning.
African-PREDICT primary project data collection
Anthropometric and physical activity measurements
Weight (kg) was measured to the nearest 0.01 kg (SECA electronic scales, SECA, Birmingham, UK), height (m) was measured to the nearest 0.1 cm (SECA stadiometer, SECA) and waist circumference (cm) was measured in triplicate using a non-flexible tape measure (Holtain, Crymych, UK), and recorded to the nearest 0.1 cm. The median of the three recordings was used in subsequent analyses. Trained anthropometrists conducted these measurements. Body mass index was calculated using the standard weight (kg)/height (m2) calculation, and waist-to-height ratio was calculated using waist circumference (cm)/height (cm).
The combined heart rate (HR) and accelerometer ActiHeart (CamNtech, Cambridge, UK) device is a small, compact and non-invasive device that was worn on the chest by each participant for a period of 7 consecutive days, collecting data at 60 s epochs. The device was used in order to objectively capture Activity Energy Expenditure, an estimate of physical activity.
Cardiovascular measurements
With participants seated, clinic BP recordings were measured at the brachial artery, twice on each arm (DINAMAP, GE Healthcare, Buckinghamshire, UK), and a mean of the four readings was then used for all subsequent analyses. There was a 5-min rest period between each measurement, and appropriate sized BP cuffs were used.
We used validated CardioXplore devices (CardioXplore, MediTech, Budapest, Hungary) for collection of 24-h BP measurements, programmed to take recordings every 30 min during the day (0600 to 2200 hours) and every hour during the night (2200 to 0600 hours). The ABPM was fitted to each participant at approximately the same time every day (late morning), using an appropriate sized cuff, and as per the manufacturer’s instructions. Only participants with >70% of valid BP measurements, >20 day measurements and >7 night measurements were included in the final analyses.26
Both AIx and aPWV measurements were conducted using the SphygmoCor XCEL device (SphygmoCor XCEL, AtCor Medical, Sydney, Australia).27 AIx was captured at the brachial artery pulse point using a brachial pressure cuff, and calculated using software-in-built pulse wave analysis. aPWV was captured at the femoral and carotid arterial pulse points. The femoral artery wave form was captured via an appropriate sized cuff placed around the thigh, and the carotid arterial waveform was captured simultaneously via applanation tonometry. The SphygmoCor XCEL device also produced a central arterial waveform that provided an estimated central systolic BP reading, obtained from the peripheral arterial wave form via the in-built generalized transfer function.28
Biochemical measurements
Fasted venous blood samples were collected from the brachial antecubital vein into serum SST tubes (γ-glutamyl transpeptidase (GGT), cotinine, lipids, insulin, I-CAM, V-CAM, IL-6, CRP, TNF-α and ROS), EDTA plasma tubes (MCP-1) and sodium fluoride plasma tubes (glucose). We conducted analyses for low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol, triglycerides, glucose, high-sensitivity CRP and GGT (Cobas Integra 400plus, Roche, Basel, Switzerland). Cotinine (chemiluminescence method on the Immulite (Siemens, Erlangen, Germany)) and insulin (electrochemiluminescence method on the e411 (Roche)) were also assayed. I-CAM, V-CAM, MCP-1, high-sensitivity TNF-α and high-sensitivity IL-6 were assayed using Quantikine ELISA kits (R&D systems, Minneapolis, MN, USA). Serum peroxides as indication of ROS were determined by an improved assay system based on the principle of the derivatives of reactive oxygen metabolites test, which is recognized as an efficient method for evaluating oxidative stress in the body. This spectrophotometric method was performed on a Synergy H4 hybrid microplate reader (BioTek, Winooski, VT, USA). ROS levels are presented in Units, where 1.0 mg l−1 H2O2 represents one unit of ROS.29
Statistical analysis
We categorized participants according to their BP status. Based on normotensive screening BP n=403 participants were recruited onto the African-PREDICT project, with n=7 excluded as they did not have valid ABPM measurements, leaving n=396. We included n=352 in the current statistical analyses. The remaining 44 were excluded as on the primary project day they had elevated clinic BP; that is, they were identified as ‘true hypertensive’ (n=28) or ‘white coat hypertensive’ (n=16). These two cohorts were not included in further analyses as the size of the cohorts was deemed too small. See Table 1 for details.
The remaining participants were categorized as normotensive or MHT. Normotensive status was based on having a normal clinic BP (that is, <140 mm Hg systolic BP, and<90 mm Hg diastolic BP) and normal ABPM (that is, 24-h readings <130 and<80 mm Hg, daytime readings <135 and<85 mm Hg and night time readings <120 and<70 mm Hg). MHT status was classified as participants having normal clinic BP (<140 and <90 mm Hg), but an elevated ABPM (24-h SBP and/or DBP⩾130/80 mm Hg; day SBP and/or DBP⩾135/85 mm Hg; night SBP and/or DBP⩾120/70 mm Hg). MHT was classified as being hypertensive either at 24-h, and/or day, and/or night.26
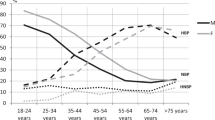
Statistical analyses were conducted using SPSS version 22 (IBM, Armonk, NY, USA). χ2 analyses were conducted for categorical data, whereas independent samples t-test, and analysis of covariance analyses were used for analysis of continuous data. Normality of variables was tested using the Shapiro–Wilk test and visual inspection of histogram plots. Normally distributed data are expressed as the arithmetic mean and standard deviation. Skewed data were log transformed and the geometric mean and 5th and 95th percentiles are displayed (Tables 3 and 4). Adjusted odds ratio analyses were conducted, and data displayed in forest plots (Figure 1). As the study sample represents a young, healthy population, we were unable to use clinical cutoff values for odds ratio analyses as changes in pressure, stiffness and endothelial function are expected to be early sub-clinical changes for those at increased risk. Cutoff values used for the odds ratios were therefore determined as median splits of the cohort as a whole.
Adjusted odds ratios for having adverse central systolic blood pressure (cSBP), arterial stiffness and biochemical markers of cardiovascular risk in individuals with masked hypertension. Adjusted for age, sex, ethnicity, waist circumference, γ-glutamyl transpeptidase, cotinine and physical activity levels (augmentation index (AIx) additionally adjusted for height, aPWV additionally adjusted for MAP), n=352. aPWV, aortic pulse wave velocity; CRP, C-reactive protein; I-CAM, intracellular adhesion molecule; IL-6, interleukin-6; MCP-1, monocyte chemoattractant protein; ROS, reactive oxygen species; TNF-α, tumor necrosis factor-α; V-CAM, vascular cellular adhesion molecule.
Results
As indicated in Table 1, of the 352 participants included in our analyses, n=290 (82.4%) were normotensive by clinic BP and by 24-h BP and n=62 (17.6%) had MHT.
Table 2 demonstrates on which criteria participants were classified as MHT, indicating that the majority of classifications were based on hypertensive nighttime readings alone (52%), and that 24% were MHT according to all times (nighttime, daytime and 24-h).
In Table 3, we compared the profiles of the normotensive and MHT status groups. Although age and ethnicity did not differ between the groups, the MHT group consisted of significantly more men than the normotensive group (67.7% vs. 33.8%). The level of completed education between the two groups did not statistically differ; the majority in both groups having attained a college/university level of education. MHT participants were taller, had increased adiposity, higher clinic BP, 24-h BP and central BP, and aPWV (6.58 vs. 6.24 m s−1; all P⩽0.001). With regards to biochemical markers of cardiovascular risk, high-density lipoprotein-cholesterol was lower (1.17 vs. 1.38 mmol l−1), and triglycerides (1.2 vs 0.92 mmol l−1), glucose (4.62 vs. 4.30 mmol l−1), insulin (12.77 vs. 10.13 uU ml−1), MCP-1 (175 vs. 152 pg ml−1) and I-CAM (185 vs. 161 ng ml−1) were higher in the MHT group (all P<0.05). GGT was higher in the MHT group, but there were no significant differences in physical activity or cotinine levels between the groups.
We repeated these analyses in Table 4, with outcome variables adjusted for age, sex, ethnicity, waist circumference, GGT, cotinine and activity energy expenditure. Following these adjustments, elevated levels for adiposity; BPs and aPWV (6.54 vs. 6.26 m s−1, P=0.020) were confirmed in the MHT group compared with the normotensive group. Twenty-four- hour HR (79 vs. 75 b.p.m.) was also higher in the MHT group compared with the normotensive group. Following adjustments, MCP-1 (172 vs 153 pg ml−1) was higher in the MHT group (P=0.009), whereas AIx (9.26% vs. 7.24%, P=0.053) and V-CAM (604 vs. 560 ng ml−1) tended to be higher in the MHT group (P=0.054).
Figure 1 displays the results of adjusted odds ratios for the likelihood of having increased central systolic BP, arterial stiffness or biochemical markers of cardiovascular risk in MHT. When compared with the normotensive group, participants with MHT had increased odds for having elevated central systolic BP (1.537, 95% confidence interval (CI)=1.089–2.171), aPWV (1.567, 95% CI=1.115–2.202), insulin (1.443, 95% CI=1.005–2.101), MCP-1 (1.499, 95% CI=1.049–2.141), V-CAM (1.409, 95% CI=1.012–1.962) and CRP (1.440, 95% CI=1.009–2.054).
Discussion
Participants were primarily included in the African-PREDICT project based on their normotensive BP measurements at the screening stage of the project (that is, <140/90 mm Hg). It was therefore noteworthy to detect that almost 18% of this apparently healthy, black and white, 20- to 30-year-old cohort were hypertensive when assessed via ambulatory BP measurements, a condition termed MHT. The occurrence of MHT in our young cohort supports evidence that proposes that the prevalence of MHT is between 8 and 30% in populations classified as normotensive by clinic BP readings.11, 30 This population would not have been identified as hypertensive in the current study if clinic BP solely had been assessed, and therefore would be unaware of being at increased risk of CVD development.
Andrikou et al.31 have also previously demonstrated increased CRP and PWV levels in MHT participants compared with normotensives. Also, increased aPWV was observed in MHT of an 18- to 80-year-old age group32 and brachial-ankle PWV was increased in a type-2 diabetic cohort.33 Further MHT has been associated with inflammation, endothelial dysfunction, diabetes, chronic kidney disease, obstructive sleep apnea, increased physical activity, mental stress, smoking and alcohol consumption.11 However, cardiovascular risk factors associated with MHT in young, otherwise healthy adults have been poorly explored, also in sub-Saharan Africa.
Despite the screening and clinic BP values for both groups being in the normotensive range, the masked hypertensives of the current study displayed higher BPs in all methods of measurement, namely, screening-, clinic-, ambulatory- and central systolic-BP, when compared with normotensives. Furthermore, adjusted odds ratios demonstrated that MHT was associated with increased risk for elevated levels of central systolic pressure, and also insulin. MHT was additionally associated with increased adiposity, as determined via body mass index, waist circumference and waist-to-height ratio, confirming findings from a Japanese population that demonstrated that waist circumference, body mass index and waist-to-hip ratio were all significant predictors of MHT.34 We also observed an elevated 24-h HR in the MHT group, suggesting increased sympathetic nervous system activity, which may contribute to obesity-related hypertension.35 Therefore, it is plausible that the observed increased adiposity in the MHT group may be associated with the development of MHT, potentially by regulation of insulin-36 and HR-associated increases in sympathetic activation.35 This is further supported by the observation that the majority of participants (52%) were categorized as MHT by their nighttime ABPM alone.37
Following adjustment for a number of potential confounders, large artery stiffness was higher in the MHT group compared with the normotensive group. Increased aPWV (independent of differences in MAP) in the MHT group suggests that early vascular remodeling has occurred, in which reduced elasticity of the arterial wall may have led to increased stiffness of the aorta. AIx (a surrogate marker of arterial stiffness) also tended to be higher in the MHT group (P=0.053), thus suggesting augmented late central systolic pressure as a result of late return of the reflected wave because of increased stiffness of the artery. aPWV and AIx are both associated with increased morbidity and mortality15, 38, 39, 40, 41 and are associated with the presence of other cardiovascular risk factors.42, 43, 44
As AIx is considered as a measure of global endothelial function,45 we expected that markers of endothelial activation would also be elevated with MHT. Indeed, a prominent finding of our study was the elevated circulating levels of MCP-1 in MHT. Similarly, another marker of endothelial activation, V-CAM, also tended to be higher in the MHT group (P=0.054). Furthermore, odds ratio analyses demonstrated that MHT was associated with increased risk for elevated levels of these two markers. Both factors activate the endothelium by promoting monocyte adhesion to the endothelial wall, and therefore facilitate the development of atherosclerosis.46, 47, 48, 49
On top of the findings that MHT was associated with arterial stiffness and endothelial activation, we also found an increased odds for inflammation (CRP). Although CRP is an accepted index of overall inflammatory activity, the lack of difference in the inflammatory markers between the two groups may suggest that at this early stage of MHT development (young adults), inflammation may have a lesser role than endothelial activation. This may be supported by a study conducted in an older (40–75 years), sedentary, pre-hypertensive African-American MHT cohort, where increased CRP levels were observed when compared with a ‘true pre-hypertensive’ control group (n=17).50
The physiological mechanisms explaining the development of MHT are not well understood. Pickering et al.3 hypothesized that that those with higher ABPM readings may be more physically active than those presenting as truly normotensive, however, we controlled for 7-day physical activity levels, and also found no difference between the two groups. Similarly, Mann et al.51 suggested that smoking raises daytime ABPM readings, however, we controlled for cotinine levels, which should eradicate this effect, and also, cotinine levels did not differ between our two groups.
In this young adult population, a noteworthy contribution of our findings relates to those measures that were similar between the normotensive and MHT participants, namely serum lipids, glucose, the majority of inflammatory markers (IL-6, TNF-α), ROS, smoking behavior and physical activity levels. Our data suggest that these markers may not be useful markers in the prediction of MHT in this population, although this may be different in older populations. The current study demonstrated that MHT is associated with increased cardiovascular risk on a vascular level, which was specifically evidenced by increased endothelial activation and arterial stiffness. This increase in cardiovascular risk was also associated with increased adiposity. However, cause and effect cannot be established using our evidence because of the cross-sectional nature of the study, and therefore whether increased endothelial activation occurs before the development of MHT cannot be clarified.
In clinical practice in high-income countries, ABPM is typically conducted only in those who present as hypertensive in clinic, making the diagnosis of MHT difficult. A further contributing factor to the difficulty in MHT diagnosis is that in low- and middle-income countries ABPM is rarely used. Our study highlights the high prevalence of MHT occurring in young, seemingly healthy adults (We furthermore found no ethnic-specific difference in MHT frequency in young black and white individuals.). Effective methods of diagnosing MHT are vital, which will allow MHT patients to commence with the required pharmaceutical and lifestyle interventions. The ability to routinely detect MHT early in life would have a substantial beneficial impact by reducing the significant global economic burden posed by CVD development.
It is therefore important to devise a feasible method of diagnosing MHT. Fitting every individual with an ABPM device is not viable in low resource settings, but our findings support previous results52, 53 that MHT participants consistently have clinic SBP above 120 mm Hg. Therefore, for participants presenting in clinic with SBP⩾120 mm Hg together with other hypertension risk factors (for example, obesity,53 and family history of hypertension), ABPM is likely to be cost-effective. Although this remains unlikely in low- and middle-income countries, it may be more feasible than suggesting that clinics measure ABPM on all patients presenting with SBP greater than 120 mm Hg. Further to this, in low- and middle-income countries, home BP monitoring may be more viable than ABPM should low-cost validated devices be available. In the first instance, it is important to raise awareness of the phenomenon of MHT, as many medical and health practitioners may be unaware of its existence.
With regard to investigating MHT, a limitation of the current study is that we specifically recruited apparently healthy, young adults and therefore the data are not generalizable to all South African adults. Further, the study was cross-sectional and therefore causality cannot be inferred. However, the African-PREDICT project is longitudinal in design, and therefore the opportunity to later assess how MHT at baseline relates to aging and future CVD does exist. Another limitation is the limited reproducibility of ABPM, as most recently demonstrated by Keren et al.54 who demonstrated only a moderate correlation between ABPM measurements taken 14 weeks apart. To ensure the most accurate ABPM measurements in the current study, participants were familiarized with the clinic setting on a previous screening day. All operators of the ABPM were trained to fit the ABPM devices using an identical protocol.
In conclusion, we found that MHT was common (18%) in young, apparently healthy, black and white South Africans. This percentage may grossly underestimate population prevalence and is not generalizable to the whole South African population as the current data are based on apparently healthy participants younger than 30 years. However, a review conducted by Gorostidi et al.53 demonstrated that MHT patients are more likely to be young. We found that MHT was associated with elevated cardiovascular risk, evidenced by increased adiposity, central pressure, large artery stiffness and endothelial activation. Our findings highlight the importance of early and accurate detection of MHT as a means of reducing the incidence of CVD, thereby reducing its global economic and social burden. Further studies are required in order to determine the most cost-effective method of identifying undiagnosed MHT cases, particularly in Africa.
References
World Health Organisation Cardiovascular Diseases 2013 [updated on January 2015; cited on 13 April 2015]. Available from http://www.who.int/mediacentre/factsheets/fs317/en/index.html.
Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S . Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol 2014; 43: 116–128.
Pickering TG, Davidson K, Gerin W, Schwartz JE . Masked hypertension. Hypertension 2002; 40: 795–796.
O'Brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P . Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005; 23: 697–701.
McKay DW, Myers MG, Bolli P, Chockalingam A . Masked hypertension: a common but insidious presentation of hypertension. Can J Cardiol 2006; 22: 617–620.
Papadopoulos DP, Makris TK . Masked hypertension definition, impact, outcomes: a critical review. J Clin Hypertens (Greenwich) 2007; 9: 956–963.
Pickering TG . White coat hypertension: time for action. Circulation 1998; 98: 1834–1836.
Pickering TG, Eguchi K, Kario K . Masked hypertension: a review. Hypertens Res 2007; 30: 479–488.
Longo D, Dorigatti F, Palatini P . Masked hypertension in adults. Blood Press Monit 2005; 10: 307–310.
Angeli F, Reboldi G, Verdecchia P . Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens 2010; 23: 941–948.
Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D . Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens 2014; 28: 521–528.
Boggia J, Silvarino R, Luzardo L, Noboa O . Significance of white-coat and masked hypertension in chronic kidney disease and end-stage renal disease. Hypertens Res 2014; 37: 882–889.
Cha R-h Kim S, Ae Yoon S, Ryu D-R, Eun Oh J, Han S-Y, Young Lee E, Ki Kim D, Kim YS . Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study. Hypertens Res 2014; 37: 172–178.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, Laurent S . Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension 2002; 39: 10–15.
Mattace-Raso FUS, van der Cammen TJM, Hofman A, van Popele NM, Bos ML, Schalekamp MADH, Asmar R, Reneman RS, Hoeks APG, Breteler MMB, Witteman JCM . Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam study. Circulation 2006; 113: 657–663.
Nurnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schafers RF . Augmentation index is associated with cardiovascular risk. J Hypertens 2002; 20: 2407–2414.
Yasmin, McEniery CM, Wallace S, Mackenzie IS, Cockcroft JR, Wilkinson IB . C-Reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol 2004; 24: 969–974.
Ridker PM, Rifai N, Rose L, Buring JE, Cook NR . Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med 2002; 347: 1557–1565.
de Lemos JA, Morrow DA, Sabatine MS, Murphy SA, Gibson CM, Antman EM, McCabe CH, Cannon CP, Braunwald E . Association between plasma levels of monocyte chemoattractant protein-1 and long-term clinical outcomes in patients with acute coronary syndromes. Circulation 2003; 107: 690–695.
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH . Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997; 336: 973–979.
Ridker PM, Hennekens CH, Roitman-Johnson B, Stampfer MJ, Allen J . Plasma concentration of soluble intercellular adhesion molecule 1 and risks of future myocardial infarction in apparently healthy men. Lancet 1998; 351: 88–92.
Hwang SJ, Ballantyne CM, Sharrett AR, Smith LC, Davis CE, Gotto AM Jr., Boerwinkle E . Circulating adhesion molecules VCAM-1, ICAM-1, and E-selectin in carotid atherosclerosis and incident coronary heart disease cases: the Atherosclerosis Risk In Communities (ARIC) study. Circulation 1997; 96: 4219–4225.
Blankenberg S, Rupprecht HJ, Bickel C, Peetz D, Hafner G, Tiret L, Meyer J . Circulating cell adhesion molecules and death in patients with coronary artery disease. Circulation 2001; 104: 1336–1342.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion J-M, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y . European Society of Hypertension Position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31: 1731–1768.
Hwang MH, Yoo JK, Kim HK, Hwang CL, Mackay K, Hemstreet O, Nichols WW, Christou DD . Validity and reliability of aortic pulse wave velocity and augmentation index determined by the new cuff-based SphygmoCor Xcel. J Hum Hypertens 2014; 28: 475–481.
Pauca AL, O’Rourke MF, Kon ND . Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension 2001; 38: 932–937.
Hayashi I, Morishita Y, Imai K, Nakamura M, Nakachi K, Hayashi T . High-throughput spectrophotometric assay of reactive oxygen species in serum. Mutat Res 2007; 631: 55–61.
Bobrie G, Clerson P, Ménard J, Postel-Vinay N, Chatellier G, Plouin P-F . Masked hypertension: a systematic review. J Hypertens 2008; 26: 1715–1725.
Andrikou I, Tsioufis C, Dimitriadis K, Syrseloudis D, Valenti P, Almiroudi M, Lioni L, Tousoulis D, Stefanadis C . Similar levels of low-grade inflammation and arterial stiffness in masked and white-coat hypertension: comparisons with sustained hypertension and normotension. Blood Press Monit 2011; 16: 218–223.
Silva JA, Barbosa L, Bertoquini S, Maldonado J, Polonia J . Relationship between aortic stiffness and cardiovascular risk factors in a population of normotensives, white-coat normotensives, white-coat hypertensives, sustained hypertensives and diabetic patients. Rev Port Cardiol 2004; 23: 1533–1547.
Takeno K, Mita T, Nakayama S, Goto H, Komiya K, Abe H, Ikeda F, Shimizu T, Kanazawa A, Hirose T, Kawamori R, Watada H . Masked hypertension, endothelial dysfunction, and arterial stiffness in type 2 diabetes mellitus: a pilot study. Am J Hypertens 2012; 25: 165–170.
Asayama K, Sato A, Ohkubo T, Mimura A, Hayashi K, Kikuya M, Yasui D, Kanno A, Hara A, Hirose T, Obara T, Metoki H, Inoue R, Hoshi H, Satoh H, Imai Y . The association between masked hypertension and waist circumference as an obesity-related anthropometric index for metabolic syndrome: the Ohasama study. Hypertens Res 2009; 32: 438–443.
Kalil GZ, Haynes WG . Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens Res 2012; 35: 4–16.
Anderson EA, Hoffman R, Balon T, Sinkey C, Mark A . Hyperinsulinemia produces both sympathetic neural activation and vasodilation in normal humans. J Clin Invest 1991; 87: 2246.
Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL . Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens 2002; 15: 111–118.
Blacher J, Asmar R, Djane S, London GM, Safar ME . Aortic Pulse Wave Velocity as a Marker of Cardiovascular Risk in Hypertensive Patients. Hypertension 1999; 33: 1111–1117.
Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, Havlik R, Lakatta EG, Spurgeon H, Kritchevsky S, Pahor M, Bauer D, Newman A . Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390.
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318–1327.
London GM, Blacher J, Pannier B, Guérin AP, Marchais SJ, Safar ME . Arterial wave reflections and survival in end-stage renal failure. Hypertension 2001; 38: 434–438.
O'Rourke MF, Staessen JA, Vlachopoulos C, Duprez D, Plante Ge E . Clinical applications of arterial stiffness; definitions and reference values. Am J Hypertens 2002; 15: 426–444.
Laurent S, Cockroft J, Bortel LV, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
McEniery CM, Cockcroft JR . Does arterial stiffness predict atherosclerotic coronary events? Adv Cardiol 2007; 44: 160–172.
Hayward CS, Kraidly M, Webb CM, Collins P . Assessment of endothelial function using peripheral waveform analysis: a clinical application. J Am Coll Cardiol 2002; 40: 521–528.
Niu J, Kolattukudy P . Role of MCP-1 in cardiovascular disease: molecular mechanisms and clinical implications. Clin Sci 2009; 117: 95–109.
Cybulsky MI, Iiyama K, Li H, Zhu S, Chen M, Iiyama M, Davis V, Gutierrez-Ramos JC, Connelly PW, Milstone DS . A major role for VCAM-1, but not ICAM-1, in early atherosclerosis. J Clin Invest 2001; 107: 1255–1262.
Libby P . Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr 2006; 83: 456S–460SS.
Cook-Mills JM, Marchese ME, Abdala-Valencia H . Vascular cell adhesion molecule-1 expression and signaling during disease: regulation by reactive oxygen species and antioxidants. Antioxid Redox Signal 2011; 15: 1607–1638.
Veerabhadrappa P, Diaz KM, Feairheller DL, Sturgeon KM, Williamson ST, Crabbe DL, Kashem AM, Brown MD . Endothelial-dependent flow-mediated dilation in African Americans with masked-hypertension. Am J Hypertens 2011; 24: 1102–1107.
Mann SJ, James GD, Wang RS, Pickering TG . Elevation of ambulatory systolic blood pressure in hypertensive smokers. A case-control study. JAMA 1991; 265: 2226–2228.
Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB . Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med 1999; 131: 564–572.
Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A . Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res 2015; 38: 1–7.
Keren S, Leibowitz A, Grossman E, Sharabi Y . Limited reproducibility of 24-h ambulatory blood pressure monitoring. Clin Exp Hypertens 2015; 37: 599–603.
Acknowledgements
We are grateful toward all individuals voluntarily participating in the study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University is also duly acknowledged. We further thank research support from the research entity, Physical Activity Sport and Recreation (PhASRec) at the North-West University, for the collection and analysis of the physical activity data. The research project was financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation of South Africa; as well as corporate social investment grants from Pfizer (South Africa), Boehringer Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in-kind contributions of Roche Diagnostics (SA). Any opinion, findings and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in this regard.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Thompson, J., Smith, W., Ware, L. et al. Masked hypertension and its associated cardiovascular risk in young individuals: the African-PREDICT study. Hypertens Res 39, 158–165 (2016). https://doi.org/10.1038/hr.2015.123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.123
Keywords
This article is cited by
-
Identifying a metabolomics profile associated with masked hypertension in two independent cohorts: Data from the African-PREDICT and SABPA studies
Hypertension Research (2022)
-
Contribution of single office aortic systolic blood pressure measurements to the detection of masked hypertension: data from two separate cohorts
Hypertension Research (2021)
-
Healthy aging and carotid performance: strain measures and β-stiffness index
Hypertension Research (2018)
-
Microcirculation and biomarkers in patients with resistant or mild-to-moderate hypertension: a cross-sectional study
Hypertension Research (2018)
-
Recent advances in understanding hypertension development in sub-Saharan Africa
Journal of Human Hypertension (2017)