Abstract
This study investigated the association between hemodynamic variables and the 6-minute walk distance (6MWD) in adults with and without hypertension and explored the role of hemodynamic variables as predictors of 6MWD. Patients undergoing antihypertensive medication therapy (n=41) and sex-matched healthy subjects (n=41) were evaluated for their clinical status and cardiovascular risk factors. Two 6-minute walk tests were performed along an 18-m corridor with a 30-minute rest interval. The intraclass correlation (ICC) was high among patients (ICC=0.984 (0.965; 0.992), P<0.001) and controls (ICC=0.987 (0.832; 0.996), P<0.001). The patients presented 6MWD values that were significantly lower than those of healthy controls (338.8±112.8 vs. 388.0±66.7 m, P=0.010). In patients, the 6MWD was significantly and positively correlated with sex (0.737; P<0.001), height (0.502; P<0.001) and weight (0.303; P=0.027). In addition, negative and significant correlations were observed between 6MWD and the mean (−0.577; P<0.001), systolic (−0.521; P<0.001), diastolic (−0.505; P=0.001) and pulse (−0.353; P=0.015) pressures after simultaneous adjustment for age, body height and weight. The same behavior was observed in healthy controls (except for pulse pressure), albeit with lower correlation values. A regression model with sex, age, height and weight explained 52.2% (P<0.001) of the variance. The highest explained variance in patients (64.8%; P<0.001) and controls (56.5%; P<0.001) was observed after replacing the body weight with mean pressure in the model. The 6MWD is inversely associated with hemodynamic variables in both groups and is lower in patients with hypertension compared with healthy controls. Hemodynamic variables, particularly the mean pressure, should be included in prediction equations for 6MWD.
Similar content being viewed by others
Introduction
Hypertension is the leading risk factor for cardiovascular diseases (CVDs) and a major public health problem worldwide1 and in Brazil. Despite a 6% reduction over the past three decades,2 the prevalence of hypertension in Brazil is still nearly 30%. The cardiovascular risk for adverse outcomes increases continuously with blood pressure values that exceed optimum levels.3, 4 Hypertension is related to structural and functional changes in small-, middle- and large-sized arteries that may progress to damage of target organs, such as the heart, brain and kidneys.5 Microvascular arterial remodeling also occurs in the skeletal muscles of untreated adults with hypertension.6 Such damage compromises the functional capacity and long-term independence in activities of daily living, such that patients with hypertension are at high risk of developing physical disabilities.7 Because cardiac rehabilitation aims to interrupt the mutual reinforcement between high blood pressure and its underlying mechanisms, the early recognition of functional impairments in patients with hypertension may allow for immediate intervention to prevent more severe disabilities.
As its first use in patients undergoing cardiac rehabilitation,8 the six-minute walk test (6MWT) has been considered as a valid and reliable method in the assessment of functional capacity in outpatients.9, 10, 11 The 6MWT evolved from other timed walk tests12, 13 and is preferred to other methods for the assessment of functional capacity because it is safe, well tolerated by patients, easy to perform, inexpensive and similar to daily-living activities.14 This test’s main outcome—the six-minute walk distance (6MWD)—is analyzed either as an absolute or percent value based on reference equations obtained from healthy subjects. Despite the number of published equations for the adult population,15 the use of equations from national samples is advocated as 6MWT results have been demonstrated to be region-dependent.16
Literature on the 6MWT in patients with hypertension is limited. Clinical trials have reported low absolute values of the 6MWD in adults with grade-I or -II hypertension and comorbidities, which improved after physical rehabilitation programs.17, 18, 19 Cross-sectional studies have suggested diminished 6MWD in women with grade-I hypertension with comorbidities,20 whereas another cross-sectional study21 demonstrated preserved 6MWD in men with grade-I hypertension without comorbidities along with a significant 8% overestimation of the predicted distance using a foreign equation.22 The 6MWD is correlated with other functional outcomes such as the ‘Timed Up and Go’ test in women with hypertension and comorbidities.23 However, these observations were derived from small samples with specific characteristics and thus were subject to spectrum bias, resulting in limited external validity.24
The goodness-of-fit (R2) of Brazilian prediction equations25, 26, 27 based on personal variables (age, sex, body height and weight) ranges from 30 to 60%. Such low values suggest that other important variables should be considered as predictors of 6MWD. Because some factors associated with the 6MWD in healthy subjects are also risk factors for CVD—that is, sex, age, weight and height28, 29, 30, 31—it is hypothesized that other factors related to the pathophysiology of hypertension may contribute to a better prediction of the 6MWD in this population. Notably, the association between 6MWD and hemodynamic variables in adults with and without hypertension remains unknown, as well as their potential role as predictors of 6MWD. Therefore, the aims of this study are twofold: (1) to test the association between hemodynamic variables and the 6MWD in adults with hypertension; and (2) to explore the role of hemodynamic variables as predictors of the 6MWD to be included in a population-specific equation.
Methods
Ethics
The Institutional Ethics Committee approved this study protocol before execution (CAAE 05517012.8.0000.5235). All subjects signed an informed consent form after being informed of the study aims and procedures.
Study design and sample size
This was a sex-matched, case–control study. The examiner was not blinded to the participants’ group as the 6MWD outcome is not likely to be influenced by this information. Considering the association between the 6MWD and hemodynamic variables as the main outcome of this study, a minimal sample size of 36 participants per group was necessary to observe a minimal correlation of 0.41 (weak or higher) at a 5% significance level and 80% study power.
Participants
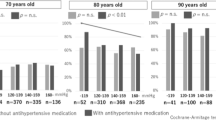
Table 1 summarizes the sample group’s descriptive data. Forty-one patients undergoing routine antihypertensive medication therapy were consecutively assessed for eligibility from December 2012 to June 2013 at the Division of Arterial Hypertension of the National Institute of Cardiology (RJ, Brazil). Forty-one healthy subjects were also assessed for eligibility among the patient’s relatives and individuals who accompanied the patients during the clinical visits (Figure 1). Eligibility was considered depending on the following inclusion criteria: age >18 years; no physical limitations that influence walking; and no recent history (<6 months) of musculoskeletal pain in the lower limbs and spine. The following additional criteria were applied for patients: an established diagnosis of primary systemic arterial hypertension before the study (systolic pressure (SP) ⩾140 mm Hg and/or diastolic pressure (DP) ⩾90 mm Hg on repeat visits);5 completion of biochemical blood analysis; and the absence of valvular disease, ventricular dysfunction and cardiac arrhythmias.
History, physical examination and laboratory analysis
The patient’s clinical histories were obtained and they underwent anamnesis and physical examination for the assessment of their personal characteristics after a 10-minute rest in the sitting position. The same examiner performed all of the assessments in a temperature-controlled room (21–23 °C) during the morning (0800—1100 h) and in the presence of a physician.
Information about the self-reported duration of hypertension, smoking habits, history of premature CVD (men <55 years, women <65 years)5 and physical activity level32, 33 were collected. Body height and weight were obtained using an analog scale and rounded to the closest decimal value; these values were used to calculate the Quetelet’s body mass index. The heart rate (HR), SP and DP were measured in the office using an oscillometric-automated device positioned at the right-sided wrist (model BP3AF1-3; Onbo Electronic, Bao An Shin, Shenzen, China). The participant was allowed to rest for 5–10 min in a seated position before three repeat blood pressure measurements were obtained, spaced by a 1–2 min interval.5 Both SP and DP were used to calculate the pulse pressure (PP=SP−DP) and mean arterial pressure (MP=DP+PP/3). All arterial pressure measurements were reported as the average of the three measurements. Laboratory biochemical analyses for the assessment of cardiovascular risk factors were performed in the fasting state and included serum creatinine, serum glucose, uric acid, total triglycerides, total cholesterol, low-density lipoprotein, high-density lipoprotein and C-reactive protein (CRP).
The hypertension grade was determined according to the average of the office blood pressure values obtained during screening.5 The additional cardiovascular risk factors that were assessed included: obesity (body mass index ⩾30 kg m−2);34 sedentary lifestyle (IQPA: sedentary or irregularly active during the prior month); dyslipidemia (low-density lipoprotein-cholesterol <100 mg dl−1 for controls or <70 mg dl−1 for cases, high-density lipoprotein-cholesterol >50 mg dl−1 and triglycerides >150 mg dl−1, according to the American Diabetes Association, 2013); and diabetes mellitus (fasting serum glucose >126 mg dl−1).
Functional capacity: the 6MWT
The 6MWT was performed according to the general published recommendations,35 with minor adaptations.21 Before the 6MWT, subjects were requested to not engage in physical activities for 24 h and to not smoke or ingest alcohol for at least 3 h. All 6MWT were performed outdoors along an 18-m corridor delimited with cones at both ends.
All subjects were instructed to walk as fast as they could along the corridor. They were also informed to slow down their walk or to interrupt it if necessary. During all tests, the participants were monitored verbally by the Borg modified scale every 2 min. For the duration of the test, the examiner did not use incentive phrases, although the participants were informed about the test duration 3 min after its start (‘Three minutes left!’). By the sixth minute, each subject was requested to stop and the number of runs and the remaining distance of the last run were summed. The blood pressure and HR were measured before the test, and during the first and sixth minute after finishing the test in the sitting position. Two tests were performed with a 30-minute interval, and the average of the two 6MWD values was used to best approximate a representative true value.36 The post-test hemodynamic variables used for the analyses corresponded to the ‘best effort’ 6MWT.
The 6MWD absolute values were provided with their percent values predicted using three equations derived from Brazilian samples.25, 26, 27 The maximal HR was predicted using a regression equation for adults.37
Statistical analysis
Continuous and ordinal variables were described as the mean±s.d. or median (minimum; maximum), whereas nominal variables were represented by n (%). Normality of distributions was evaluated using the Kolmogorov–Smirnov test. Continuous variables were compared between and within groups by the one-tailed Student’s t-test and paired t-test, respectively. Categorical variables between groups were compared by the Z-test and were coded as dummy variables: sex (male=1, female=0) and risk factors for CVD (present=1; absent=0). The repeatability of the 6MWT was measured by the two-way random intraclass coefficient (ICC and 95% confidence interval) with absolute agreement. The hemodynamic variables that were evaluated pre- and post-6MWT (first and sixth minute) were compared through one-way analysis of variance (ANOVA) with Dunnett’s post hoc test (control: pre-6MWD). Bivariate associations were examined by one-tailed Pearson’s r correlation coefficient between 6MWD and hemodynamic variables. Partial correlations for hemodynamic variables were also estimated after controlling for possible confounding variables (age, height and weight). Several linear regression models were generated to explore the role of hemodynamic variables as predictors of absolute 6MWD. Each model was limited to four dependent variables because of the sample size (minimal ratio case: variable=10:1). A ‘reference’ model (no. 0) was created with variables most commonly used in 6MWD prediction equations (sex, age, height and weight).15 Four other models were generated with three fixed variables (sex, age and height) because of significant high correlations with the 6MWD plus a hemodynamic variable: SP, DP, MP or PP (nos. 1 to 4, respectively). The adjusted R2 and P-values were calculated to evaluate each model fit. Statistical significance was considered as P<0.05 with a 95% confidence interval. Analyses were conducted using SPSS 17 (SPSS, Chicago, IL, USA).
Results
Performance and repeatability of 6MWT
All participants completed the 6MWT without interruption. The intraclass correlation was high among patients (ICC=0.984 (0.965; 0.992), P<0.001) and controls (ICC=0.987 (0.832; 0.996), P<0.001).
Significantly lower 6MWD values were observed for the second test compared with the first in both groups of patients (344.6±112.2 vs. 331.1±115.0 m, P=0.005) and healthy controls (387.7±66.8 vs. 376.1±68.4 m, P<0.001), with greater variability in the former group (Table 2). The 6MWD was significantly lower in patients compared with healthy controls for the first and second tests (P=0.019 and 0.022, respectively). Patients presented an average 6MWD that was significantly lower than that of healthy controls (338.8±112.8 vs. 388.0±66.7 m, P=0.010).
All Brazilian equations overestimated the 6MWD (Table 2). Iwama’s equation yielded significantly lower predicted values for patients compared with healthy controls (59.9±16.6% vs. 65.5±9.0%, P=0.032), whereas no significant differences were observed for the 6MWD percent values, as predicted by the equations of Dourado et al.15 (53.2±15.2% vs. 55.7±7.4%, P=0.177) or Soares and Pereira27 (58.7±18.3% vs. 61.6±9.4%, P=0.184).
The hemodynamic variables SP, DP and HR exhibited significantly (all P<0.001) high values in both groups during the first minute after the test, and remained significantly high during the sixth minute despite a trend of reduction to pre-6MWT values (Table 2).
Association between 6MWD and other variables
In patients, the 6MWD was significantly and positively correlated with sex (0.737; P<0.001), height (0.502; P<0.001) and weight (0.303; P=0.027) (Table 3). Negative and significant correlations were observed between 6MWD and HR (−0.604; P<0.001), MP (−0.518; P<0.001), SP (−0.480; P=0.001), DP (−0.441; P=0.002), age (−0.383; P=0.007), duration of hypertension (−0.361; P=0.010) and PP (−0.341; P=0.015). The simultaneous adjustment for age, height and weight yielded, nevertheless, significant and stronger correlations between all hemodynamic variables and the 6MWD, except for HR, which presented a weaker yet significant correlation.
In healthy controls, the 6MWD was also significantly and positively correlated with sex (0.680; P<0.001), height (0.635; P<0.001) and weight (0.398; P=0.005). By contrast, the averaged 6MWD was negatively correlated to MP (−0.304; P<0.027), SP (−0.290; P=0.033) and DP (−0.269; P=0.044), but not to HR (−0.231; P=0.073), age (−0.147; P=0.180) or PP (−0.120; P=0.227). The simultaneous adjustment for age, height and weight yielded significant and stronger negative correlations between all hemodynamic variables and the 6MWD again, except for PP.
Prediction of the 6MWD using clinical and hemodynamic variables
The average 6MWD was significantly predicted by all models (nos. 0–4) (all P<0.001) in both groups (Table 4). In patients with hypertension, model no. 0 exhibited the lowest explained variance (52.2%). Replacing the body weight by PP, SP, DP or MP yielded progressively higher explained variances of 54.8%, 61.1%, 62.6% and 64.8%, respectively. Healthy controls exhibited a similar explained variance of model no. 0 (54.7%) compared with the patients with hypertension. Likewise, replacing the body weight by PP, SP, DP or MP yielded progressively higher explained variances of 51.2%, 54.8%, 56.1% and 56.5%, respectively.
Discussion
This study investigated the association between hemodynamic variables and the 6MWD in adults with and without hypertension, and explored the role of hemodynamic variables as predictors of the 6MWD for inclusion in a population-specific equation. The main outcomes of this study are: (1) the 6MWD is inversely associated to MP, SP, DP and PP both in patients with hypertension and in healthy controls; and (2) hemodynamic variables, mainly MP, improve the prediction of the 6MWD in both groups. This is the first study to explore the differences in the 6MWT between patients with hypertension and healthy subjects, as well as to confirm that hemodynamic variables can be used for the prediction of functional capacity.
The high repeatability between two tests in this study was an expected outcome as this has been previously reported for patients undergoing cardiac rehabilitation (ICC=0.96 (0.93; 0.98))38 and healthy subjects (ICC=0.84 for three 6MWT).39 However, a 3–4% reduction in the 6MWD in the second test was unanticipated because the second 6MWD usually increases by 3–5% in patients with CVD38 and in healthy subjects,39 allegedly due to the ‘learning effect’. Although a reduction of the 6MWD in sequential tests may suggest a low-effort test, this explanation is unlikely because the post-6MWT predicted an HR increase similar to other studies.25, 27 Other likely explanations include the short rest period between tests with partial metabolic recovery or perhaps a low motivation to repeat the test.11 Interestingly, the use of the 6MWD from the ‘best effort’ test was recently criticized and the 6MWD obtained as the average of trials has been considered as more representative of the true value.36 In this regard, the averaged 6MWD is not influenced by the order of the greater-distance test. Further studies are required to confirm if the decreasing trend in repetitive 6MWD is specific to patients with hypertension. Moreover, whether a single 6MWD38 or multiple 6MWD are necessary for this population and, in the latter case, whether the proper outcome for the evaluation of cardiac rehabilitation programs is the ‘best effort’ or the averaged 6MWD still requires clarification.
Patients with hypertension presented lower 6MWD compared with sex-matched healthy controls, highlighting that the 6MWT captures the hemodynamic-related functional capacity of patients with hypertension. Personal variables (age, body height and weight) that are considered as risk factors for CVD also have an inverse effect on the 6MWD in patients with hypertension. It appears surprising that the same factors also affect the 6MWD in healthy controls. However, this is not contradictory because cardiovascular risk increases linearly with blood pressure values.3, 4 In addition, the large SD of the 6MWD observed in patients compared with healthy controls reflects the heterogeneity of phenotypes in hypertension itself. Accordingly, the systematic overestimation of the 6MWD by the Brazilian equations based on healthy controls can be explained by the low 6MWD values observed because of the adopted methods. However, the absence of a significant difference between groups in two out of three reference equations26, 27—along with their low R2—strongly suggests that equations derived from control groups are not capturing the statistical relationships between the 6MWD and clinical, and hemodynamic variables, which are population-specific.
Both groups presented values of the 6MWD that were somewhat lower than those of other studies.18, 19, 20, 21, 23 The systematically low values are because of methodological factors known to affect negatively both groups simultaneously, including the smaller corridor and the lack of incentive phrases used during the test. The sex-match design of this study was selected because sex is a variable that is consistently correlated with the 6MWD,11, 15 with male subjects exhibiting higher values than female subjects in both studied groups. Body height, although not controlled, was not significantly different between groups and therefore exerted no directional influence on the 6MWD. Other uncontrolled variables in this study are known to negatively (higher age and body weight in the patient group)11 and positively (higher physical activity level in the control group)40 affect the 6MWD. Those differences in personal variables may contribute to a larger difference between groups but are unlikely to change the outcome of the study—the association between hemodynamic variables and functional capacity—although a reduction in statistical power may be expected because of the small sample size.41 Most importantly, those differences comprise actual risk factors for CVD that are indeed more prevalent in patients with hypertension than in healthy controls.5 Consequently, the hemodynamic-related functional capacity presented by patients and controls was indeed captured by the 6MWT and is reflected as the 6MWD.
The observed significant association values between the 6MWD and personal variables suggest that these variables influence the test outcome. The strengthening of the bivariate correlation between the 6MWD and hemodynamic variables in both groups after controlling for confounders further suggests their potential as predictors while reinforcing the internal validity of this study. Other studies also found a significant and inverse association between PP and 400-m gait speed in elderly subjects at risk for mobility disability, suggesting that hemodynamic parameters are associated with functional capacity tests, notwithstanding a self-paced gait.42 On the basis of this interpretation, the inclusion of hemodynamic variables in equations for the prediction of the 6MWD appears justified. Most importantly, the significant association between hemodynamics and functional capacity in healthy subjects justifies the use of the 6MWT as a diagnostic routine test in the population at risk of developing CVD for the early recognition of impaired functional capacity. This clinical implication of this statement in primary preventive medicine is in agreement with the current trend in hypertension management of treating patients who have not yet manifested symptoms.43
A new trend is emerging in the development of the 6MWD prediction equations. Given the apparent limitation of the reference equations in adjusting between the real and predicted 6MWD, a new approach replaces the comparison ‘patient–control’ with ‘patient–patient’. This new approach has already been applied for the derivation of a more specific equation for use in patients with Parkinson’s disease. The outcomes from other tests specifically related to the pathophysiology of the disease—the Berg Balance Scale and TUG—were also identified as independent predictors along with weight, height, age and sex.44, 45 The 6MWD was also a marker of disability in patients with systemic sclerosis with disease-specific determinants of the 6MWD, such as disease activity and the Scleroderma Health Assessment Questionnaire score.46 Similarly, the results of this study call for the further investigation of new prediction equations based on the hemodynamic variables associated with the 6MWD, mainly MP because of its higher significant correlation and adjusted R2 in the models evaluated. To this end, a large sample of adults with hypertension presenting different phenotypes and other risk factors for CVD should be studied to determine a specific prediction equation for this population to be used as an outcome of cardiac rehabilitation programs.
Some study limitations deserve consideration regarding the interpretation of the results. All patients were under antihypertensive treatment with different combinations of medication classes and dosages, and thus drug effects on blood pressure levels and performance could not be investigated. Although blood pressure levels could be corrected to account for this, this was not performed because a constant correction factor would not change the observed associations. Nevertheless, the studied sample included patients with grade I–II hypertension despite drug therapy, which is likely to result from resistant hypertension or suboptimal medication regimens that were still under adjustment.47 Therefore, the observed results are considered representative for medicated patients and should not be extrapolated to untreated patients without proper evidence. In addition, the finding of the highest observed R2 value in model no. 3 suggests that other variables such as physical activity level and HR could be used to improve the prediction of the 6WMD. However, because of the sample size that would be required, this evaluation was not performed in our study and is recommended for future studies. Notably, we did not assess indices of left ventricular function (for example, stroke volume) that are correlated to the 6MWD in patients with heart failure,48 and as such, this might represent a confounder of our results. Finally, the cause–effect relationship between hemodynamic variables and the 6MWD cannot be assessed in this study. Case–control designs do not allow causal inference (that is, the increase in hemodynamic variables decreases the 6MWD and a decrease in hemodynamic variables increases the 6MWD per se) owing to a possible cause-and-effect reversal, and thus the results must be interpreted accordingly.
In summary, our study demonstrated that the 6MWD is inversely associated with hemodynamic variables in both groups and is lower in patients with hypertension compared with healthy controls. Hemodynamic variables, particularly the MP, should be included in prediction equations for 6MWD under the concept of ‘patient–patient’ comparison.
References
Kearney PM, Whelton M, Reynolds K, Whelton PK, He J . Worldwide prevalence of hypertension. A systematic review. J Hypertens 2004; 22: 11–19.
Picon RV, Fuchs FD, Moreira LB, Riegel G, Fuchs SC . Trends in prevalence of hypertension in Brazil: a systematic review with meta-analysis. PLoS One 2012; 7: e48255.
MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, Abbott R, Godwin J, Dyer A, Stamler J . Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990; 335: 765–774.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R . Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Hernández N, Torres SH, Finol HJ, Vera O . Capillary changes in skeletal muscle of patients with essential hypertension. Anat Record 1999; 256: 425–432.
Hajjar I, Lackland DT, Cupples LA, Lipsitz LA . Association between concurrent and remote blood pressure and disability in older adults. Hypertension 2007; 50: 1026–1032.
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB . The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985; 132: 919–923.
Solway S, Brooks D, Lacasse Y, Thoimas S . A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001; 119: 256–270.
Hamm LF, Wenger NK, Arena R, Forman DE, Lavie CJ, Miller TD, Thomas RJ . Cardiac rehabilitation and cardiovascular disability: role in assessment and improving functional capacity. J Cardiopulm Rehabil Prev 2013; 33: 1–11.
Papathanasiou JV, Ilieva E, Marinov B . Six-minute waling test: An effective and necessary tool in modern cardiac rehabilitation. Hellenic J Cardiol 2013; 54: 126–130.
Balke B . A simple field test for the assessment of physical fitness. Rep Civ Aeromed Res Inst US 1963, 1–8.
McGavin CR, Gupta SP, McHardy GJ . Twelve-minute walking test for assessing disability in chronic bronchitis. BMJ 1976; 1: 822–823.
Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM . Two-, six-, and twelve-minute walking distance tests in respiratory disease. BMJ 1982; 284: 1607–1608.
Dourado VZ . Reference equations for the 6-minute walk test in healthy individuals. Arq Bras Cardiol 2011; 96: e128–e138.
Casanova C, Celli BR, Barria P, Casas A, Cote C, de Torres JP, Jardim J, Lopez MV, Marin JM, Montes de Oca M, Pinto-Plata V, Aguirre-Jaime A, Six Minute Walk Distance Project (ALAT). The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J 2010; 37: 150–156.
Accyoli MF, Piotto RF . Effect of a cardiac rehabilitation program–phase III carried out on hypertensive women in a therapeutic pool and on the ground. Rev Inst Ciênc Saúde 2007; 25: 141–146.
Lima MMO, Britto RR, Baião EA, Alves GS, Abreu CDG, Parreira VF . Aerobic exercises on the control of post menopause hypertension. Fisioter Mov 2011; 24: 23–31.
Souza JF, Nogueira IDB, Lira MJL, Silva EC, Ferreira GMH, Nogueira PAMS . Correlation between functional fitness and quality of life in elderly hypertensive women undergoing resistance training. ConScientiae Saúde 2011; 10: 312–318.
Ribeiro A, Younes C, Mayer D, Fréz AR, Riedi C . Six minute walk test on cardiovascular risk factors women evaluation. Fisioter Mov 2011; 24: 713–719.
Costa HS, Martins AMB, Quirino FC, Severino G, Novais LD, Lima MMO . Functional capacity in hypertensive men by walked distance and correlations with the reference equations. Fisioter Mov 2009; 22: 557–564.
Enright PL, McBurnie MA, Bittner V, Tracy RP, McNamara R, Arnold A, Newman AB . Cardiovascular Health Study. The 6-minute walk test—a quick measure of functional status in elderly adults. Chest 2003; 123: 387–398.
Pedrosa R, Holanda G . Correlation between the walk, 2-minute step and TUG tests among hypertensive older women. Rev Bras Fisioter 2009; 13: 252–256.
Willis BH . Spectrum bias—why clinicians need to be cautions when applying diagnostic test studies. Fam Pract 2008; 25: 390–396.
Iwama AM, Andrade GN, Shima P, Tanni SE, Godoy I, Dourado VZ . The six-minute walk test and body weight-walk distance product in healthy Brazilian subjects. Braz J Med Biol Res 2009; 42: 1080–1085.
Dourado VZ, Vidotto MC, Guerra RLF . Reference equations for the performance of healthy adults on field walking tests. J Bras Pneumol 2011; 37: 607–614.
Soares MR, Pereira CAC . Six-minute walk test: reference values for healthy subjects in Brazil. J Bras Pneumol 2011; 37: 576–583.
Pickering G . Hyperpiesis: high blood pressure without evident cause: essential hypertension. BMJ 1965; 2: 1021–1026 concl.
Parker DR, Lapane KL, Lasater TM, Carleton RA . Short stature and cardiovascular disease among men and women from two southeastern New England communities. Int Epidemiol Ass 1998; 27: 970–975.
Hamilton DM, Haennel RG . Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. J Cadiopulm Rehabil 2000; 20: 156–164.
Pires SR, Oliveira AC, Parreira VF, Britto RR . Six-minute walk test at different ages and body mass indexes. Rev Bras Fisioter 2007; 11: 131–134.
Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira E, Oliveira LC, Braggion G . Questionário internacional de atividade física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Ativ Física Saúde 2001; 6: 5–18.
Pardini R, Matsudo SM, Araújo T, Matsudo V, Andrade E, Braggion G, Andrade D, Oliveira L, Figueira JRA, Raso V . Validação do questionário internacional de nível de atividade física (IPAQ—versão 6): estudo piloto em adultos jovens brasileiros. Rev Bras Ciênc Mov 2001; 9: 45–51.
World Health Organization. Western Pacific Region, International Association for the Study of Obesity, International Obesity Task Force. Redefining obesity and its treatment. World Health Organization: Geneva, Switzerland. 2000.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117.
Dolmage TE, Hill K, Evans RA, Goldstein RS . Has my patient responded? Interpreting clinical measurements such as the 6-minute walk test. Am J Respir Crit Care Med 2011; 184: 642–646.
Tanaka H, Monahan KD, Seals DR . Age-predicted maximal heart rate revisited. J Am Coll Cardiol 2001; 37: 153–156.
Bellet RN, Francis RL, Jacob JS, Healy KM, Bartlett HJ, Adams L, Morris NR . Repeated six-minute walk tests for outcome measurement and exercise prescription in outpatient cardiac rehabilitation: a longitudinal study. Arch Phys Med Rehabil 2011; 92: 1388–1394.
Camarri B, Eastwood PR, Cecins NM, Thompson PJ, Jenkins S . Six minute walk distance in healthy subjects aged 55-75 years. Respir Med 2006; 100: 658–665.
Steffens D, Beckenkamp PR, Hancock M, Paiva DN, Alison JA, Menna-Barreto SS . Activity level predicts 6-minute walk distance in healthy older females: an observational study. Physiotherapy 2013; 99: 21–26.
Farejö T, Farejö A . To match or not to match in epidemiological studies—same outcome but less power. Int J Environ Res Public Health 2010; 7: 325–332.
Heffernan KS, Manini TM, Hsu F-C, Blair SN, Nicklas BJ, Kritchevsky SB, Newman AB, Sutton-Tyrrell K, Church TS, Haskell WL, Fielding RA . Relation of pulse pressure to long-distance gait speed in community-dwelling older adults: findings from the LIFE-P study. PLoS One 2012; 7: e49544.
Ferreira AS . Integrative medicine for hypertension: the earlier the better for treating who and what are not yet ill. Hyperten Res 2013; 36: 1–7.
Falvo MJ, Earhart GM . Six-minute walk distance in persons with Parkinson disease: a hierarchical regression model. Arch Phys Med Rehabil 2009; 90: 1004–1008.
Falvo MJ, Earhart GM . Reference equation for the six-minute walk in individuals with Parkinson disease. J Rehabil Res Dev 2009; 46: 1121–1126.
Deuschle K, Weinert K, Becker MO, Backhaus M, Huscher D, Riemekasten G . Six-minute walk distance as a marker of disability and complaints in patients with systemic sclerosis. Clin Exp Rheumatol 2011; 29: S52–S59.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM, American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, Kronenberg MW, Kostis JB, Kohn RM, Guillotte M, Greenberg B, Woods PA, Bourassa MG . Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. JAMA 1993; 270: 1702–1707.
Acknowledgements
This study was supported by a grant (APQ1 E-26/110.450/2012) from the Fundação Carlos Chagas Filho de Amparo à Pesquisa no Estado do Rio de Janeiro (FAPERJ). We also thank the anonymous reviewers for their helpful suggestions and comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramos, R., Guimarães, F., Cordovil, I. et al. The six-minute walk distance is a marker of hemodynamic-related functional capacity in hypertension: a case–control study. Hypertens Res 37, 746–752 (2014). https://doi.org/10.1038/hr.2014.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.59
Keywords
This article is cited by
-
Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit
Hypertension Research (2016)