Abstract
Microalbuminuria is an indicator of renal disease and is known to be related to obesity. The aim of this study is to investigate the association between the cross-sectional area of visceral adipose tissue (VAT) and the prevalence of microalbuminuria. We conducted a cross-sectional study of 1154 subjects who underwent routine checkups, including computed tomography (CT) scans of abdominal adipose tissue. We used the lowest tertile as a reference of abdominal fat. The highest tertile of VAT was related to the highest prevalence of microalbuminuria (odds ratio (OR): 1.96; 95% CI: 1.12–3.43). Subcutaneous adipose tissue (SAT) was not associated with microalbuminuria. In men, the highest tertile for VAT was associated with the highest prevalence of microalbuminuria (OR: 2.74; 95% CI: 1.44–5.22). In women, VAT or SAT was not associated with microalbuminuria. In nondiabetic subjects, the highest tertile for VAT was associated with the highest prevalence of microalbuminuria (OR: 2.23; 95% CI: 1.15–4.32). Among subjects without metabolic syndrome or with body mass index <25 kg m−2, the highest tertile for VAT was associated with microalbuminuria in age- and sex-adjusted model, respectively (OR: 1.62; 95% CI: 1.01–2.31; OR: 2.21; 95% CI: 1.05–4.65). The analysis of the association of VAT and insulin resistance (IR) indicated that a higher VAT was associated with a higher IR (highest tertile for VAT—OR: 2.91; 95% CI: 1.70–4.96). In conclusion, the highest VAT of the current study was significantly correlated with the highest prevalence of microalbuminuria, even in traditionally low-risk subjects without diabetes, and this association is potentially related with a higher IR.
Similar content being viewed by others
Introduction
Microalbuminuria is known as an early clinical manifestation of diabetic nephropathy. Recent studies showed that microalbuminuria is a predictor of cardiovascular disease and renal disease in subjects without diabetes.1, 2 Central obesity is associated with the metabolic syndrome and insulin resistance (IR).3 Several anthropometric studies have reported that microalbuminuria is related to central obesity.4, 5, 6, 7 These studies, however, could not differentiate between visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) accumulation, because waist circumference or waist-to-hip ratio was used as a measure to evaluate central obesity.4, 5, 6, 7
Visceral fat is known to be metabolically active and contributes to cardiovascular outcomes. Therefore, the effect of visceral obesity should be evaluated separately from that of the subcutaneous obesity.8 To date, there are no clear standard for the evaluation of visceral fat obesity. However, Horie et al.,9 in a study on male Japanese individuals, defined the visceral fat obesity as VAT >100 cm2.9 He et al.10 reported that the metabolic risk increased significantly in both men and women at VAT >100 cm2.10 However, additional review of the clinical usefulness of these criteria and the re-establishment of standards that takes into account variability-introducing factors such as gender is required. There are a few studies that have evaluated the association of VAT with albuminuria.11, 12, 13, 14 The studies, however, were conducted among diabetic patients,11, 12, 13, 14 or included morbidly obese populations.8, 11 To date, very few studies have investigated the association of VAT and microalbuminuria in generally healthy Asian populations. As obese Asians usually have higher VAT with a lower body mass index (BMI) than Westerners, the evaluation of VAT could be more important in the Asian population. The purpose of this study is to investigate the association between visceral obesity and the prevalence of microalbuminuria in the general population, especially in subjects without diabetes or the metabolic syndrome in Korea.
Methods
Study sample
We conducted a cross-sectional study of 1165 subjects who underwent routine comprehensive health check-ups at the Healthcare System of Gangnam Center of Seoul National University Hospital from September 2006 through December 2010. The patients age ranged from 30 to 82 years. In addition, all candidates were required to undergo computed tomography (CT) scan analysis of abdominal adipose tissue and measurement of the albumin-to-creatinine ratio. Those with macroalbuminuria (urinary albumin-to-creatinine ratio, UACR >300 mg g−1) or hematuria by dipstick urinalysis, cancer or active infection were excluded from the study. A total of 1154 subjects were found to be eligible for this study. The study protocol conformed to the ethical guidelines of the updated Declaration of Helsinki Principle (2008) and was approved by the Institutional Board of Seoul National University Hospital.
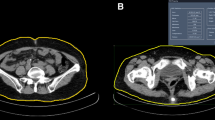
Measuresment of VAT and SAT cross-sectional area
The adipose tissue was measured at the level of the umbilicus using a 16-detector row CT scanner. The cross-sectional area (cm2) of the abdominal fat was calculated using the Rapidia 2.8 CT software (INFINITT, Seoul, Korea). The VAT cross-sectional area was defined as the intraperitoneal section of fat bound by parietal peritoneum and transversalis fascia. The SAT cross-sectional area was defined as the fat that is external to the abdomen and back muscles. As a clear standard for normal abdominal fat has not been established to date, we used the lower tertile as a reference group after dividing the abdominal fat data into three parts.
Assessment of UACR
UACR levels were determined by collecting first morning spot urine samples during the clinical examination using the clean-catch technique. The urine samples were obtained after at least 12 h of fasting. Urinary albumin was measured with an immunoturbidimetric assay and urinary creatinine was measured using the Jaffe rate reaction. In this study, microalbuminuria is defined as an albumin-to-creatinine ratio (range, 30–300 mg g−1) in a first morning spot urine sample.
Other measurements and definitions
Assessments of medical history, smoking status, the alcohol consumption status and the current use of medications, including aspirin and hormone replacement therapy, were based on the replies to a standardized questionnaire. Subjects with a fasting glucose level ⩾126 mg dl−1 or hemoglobin A1C ⩾6.5% or the current use of diabetes medication were considered as diabetic, whereas those with a systolic blood pressure (BP) >140 mm Hg or diastolic BP >90 mm Hg or taking antihypertensive medication were considered as hypertensive. Those smoking at least one cigarette a day in the past year were considered as current smokers, whereas those who stopped smoking for at least 1 year were considered as past smokers. Women were considered to have attained the menopausal stage if the menstrual cycle had ceased for at least 1 year. BP was measured using a standardized sphygmomanometer with patients in a sitting position, after a 5-min rest, and an average of three measurements was recorded. The height and weight of the subjects were measured with the individuals dressed only in an examination gown and without shoes. BMI is expressed as the weight in kilograms divided by the square of the height expressed in meters (kg m−2). The waist circumference was measured in the standing position at the level of the umbilicus by an examiner. Blood samples were collected after at least 12 h of fasting and were used to determine triglyceride, high-density lipoprotein-cholesterol, glucose and fasting insulin. To estimate IR, homeostasis model assessment (HOMA) was used, according to the following equation: HOMA-IR=fasting insulin (μU ml−1) × fasting glucose (mg dl−1)/405.15 Our definition of metabolic syndrome followed the National Cholesterol Education Program Adult Treatment Panel III (NCEP/ATP III) guidelines. The presence of any three of the following five traits allowed a diagnosis of the metabolic syndrome: central obesity was defined as a waist circumference ⩾90 cm in male subjects and ⩾80 cm in female subjects.16 Hypertriglyceridemia was defined as triglyceride ⩾150 mg dl−1, low high-density lipoprotein level was defined as high-density lipoprotein-cholesterol <40 mg dl−1 in male subjects and <50 mg dl−1 in female subjects. High BP was defined as a BP ⩾130 85 mm Hg or hypertension subjects, and high fasting plasma glucose was defined as fasting plasma glucose ⩾100 mg dl−1 or diabetic subjects. IR was defined as the highest quartile of HOMA-IR.17
Statistical methods
The participants were divided into three groups according to their abdominal fat content. Age-adjusted, sex-specific Pearson’s correlation coefficients were used to assess the correlation of UACR with the measures of cross-sectional area of abdominal fat (VAT or SAT). Analysis of variance and χ2 test were used to determine whether there were differences in the prevalence of microalbuminuria among the VAT and SAT cross-sectional area groups. After univariate analysis, a multivariate logistic regression analysis was performed, which was adjusted for variables that showed significant association (P<0.05) in the univariate logistic regression analysis (P<0.05). All statistical analyses of the data were conducted with SPSS version 19.0 software (SPSS, Chicago, IL, USA). All reported P-values were two-tailed, and the threshold of statistical significance was set at P<0.05.
Results
Baseline characteristics
The baseline characteristics of the participants separated by the tertile for cross-sectional area of VAT and by sex are shown in Table 1. For each group, the overall means and means for each tertile for cross-sectional area of VAT are shown along with the incidence of comorbidity. The average age of the participants was 56 years for men and 58 years for women. Overall, the prevalence of microalbuminuria was 10.4% in the entire group, 11.0% among men and 6.8% among women. Among the studied population, 17% and 41% had diabetes or hypertension, respectively. In addition, 44% of men and 24% of women had metabolic syndrome. The mean BMI was 24.92±2.62 in men and 23.14±2.87 in women. There was a positive association between microalbuminuria and VAT cross-sectional area (P<0.001 for men and P<0.049 for women). Mean±s.d. of VAT cross-sectional area was 85±27 cm2 in T1, 144±14 cm2 in T2 and 211±33 cm2 in T3. There was a significantly higher prevalence of microalbuminuria in men with a greater VAT cross-sectional area (P<0.001), but not in women (P=0.106). In both sexes, higher VAT was associated with a higher prevalence of diabetes, hypertension and metabolic syndrome and a higher HOMA-IR mean (Table 1).
Association of VAT tertiles with microalbuminuria
Table 2 shows the OR for microalbuminuria that corresponds to the abdominal obesity. In both sex, the highest tertile for VAT cross-sectional area was associated with the highest prevalence of microalbuminuria in the multivariate model (OR: 1.96; 95% CI: 1.12–3.43). SAT cross-sectional area was not related to microalbuminuria. Among men, the highest tertile for VAT cross-sectional area was associated with the highest prevalence of microalbuminuria (OR: 2.74; 95% CI: 1.44–5.22). The SAT cross-sectional area was not related to microalbuminuria in the multivariate model. Among women, there was no association between VAT or SAT cross-sectional area and microalbuminuria.
Association of VAT tertiles and microalbuminuria in subjects without diabetes, metabolic syndrome or BMI <25 kg m−2
Because diabetes significantly affects the prevalence of microalbuminuria, we also analyzed the association between visceral obesity and microalbuminuria among subjects with diabetes (Table 3). In both sexes, the highest VAT cross-sectional area was shown to be related to the highest prevalence of microalbuminuria (OR: 2.23; 95% CI: 1.15–4.32). In the subgroup analysis among men, the highest VAT cross-sectional area was associated with the highest prevalence of microalbuminuria (OR: 2.72; 95% CI: 1.22–6.03). Among women, VAT-cross sectional area and microalbuminuria were not associated with each other.
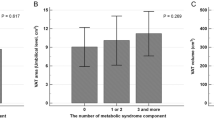
As the metabolic syndrome is known to be related to microalbuminuria, we conducted a subgroup analysis of subjects without this condition (Table 4). In both sexes, the highest VAT cross-sectional area was only associated with the highest prevalence of microalbuminuria in an age- and sex-adjusted model (OR: 1.62; 95% CI: 1.01–2.31), but not in the multivariate analysis.
In addition, we conducted analysis in subjects BMI <25 kg m−2. In both sexes, the highest VAT cross-sectional area was only associated with the highest prevalence of microalbuminuria in an age- and sex-adjusted model (OR: 2.21; 95% CI: 1.05–4.65), but not in the multivariate analysis.
The association of VAT tertiles with IR
As the most accepted hypothesis that is attributed to the pathophysiology of microalbuminuria is IR, we analyzed the association between visceral obesity and IR. We defined IR as the highest quartile of HOMA-IR. In this analysis, as VAT cross-sectional area went higher, the prevalence of IR became higher (T2—OR: 1.90; 95% CI: 1.14–3.19; T3—OR: 2.91; 95% CI: 1.70–4.96) in the multivariate model (Table 4). This indicated a significant increase in the prevalence of IR in the highest tertile of VAT cross-sectional area.
Discussion
The principal objective of this study was to investigate the relationship between abdominal obesity and microalbuminuria in the general population in Korea. The results of this study indicate that the highest tertile for VAT cross-sectional area was significantly associated with the highest prevalence of microalbuminuria, especially among men, although SAT cross-sectional area showed no significant association with microalbuminuria. In subjects without diabetes, the highest VAT cross-sectional area was significantly associated with the highest prevalence of microalbuminuria. Similarly, among subjects without the metabolic syndrome, the highest VAT cross-sectional area was associated with the highest prevalence of microalbuminuria in age- and sex-adjusted model. These findings suggest that VAT cross-sectional area is associated with microalbuminuria even in subjects with a low cardiovascular risk, such as nondiabetic subjects or subjects without the metabolic syndrome. Among women, however, VAT cross-sectional area was not significantly related to the prevalence of microalbuminuria. Therefore, we can summarize that the prevalence of microalbuminuria is related to VAT cross-sectional area rather than SAT cross-sectional area, especially in men.
In this study, VAT cross-sectional area shows a significant association with the prevalence of microalbuminuria in generally healthy Koreans. There are several studies on abdominal obesity and the prevalence of microalbuminuria in Asians. A correlation between abdominal fat and prevalence of microalbuminuria was demonstrated in Japanese diabetic patients.12, 14 An association between visceral fat using a bioelectrical impedance analysis method and prevalence of microalbuminuria was demonstrated in Japanese male subjects.18 In addition, a study examining a Chinese population found that the BMI, waist circumference and waist-to-hip ratio had a significant correlation with microalbuminuria.19 However, two of the studies included only diabetic patients, and another study had a small sample size, although it was conducted in a healthy population. As these studies did not measure abdominal fat with CT scanning, the effect of VAT or SAT could not be evaluated precisely. Therefore, the clinical significance of VAT and SAT in the nondiabetic healthy population has not been sufficiently explored, so far.
To the best of our knowledge, only a few studies have reported an association between the CT-based measurements of VAT with the development of albuminuria.13, 14 Recently, a large-population-based study was conducted to identify the correlation between the prevalence of microalbuminuria and VAT or SAT, based on the CT scan analysis in both men and women.8 It is a well-designed study and the results showed a significant correlation between VAT and the prevalence of microalbuminuria in men. In that study, however, the definition of microalbuminuria also included macroalbuminuria (i.e., UACR >25 mg g−1 in women or >17 mg g−1 in men). Because the clinical significance of microalbuminuria and macroalbuminuria varies, that of microalbuminuria needs to be evaluated separately.20 Furthermore, the study also included obese subjects as the mean BMI exceeded 27 kg m−2. Considering that the mean BMI of Asians is approximately 25 kg m−2, the population in our study (mean BMI: 24.92 kg m−2) could more appropriately represent Asian populations. Hence, our study is of value as it analyzes microalbuminuria and investigates healthy and less obese Asians.
The relationship between microalbuminuria and VAT has already been established in an obese population8, 11 or in a diabetic population.11, 12, 13, 14 However, the relationship between microalbuminuria and VAT was not clear for a population with a traditionally low cardiovascular risk, such as subjects without diabetes or the metabolic syndrome. In this study, even in nondiabetic individuals, a significant correlation between VAT cross-sectional area and the prevalence of microalbuminuria was observed. Similarly, an analysis of subjects without the metabolic syndrome or BMI <25 kg m−2 indicated that there was a significant correlation between the VAT cross-sectional area and prevalence of microalbuminuria in an age- and sex-adjusted model. These results suggest that even in a traditionally low-risk group, the VAT cross-sectional area was related to microalbuminuria.
Our results suggest that visceral obesity is independently associated with prevalence of microalbuminuria among men, but not among women. This result is consistent with a previous study.8 In that study, there was a significant relationship between visceral obesity and microalbuminuria in men, but not in women. This suggests that the clinical implication of obesity may differ between men and women. Although the precise mechanism underlying the gender difference in the relationship between visceral obesity and microalbuminuria has not been elucidated, the differences between men and women in fat metabolism, fat deposition patterns and the health consequences of obesity are widely accepted.21 He et al. attributed the lower incidence of visceral fat obesity in women than in men to a metabolic protective effect of adiponectin.10 However, women with visceral fat were found to have more increased metabolic risk compared with men, although the underlying pathophysiology was not clear. Men are more likely to deposit fat in the abdominal region. However, the fat distribution in women varies depending on age, as women tend to accumulate adipose tissue in the gynoid region (thigh and buttock), but after the age of 40 years or during the post-menopausal period, accumulate fat in the abdomen and the visceral area. Therefore, we analyzed the association between microalbuminuria and visceral fat in women according to their menopausal status, but the results were not significant. However, we cannot exclude the possibility that the sample size of postmenopausal women was inadequate. In the case of women, more studies using a larger population stratified by age and menopausal stage are needed.
In the analysis of the association between VAT cross-sectional area and IR, a higher VAT cross-sectional area was associated with a higher prevalence of IR. The mechanisms that underlie the observed link between VAT and microalbuminuria may involve IR, as suggested by our findings that a higher VAT cross-sectional area was associated with a greater IR. These results indicate a close relationship between VAT cross-sectional area and IR, as described previously.11, 22, 23
Whether VAT has a unique association with microalbuminuria or whether SAT shares this link has been the subject of controversy.24 Two studies have proposed that SAT had a protective effect on the development of microalbuminuria in women8 and had a negative correlation with the metabolic risk factors.25 However, in our study, the SAT cross-sectional area was not related to microalbuminuria. We also analyzed the association between the VAT-to-SAT ratio and microalbuminuria to identify the interaction of VAT and SAT, but we did not find any correlation. Therefore, further studies are needed to investigate the association between SAT and microalbuminuria.
This study had certain limitations. First, as our study was a cross-sectional study, we could not identify a causal link between visceral adiposity and microalbuminuria. Second, the study was performed in an individual center and the subjects were candidates who were recruited for a regular health check-up; therefore, a selection bias was unavoidable. Another limitation was that the microalbuminuria was measured only once from the spot urine sample collected in the morning. Although 24-h or overnight urine collections are originally used to measure albumin excretion, good correlations are already known between the UACR and albuminuria levels measured overnight or in 24-h urine collections.26
In conclusion, we found that VAT cross-sectional area is associated with the prevalence of microalbuminuria in Korean men. Furthermore, this phenomenon can be observed in subjects without diabetes and metabolic syndrome and even in BMI <25 kg m−2 subjects. In our study, higher VAT cross-sectional area is associated with IR. Asians are quite prone to visceral fat accumulation, which may explain their greater propensity to develop microalbuminuria at relatively low BMI levels.23 Asians with visceral obesity should make a concerted effort toward weight reduction to prevent renal dysfunction and the cardiovascular risk associated with microalbuminuria. Furthermore, clinicians should seriously consider decreasing the VAT of the traditionally low-risk population to prevent microalbuminuria. However, further studies using a larger sample size are required to validate these findings in women.
References
Romundstad S, Holmen J, Hallan H, Kvenild K, Kruger O, Midthjell K . Microalbuminuria, cardiovascular disease and risk factors in a nondiabetic/nonhypertensive population. The Nord-Trondelag Health Study (HUNT, 1995–97), Norway. J Intern Med 2002; 252: 164–172.
Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, Appleyard M, Jensen JS . Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 2004; 110: 32–35.
Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, Fujimoto WY . Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med 2004; 140: 992–1000.
de Boer IH, Sibley SD, Kestenbaum B, Sampson JN, Young B, Cleary PA, Steffes MW, Weiss NS, Brunzell JD . Central obesity, incident microalbuminuria, and change in creatinine clearance in the epidemiology of diabetes interventions and complications study. J Am Soc Nephrol 2007; 18: 235–243.
Kramer H, Reboussin D, Bertoni AG, Marcovina S, Lipkin E, Greenway FL 3rd, Brancati FL . Obesity and albuminuria among adults with type 2 diabetes: the Look AHEAD (Action for Health in Diabetes) Study. Diabetes Care 2009; 32: 851–853.
Liese AD, Hense HW, Doring A, Stieber J, Keil U . Microalbuminuria, central adiposity and hypertension in the non-diabetic urban population of the MONICA Augsburg survey 1994/95. J Hum Hypertens 2001; 15: 799–804.
Pinto-Sietsma SJ, Navis G, Janssen WM, de Zeeuw D, Gans RO, de Jong PE . A central body fat distribution is related to renal function impairment, even in lean subjects. Am J Kidney Dis 2003; 41: 733–741.
Foster MC, Hwang SJ, Massaro JM, Hoffmann U, DeBoer IH, Robins SJ, Vasan RS, Fox CS . Association of subcutaneous and visceral adiposity with albuminuria: the Framingham Heart Study. Obesity (Silver Spring, MD) 2011; 19: 1284–1289.
Horie N, Komiya H, Mori Y, Tajima N . New body mass index criteria of central obesity for male Japanese. Tohoku J Exp Med 2006; 208: 83–86.
He H, Ni Y, Chen J, Zhao Z, Zhong J, Liu D, Yan Z, Zhang W, Zhu Z . Sex difference in cardiometabolic risk profile and adiponectin expression in subjects with visceral fat obesity. Transl Res 2010; 155: 71–77.
Nielsen S, Jensen MD . Relationship between urinary albumin excretion, body composition, and hyperinsulinemia in normotensive glucose-tolerant adults. Diabetes Care 1999; 22: 1728–1733.
Asakawa H, Tokunaga K, Kawakami F . Relationship of abdominal fat with metabolic disorders in diabetes mellitus patients. Diabetes Res Clin Pract 2002; 55: 139–149.
Sibley SD, de Boer IH, Steffes MW, Brunzell JD . Intra-abdominal fat and elevated urine albumin excretion in men with type 1 diabetes. Diabetes Care 2007; 30: 1898–1900.
Hanai K, Babazono T, Nyumura I, Toya K, Ohta M, Bouchi R, Suzuki K, Inoue A, Iwamoto Y . Involvement of visceral fat in the pathogenesis of albuminuria in patients with type 2 diabetes with early stage of nephropathy. Clin Exp Nephrol 2010; 14: 132–136.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Zhao Z, Nie H, He H, Yan Z, Liu D, Luo Z, Ma L, Ni Y, Chen J, Jing J, Cao T, Yang H, Tepel M, Zhang W, Zhu Z . High sensitivity C-reactive protem predicts target organ damage in Chinese patients with metabolic syndrome. Metabolism 2007; 56: 1612–1619.
Kalish GM, Barrett-Connor E, Laughlin GA, Gulanski BI . Association of endogenous sex hormones and insulin resistance among postmenopausal women: results from the Postmenopausal Estrogen/Progestin Intervention Trial. J Clin Endocrinol Metab 2003; 88: 1646–1652.
Tamba S, Nakatsuji H, Kishida K, Noguchi M, Ogawa T, Okauchi Y, Nishizawa H, Imagawa A, Nakamura T, Matsuzawa Y, Funahashi T, Shimomura I . Relationship between visceral fat accumulation and urinary albumin–creatinine ratio in middle-aged Japanese men. Atherosclerosis 2010; 211: 601–605.
Zheng J, Ye P, Wang X, Xiao WK, Wu HM . The relationship between obesity and microalbuminuria among general population in Beijing area. Zhonghua Nei Ke Za Zhi 2011; 50: 388–392.
Mathiesen ER, Ronn B, Storm B, Foght H, Deckert T . The natural course of microalbuminuria in insulin-dependent diabetes: a 10-year prospective study. Diabetes Med 1995; 12: 482–487.
Power ML, Schulkin J . Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr 2008; 99: 931–940.
Hoehner CM, Greenlund KJ, Rith-Najarian S, Casper ML, McClellan WM . Association of the insulin resistance syndrome and microalbuminuria among nondiabetic native Americans. The Inter-Tribal Heart Project. J Am Soc Nephrol 2002; 13: 1626–1634.
Després JP, Lemieux I . Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881–887.
Goodpaster BH, Thaete FL, Simoneau J-A, Kelley DE . Subcutaneous abdominal fat and thigh muscle composition predict insulin sensitivity independently of visceral fat. Diabetes 1997; 46: 1579–1585.
Hamdy O, Porramatikul S, Al-Ozairi E . Metabolic obesity: the paradox between visceral and subcutaneous fat. Curr Diabetes Rev 2006; 2: 367.
Molitch ME, DeFronzo RA, Franz MJ, Keane WF, Mogensen CE, Parving HH . Diabetic nephropathy. Diabetes Care 2003; 26 (Suppl 1): S94–S98.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H., Kim, H., Shin, N. et al. Visceral obesity is associated with microalbuminuria in nondiabetic Asians. Hypertens Res 37, 679–684 (2014). https://doi.org/10.1038/hr.2014.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.47
Keywords
This article is cited by
-
Albuminuria and markers for cardiovascular risk in 12-year-olds from the general Dutch population: a cross-sectional study
European Journal of Pediatrics (2023)
-
The Short-Term Renal Effects of Bariatric Surgery: A Comparative Study Between Sleeve Gastrectomy and One Anastomosis Gastric Bypass Operations Among Egyptian Patients With Severe Obesity
Obesity Surgery (2020)
-
The need for noninvasive methods to monitor hemodynamics in hypertension therapy
Hypertension Research (2016)
-
Relations of body weight status in early adulthood and weight changes until middle age with hypertension in the Chinese population
Hypertension Research (2016)
-
Waist circumference compared with other obesity parameters as determinants of coronary artery disease in essential hypertension: a 6-year follow-up study
Hypertension Research (2016)