Abstract
Obesity, arterial stiffness and high aldosterone levels can interact to cause resistant hypertension (RHTN). Lower adiponectin (APN) levels may be significantly associated with hypertension. However, the importance of hypoadiponectinemia as a complicating factor in the lack of blood pressure (BP) control in individuals with RHTN has not been demonstrated. Ninety-six RHTN patients were classified into uncontrolled (UCRHTN, n=44) and controlled (CRHTN, n=52) subgroups. Their APN and aldosterone levels, office and ambulatory BP (ABPM) measurements, endothelium-dependent brachial artery responses (flow-mediated dilation (FMD)), left ventricular mass index (LVMI) and pulse wave velocity (PWV) were evaluated. The UCRHTN subgroup had increased aldosterone levels, as well as higher LVMI and PWV. In addition, lower APN levels and impaired FMD response were found in this subgroup. The brachial and ABPM pulse pressures were inversely associated with the APN levels (r=−0.45, P=0.002; r=−0.33, P=0.03, respectively), as were the aldosterone levels and the PWV (r=−0.38, P=0.01; r=−0.36, P=0.02, respectively) in UCRHTN patients. The PWV was only significantly influenced by the APN level in the UCRHTN subgroup in the multivariate regression analysis. None of the correlations mentioned above were observed in the CRHTN subgroup. Hypoadiponectinemia and high aldosterone levels may therefore be implicated in resistance to antihypertensive therapy related to arterial stiffness.
Similar content being viewed by others
Introduction
Resistant hypertension (RHTN) is a condition in which the blood pressure (BP) remains above the target level (140/90 mm Hg) despite the concurrent use of three or more antihypertensive drugs of different classes. Ideally, one of these agents should be a diuretic, and all agents should be prescribed at optimal doses.1 This revised definition includes a subgroup of resistant hypertensive patients whose BP is controlled using four or more antihypertensive medications; these patients are referred to as having controlled RHTN (CRHTN).1 This designation may be useful for better categorizing RHTN with regard to etiology and prognosis, but we recently demonstrated that some important clinical and mechanistic findings differ between CRHTN and uncontrolled RHTN (UCRHTN) subjects.2, 3 In addition, emerging data suggest that obesity, arterial stiffness, cardiac hypertrophy, high plasma aldosterone levels and endothelial dysfunction are not only associated with RHTN but may also interact to have an important role in causing RHTN.2, 4 Moreover, vascular stiffness, as assessed by the pulse wave velocity (PWV), has been shown to be correlated with RHTN.5
Putative mechanisms of obesity-related hypertension include increased sympathetic activity, hyperstimulation of the renin–angiotensin–aldosterone system, impaired endothelial function and reduced urinary sodium excretion.6 These mechanisms underlie the hypothesis that obesity and RHTN are linked to excess circulating aldosterone, which has a significant role in the pathogenesis of metabolic syndrome and RHTN.7 A growing body of evidence indicates that cardiovascular and renal abnormalities associated with insulin resistance are mediated in part by aldosterone, acting on the mineralocorticoid receptor. Furthermore, the detection of hyperaldosteronism is important not only to treat cardiometabolic disease but also to indicate the state of ‘aldosterone excess,’ which is an increased level of aldosterone without hyperaldosteronism. Aldosterone excess has detrimental metabolic effects that contribute to metabolic syndrome and endothelial dysfunction, as well as to the development of RHTN, cardiovascular disease and chronic kidney disease.7
Adipose tissue is currently considered to be a large endocrine gland that participates in the regulation of diverse biological functions.8 The communication between adipose tissue and other biological systems is accomplished by the expression of a large number of bioactive mediators that are collectively called adipokines.8 Adiponectin (APN) is one of the most important adipokines. Previous evidence suggests that lower plasma APN concentrations are significantly associated with hypertension;9, 10, 11 however, the importance of hypoadiponectinemia as a complicating factor for the lack of BP control has not been evaluated in individuals with RHTN.
This study sought to determine the plasma APN levels and its association with the lack of BP control in RHTN patients. The associations between the APN levels and other clinical features frequently associated with this condition were also evaluated.
Methods
This cross-sectional study was approved by the Research Ethics Committee of the Faculty of Medical Sciences, University of Campinas (Campinas, Brazil), and all participants gave written informed consent form before enrolling in the study (approval no. 222/2011).
Patient population
Ninety-six RHTN subjects regularly evaluated at the Outpatient Resistant Hypertension Clinic of the University of Campinas (Campinas, Brazil) who complied with the pharmacological treatment regimen for RHTN were recruited to participate in this observational study. Patients were classified in two groups—the UCRHTN (n=44) and CRHTN (n=52) groups—and were matched for age, sex and body mass index (BMI). The diagnosis of RHTN requires a good office BP measurement technique and ambulatory BP monitoring (ABPM) to confirm persistently elevated BP levels.1 White coat hypertension was excluded by ABPM.1 Patients with pseudoresistance, including a lack of BP control secondary to poor medication adherence, as well as patients with secondary forms of hypertension, were properly identified and excluded.12 All individuals were regularly assessed during the first 6 months for drug therapy optimization. ABPM was used not only to exclude pseudoresistance to antihypertensive treatment but also as an auxiliary method to characterize UCRHTN and CRHTN patients.
The exclusion criteria were the presence of type 1 and type 2 diabetes, acute or moderate-severe renal or liver dysfunction, noncompliance with the pharmacological treatment regimen, obesity (BMI ⩾30 kg m−2), heart failure (ejection fraction <50%), valvular heart disease, cardiomyopathies, primary hyperaldosteronism (aldosterone–plasma renin activity ratio (ARR) >20 ng dl−1 per ng ml−1 h−1), sleep apnea (classified as ‘high risk’ by the Berlin sleep questionnaire), cardiac arrhythmias, aortic disease (Marfan’s syndrome, coarctation of the aorta, aneurysms or aortic surgery), a clinical history of coronary artery disease or proven coronary artery disease by coronary angiography or noninvasive tests, previous stroke, peripheral vascular disease, familial hyperlipidemia, pregnancy or oral contraceptive use, connective tissue disorders, neurological problems, malignancies, psychiatric diseases, smoking, alcohol use and drug abuse.
Nonpharmacological therapies were optimized, including a salt-restricted diet, which was monitored by measuring urinary sodium excretion (<100 mEq per 24 h).
Office BP measurements
BP was assessed at ∼0800 hours. Each subject’s BP (SBP—systolic BP; DBP- diastolic BP and PP—pulse pressure) was measured three times using a digital sphygmomanometer (Omron HEM-711DLX, OMRON Healthcare, Bannockburn, IL, USA) on the right upper arm in the sitting position after a 10-minute rest.
Ambulatory BP monitoring
The 24-hour ABPM was taken using a Spacelabs 90217 ambulatory BP monitor (Spacelabs, Redmond, WA, USA).13 Patients were instructed to perform normal daily activities and to note their sleep period in a personal diary.
Echocardiography
Measurements of the left ventricular (LV) dimensions were performed according to the American Society of Echocardiography recommendations14 using two-dimensional targeted M-mode echocardiography. The diastolic LV and systolic LV diameters, as well as the interventricular septal (IVS) and LV posterior wall thicknesses at the end of diastole, were measured using the features of the QRS wave assessed by electrocardiography. The LV mass index (LVMI) was calculated by dividing the LV mass by the body surface area. The echocardiographic measurements were evaluated by two-blinded independent investigators using a cardiovascular ultrasound machine (Siemens Acuson CV70, Munich, Bavaria, Germany) with a multifrequency sector transducer (2–4 MHz). The intraobserver and interobserver coefficients of variation were <5.5% for the diastolic LV diameter, systolic LV diameter, interventricular septal and LV posterior wall thicknesses, and <9.5% for the LVMI.
Endothelial function
Brachial artery dilation was measured using a linear vascular transducer (7–12 MHz, Toshiba Powervision 6000, Tokyo, Japan) coupled with computer-assisted analysis software and automated brachial analyzer software (Brachial Analyzer, Medical Imaging Applications, Coralville, IA, USA). The endothelium-dependent brachial artery responses (flow-mediated dilation, FMD) and endothelium-independent brachial artery responses (glyceryl-trinitrate mediated) were determined in accordance with current guidelines.15 All studies were initiated at 0800 hours after overnight fasting, and the subjects were placed in a supine position in a quiet, air-conditioned room (22–24 °C). Changes in the brachial artery diameter in both the endothelium-dependent and endothelium-independent analyses were expressed as a percentage change relative to the vessel diameter immediately before cuff inflation and drug administration, respectively. The vascular function was assessed by only one experienced blinded examiner, and there was no significant intraobserver measurement variability.
Aortic PWV measurement
The aortic PWV was measured using the velocity method with the patients in a supine position using a previously validated Complior SP system and software (Artech-Medical, Paris, France).16 Waveforms were obtained transcutaneously using the right common carotid and femoral arteries simultaneously during a minimum period of 10–15 s. The time delay (t) between the two waveforms was measured, and the distance (D) covered by the waves was measured directly between the femoral recording site and the suprasternal notch minus the distance to the carotid recording site. The PWV was calculated as D (m)/t (sec). Three consecutive readings were obtained, and the PWV is reported as the mean. The values were corrected to account for the mean arterial pressure.
Laboratory assessment
Baseline blood samples for the measurement of the plasma aldosterone concentration (PAC), plasma renin activity and plasma APN level were collected at 0800 hours after overnight fasting. During this time, the volunteers rested in a supine position for 8 h, followed by 1 h in an upright position in an air-conditioned room (22–24 °C). The PAC and total plasma APN levels were measured using enzyme-linked immunosorbent assays (ELISA; DRG International, Springfield, NJ, USA; and Quantikine Human total adiponectin/Acrp30 Immunoassay DRP 300, R&D Systems, Minneapolis, MN, USA, respectively) according to the manufacturer’s instructions. Plasma renin activity radioimmunoassay was performed using standard technique (Mayo Clinic Laboratories, Rochester, MN, USA). The inter-assay and intra-assay coefficients of variance were <8.5% for the PAC ELISA kit and <5.5% for the APN ELISA kit.
Statistical analysis
The data are expressed as the mean and and standard erron of the mean (s.e.m) or median (1st and 3rd quartiles). The normality of the distributions was assessed using the Kolmogorov–Smirnov test. Significant differences between the study groups were identified using Student’s t-test or the Mann–Whitney test for independent samples and Fisher’s test for categorical variables. Pearson’s or Spearman’s correlation test was used for the correlation analyses. Multiple regression analysis was used to predict the PWV from the age, aldosterone concentration and APN level, and to predict the FMD from the aldosterone and APN plasma level, with the aim of identifying the relative effects of these variables on the PWV and FMD. The level of significance accepted was 0.05.
Results
Table 1 lists the general characteristics of the study groups. No significant differences were observed between the UCRHTN and CRHTN subgroups with respect to age, sex and BMI. The mean ages of patients were 57±1.6 and 59±1.5 years in the UCRHTN (26 female/18 male) and CRHTN (35 female/17 male) groups, respectively, and all patients were overweight (25.0⩽BMI⩽29.9). As expected, higher office and ABPM SBPs and DBPs, as well as PPs, were found in UCRHTN individuals. Although both subgroups had LV hypertrophy, the LVMI was higher in the UCRHTN patients than the CRHTN patients. In addition, the UCRHTN subgroup had higher aortic PWV and more severe impairment in the FMD test than the CRHTN subgroup. The NTG responses in the UCRHTN and CRHTN subgroups were similar.
The biochemical test results did not show differences between the UCRHTN and CRHTN subgroups except with respect to the PAC, ARR and APN levels (Table 2). The PAC and ARR levels were higher and the APN levels were lower in UCRHTN than in CRHTN patients.
UCRHTN subjects were taking a mean of 4.9 classes of antihypertensive drugs daily, and their drug distribution was diuretics (100%), spironolactone (31.8%), β-blockers (52.3%), angiotensin-converting enzyme inhibitors (27.3%), angiotensin receptor blockers (77.3%), calcium channel blockers (65.9%) and centrally acting antihypertensive drugs (11.4%). The CRHTN subgroup was taking a mean of 4.5 drugs daily, with the prescribed medications being diuretics (100%), spironolactone (23.1%), β-blockers (46.2%), angiotensin-converting enzyme inhibitors (32.7%), angiotensin receptor blockers (34.6%), calcium channel blockers (28.8%) and centrally acting antihypertensive drugs (3.8%).
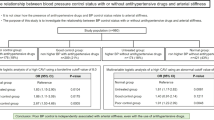
Correlation analysis for the UCRHTN subjects indicated that the plasma APN levels were inversely associated with the aldosterone concentration and the PWV (r=−0.38, P=0.01; and r=−0.36, P=0.02, respectively) (Figure 1). Furthermore, the plasma APN levels were inversely correlated with the office (Figure 2a) and ABPM SBPs (r=−0.33, P=0.03; and r=−0.42, P=0.01, respectively), as well as the brachial (Figure 2b) and ABPM PPs (r=−0.45, P=0.002; and r=−0.33, P=0.03, respectively) in UCRHTN patients. However, the plasma APN levels were not associated with the office (Figure 2c) and ABPM DBPs, the LVMI, the FMD or the ARR in the same group. The aldosterone concentrations were correlated with the PWV (r=0.43; P=0.003) in uncontrolled patients but not in the controlled patients. Multivariate linear regression analysis showed that the PWV was only significantly influenced by the APN level in UCRHTN patients (Table 3). The APN and aldosterone levels did not influence the FMD test results in the same subgroup (data not shown). Finally, the plasma APN levels were not correlated with any parameter in CRHTN subjects, in contrast to the findings for the UCRHTN subgroup.
Discussion
To the best of our knowledge, this is the first study to analyze the plasma APN levels in RHTN patients. We found that a lower plasma APN level, a higher PAC, increased vascular stiffness and LV hypertrophy, and greater impairment of endothelial function are characteristics that distinguish patients with UCRHTN from those with CRHTN. Taken together, these results, except the APN levels, support the results of previous studies using RHTN subgroups.2, 3 Poorly controlled hypertension undoubtedly leads to progressive vascular and heart damage.3 In addition, the APN levels were inversely associated with the PWV, PAC and office and ABPM pulse, and SBPs in the UCRHTN subgroup but not in the CRHTN subgroup. Finally, the APN level was predictor of the PWV in patients with UCRHTN. These findings suggest that there are several important differences in pathophysiology that may underlie the development of RHTN with respect to subgroups.
Hypoadiponectinemia can be related to hypertension via multiple mechanisms, such as insulin resistance, sympathetic activation, increased circulating fatty acid levels, impaired endothelium-dependent vasodilation and vascular inflammation.10 In turn, we showed that the APN level was inversely correlated with the office SBP and PPs in UCRHTN patients but not with the office diastolic pressure. In addition, the APN level was inversely associated with the systolic and pulse ABPM pressures. The observed correlations between the APN level and the SBP and PP can be explained by the fact that both BP components increase in response to increases in vascular resistance and large-artery stiffness. Therefore, cardiovascular risk may be more closely related to the pulsatile stress caused by large-artery stiffness during systole than to the steady-state stress due to small-vessel resistance during diastole.17, 18
Our results revealed a significant inverse relationship between the APN levels and the PWV in UCRHTN subjects. Recent studies confirm that the APN level is inversely associated with arterial stiffness in hypertensive patients.19, 20 Different mechanisms have been suggested to explain this association. APN may stimulate the activity of endothelial nitric oxide synthase,21 and also it is associated with reduced vascular smooth muscle cell proliferation.22 APN inhibits almost all pathological conditions involved in vascular disease and exerts its multiple pleiotropic effects by its direct actions on several vascular cell types.23
We found that the APN level was not associated with vascular function or the LVMI. Previous studies have found that hypoadiponectinemia was associated with impaired endothelium-dependent vasorelaxation.24 In addition, the APN level was found to be inversely correlated with the LVMI in a cross-sectional study.25 We hypothesized that the plasma APN level may be associated with endothelial dysfunction and LV hypertrophy in the early stages of hypertension. Endothelial dysfunction should be considered to be restricted to the early phase in the pathogenesis of cardiovascular disease. Moreover, several studies have established an effect of endothelial dysfunction on arterial stiffening, and the reduced bioavailability of nitric oxide impairs vascular smooth muscle relaxation, causing progressive arterial stiffening.26 The APN level might be helpful as a marker of endothelial dysfunction and might be useful in assessing the early stages of atherosclerosis.24 Conversely, the correlation between endothelial function and arterial stiffness might be reduced in advanced stages of hypertension, as observed in the RHTN group.27 This pattern may explain the poor correlation between the APN level and the brachial FMD in both the UCRHTN and CRHTN subgroups (Figure 3).
Progression from the early to severe stages of hypertension and difficult-to-control high BP levels are characterized by increased arterial rigidity and impaired endothelial function. Therefore, the correlation between endothelial dysfunction and arterial rigidity might be reduced or even absent in the advanced stages of hypertension (NT, normotensive patients; HTN, hypertensive patients; RHTN, resistant hypertensive patients).
Accumulating evidence indicates that increased levels of aldosterone are related to the pathogenesis of RHTN in obese individuals and mediate several maladaptive changes.7 The PAC and BP both fall when patients successfully lose weight.28 The APN level was inversely associated with the aldosterone concentration, which in turn was positively associated with arterial stiffness. Similarly, higher leptin levels have been shown to be associated with increased aldosterone and BP levels in UCRHTN patients when compared with CRHTN and well-controlled hypertensive patients.29 Li et al.30 demonstrated that aldosterone decreases APN expression in adipocytes, and this effect may be one of the primary mechanisms by which aldosterone is related to metabolic and cardiovascular disorders. High aldosterone concentration results in the dysregulation of proinflammatory cytokines and the APN mRNA levels in adipocytes through the activation of mineralocorticoid receptors.31 With respect to arterial stiffness, aldosterone promotes collagen deposition, enhancing vascular remodeling and impairing arterial elasticity.32
Weight loss is one possible way to increase the plasma APN level, and significant reductions in the body weight due to important lifestyle changes (almost 14% reduction in the BMI)33 modify circulating the APN level.
The management of RHTN should include nonpharmacological approaches aimed to reduce the amount of adipose tissue by rigorous lifestyle changes; the early administration of intensive pharmacological therapies, primarily those targeting the renin–angiotensin–aldosterone system and mineralocorticoid receptors; and the optimization of the treatments of RHTN-related disorders, such as diabetes and dyslipidemia.
The main limitation of this study was the small number of UCRHTN and CRHTN patients enrolled. This study did not evaluate the identity of the multimeric APN species present in the circulation,34 and further research is needed to determine whether any specific multimeric species is more closely associated with the variables assessed in this study. The 24-hour urinary aldosterone excretion rate test was not performed, although this assay could help to assess patients with changes in aldosterone physiology. As previously reported in Fasshauer et al,35 the APN levels were higher in women than in men (data not shown). For this reason, the UCRHTN and CRHTN groups were carefully sex-matched in this study to eliminate the effects of this bias. Some pharmacological aspects of our results should be taken into account. Although antihypertensive drugs can influence the APN level,31, 36, 37 these possible sources of interferences did not affect our findings. The UCRHTN subjects had reduced APN levels even though they used a greater number of antihypertensive agents. Furthermore, the lack of standard antihypertensive therapy was because of the use of individualized care. Resistant hypertensive subjects could not be assessed withdrawing the antihypertensive drugs—and trying to exclude the influence of these medications on the adiponectin levels—due to ethical concerns.
Because this study was cross-sectional, causal inferences cannot be made. However, our findings support a possible link between hypoadiponectinemia and vascular disease in RHTN condition.
In summary, we demonstrated that the PP, PAC and PWV were inversely associated with the plasma APN level only in UCRHTN patients. In addition to the involvement of a higher BP and PAC, lower APN levels and increased arterial stiffness can contribute to the greater resistance to antihypertensive treatment in the uncontrolled group and expose this group to increased cardiovascular risk. These outcomes have important implications for preventing and treating RHTN, with an intensive approach to lifestyle changes being important. The findings of the current study need to be confirmed in prospective clinical assessments using a larger RHTN population.
References
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM . Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Quinaglia T, Martins LC, Figueiredo VN, Santos RC, Yugar-Toledo JC, Martin JF, Demacq C, Pimenta E, Calhoun DA, Moreno H Jr . Non-dipping pattern relates to endothelial dysfunction in patients with uncontrolled resistant hypertension. J Hum Hypertens 2011; 25: 656–664.
Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, Demacq C, Pimenta E, Calhoun DA, Moreno H Jr . Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens 2011; 25: 532–538.
Yugar-Toledo JC, Tanus-Santos JE, Sabha M, Sousa MG, Cittadino M, Tacito LH, Moreno H Jr . Uncontrolled hypertension, uncompensated type II diabetes, and smoking have different patterns of vascular dysfunction. Chest 2004; 125: 823–830.
Pabuccu T, Baris N, Ozpelit E, Akdeniz B, Guneri S . The relationship between resistant hypertension and arterial stiffness. Clin Exp Hypertens 2011; 34: 57–62.
Kotchen TA, Grim CE, Kotchen JM, Krishnaswami S, Yang H, Hoffmann RG, McGinley EL . Altered relationship of blood pressure to adiposity in hypertension. Am J Hypertens 2008; 21: 284–289.
Sowers JR, Whaley-Connell A, Epstein M . Narrative review: the emerging clinical implications of the role of aldosterone in the metabolic syndrome and resistant hypertension. Ann Intern Med 2009; 150: 776–783.
Frayn KN, Karpe F, Fielding BA, Macdonald IA, Coppack SW . Integrative physiology of human adipose tissue. Int J Obes Relat Metab Disord 2003; 27: 875–888.
Iwashima Y, Katsuya T, Ishikawa K, Ouchi N, Ohishi M, Sugimoto K, Fu Y, Motone M, Yamamoto K, Matsuo A, Ohashi K, Kihara S, Funahashi T, Rakugi H, Matsuzawa Y, Ogihara T . Hypoadiponectinemia is an independent risk factor for hypertension. Hypertension 2004; 43: 1318–1323.
Chow WS, Cheung BM, Tso AW, Xu A, Wat NM, Fong CH, Ong LH, Tam S, Tan KC, Janus ED, Lam TH, Lam KS . Hypoadiponectinemia as a predictor for the development of hypertension: a 5-year prospective study. Hypertension 2007; 49: 1455–1461.
Adamczak M, Wiecek A, Funahashi T, Chudek J, Kokot F, Matsuzawa Y . Decreased plasma adiponectin concentration in patients with essential hypertension. Am J Hypertens 2003; 16: 72–75.
de Souza WA, Sabha M, de Faveri Favero F, Bergsten-Mendes G, Yugar-Toledo JC, Moreno H . Intensive monitoring of adherence to treatment helps to identify ‘true’ resistant hypertension. J Clin Hypertens 2009; 11: 183–191.
Groppelli A, Omboni S, Parati G, Mancia G . Evaluation of noninvasive blood pressure monitoring devices Spacelabs 90202 and 90207 versus resting and ambulatory 24-hour intra-arterial blood pressure. Hypertension 1992; 20: 227–232.
Sahn DJ, DeMaria A, Kisslo J, Weyman A . Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978; 58: 1072–1083.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R . Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 2002; 39: 257–265.
Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI . Assessment of arterial distensibility by automatic pulse wave velocity measurement. Validation and clinical application studies. Hypertension 1995; 26: 485–490.
Christensen KL . Reducing pulse pressure in hypertension may normalize small artery structure. Hypertension 1991; 18: 722–727.
Elzinga G, Westerhof N . Pressure and flow generated by the left ventricle against different impedances. Circ Res 1973; 32: 178–186.
Youn JC, Kim C, Park S, Lee SH, Kang SM, Choi D, Son NH, Shin DJ, Jang Y . Adiponectin and progression of arterial stiffness in hypertensive patients. Int J Cardiol 2011; 163: 316–319.
Mahmud A, Feely J . Adiponectin and arterial stiffness. Am J Hypertens 2005; 18: 1543–1548.
Chen H, Montagnani M, Funahashi T, Shimomura I, Quon MJ . Adiponectin stimulates production of nitric oxide in vascular endothelial cells. J Biol Chem 2003; 278: 45021–45026.
Matsuda M, Shimomura I, Sata M, Arita Y, Nishida M, Maeda N, Kumada M, Okamoto Y, Nagaretani H, Nishizawa H, Kishida K, Komuro R, Ouchi N, Kihara S, Nagai R, Funahashi T, Matsuzawa Y . Role of adiponectin in preventing vascular stenosis. The missing link of adipo-vascular axis. J Biol Chem 2002; 277: 37487–37491.
Zhu W, Cheng KK, Vanhoutte PM, Lam KS, Xu A . Vascular effects of adiponectin: molecular mechanisms and potential therapeutic intervention. Clin Sci (Lond) 2008; 114: 361–374.
Ouchi N, Ohishi M, Kihara S, Funahashi T, Nakamura T, Nagaretani H, Kumada M, Ohashi K, Okamoto Y, Nishizawa H, Kishida K, Maeda N, Nagasawa A, Kobayashi H, Hiraoka H, Komai N, Kaibe M, Rakugi H, Ogihara T, Matsuzawa Y . Association of hypoadiponectinemia with impaired vasoreactivity. Hypertension 2003; 42: 231–234.
Hong SJ, Park CG, Seo HS, Oh DJ, Ro YM . Associations among plasma adiponectin, hypertension, left ventricular diastolic function and left ventricular mass index. Blood Press 2004; 13: 236–242.
Wilkinson IB, MacCallum H, Cockcroft JR, Webb DJ . Inhibition of basal nitric oxide synthesis increases aortic augmentation index and pulse wave velocity in vivo. Br J Clin Pharmacol 2002; 53: 189–192.
Figueiredo VN, Yugar-Toledo JC, Martins LC, Martins LB, de Faria AP, de Haro Moraes C, Sierra C, Coca A, Moreno H . Vascular stiffness and endothelial dysfunction: correlations at different levels of blood pressure. Blood Press 2012; 21: 31–38.
Tuck ML, Sowers J, Dornfeld L, Kledzik G, Maxwell M . The effect of weight reduction on blood pressure, plasma renin activity, and plasma aldosterone levels in obese patients. N Engl J Med 1981; 304: 930–933.
de Haro Moraes C, Figueiredo VN, de Faria AP, Barbaro NR, Sabbatini AR, Quinaglia T, Ferreira-Melo SE, Martins LC, Demacq C, Junior HM . High-circulating leptin levels are associated with increased blood pressure in uncontrolled resistant hypertension. J Hum Hypertens 2012; 27: 225–230.
Li P, Zhang XN, Pan CM, Sun F, Zhu DL, Song HD, Chen MD . Aldosterone perturbs adiponectin and PAI-1 expression and secretion in 3T3-L1 adipocytes. Horm Metab Res 2011; 43: 464–469.
Guo C, Ricchiuti V, Lian BQ, Yao TM, Coutinho P, Romero JR, Li J, Williams GH, Adler GK . Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation 2008; 117: 2253–2261.
Brilla CG, Matsubara LS, Weber KT . Antifibrotic effects of spironolactone in preventing myocardial fibrosis in systemic arterial hypertension. Am J Cardiol 1993; 71: 12A–16A.
Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D . Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA 2003; 289: 1799–1804.
Pajvani UB, Du X, Combs TP, Berg AH, Rajala MW, Schulthess T, Engel J, Brownlee M, Scherer PE . Structure-function studies of the adipocyte-secreted hormone Acrp30/adiponectin. Implications fpr metabolic regulation and bioactivity. J Biol Chem 2003; 278: 9073–9085.
Fasshauer M, Klein J, Neumann S, Eszlinger M, Paschke R . Hormonal regulation of adiponectin gene expression in 3T3-L1 adipocytes. Biochem Biophys Res Commun 2002; 290: 1084–1089.
Yamada S, Ano N, Toda K, Kitaoka A, Shiono K, Inoue G, Atsuda K, Irie J . Telmisartan but not candesartan affects adiponectin expression in vivo and in vitro. Hypertens Res 2008; 31: 601–606.
Yilmaz MI, Sonmez A, Caglar K, Celik T, Yenicesu M, Eyileten T, Acikel C, Oguz Y, Yavuz I, Vural A . Effect of antihypertensive agents on plasma adiponectin levels in hypertensive patients with metabolic syndrome. Nephrology 2007; 12: 147–153.
Acknowledgements
This study was supported by the State of São Paulo Research Foundation (Fapesp), SP, Brazil; the National Council for Scientific and Technological Development (CNPq); and Coordination for the Improvement of Higher Education Personnel (Capes), Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Leandro Boer-Martins and Caroline Demacq are employees of Novartis Biociências S.A. (Brazil). All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Faria, A., Demacq, C., Figueiredo, V. et al. Hypoadiponectinemia and aldosterone excess are associated with lack of blood pressure control in subjects with resistant hypertension. Hypertens Res 36, 1067–1072 (2013). https://doi.org/10.1038/hr.2013.92
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.92
Keywords
This article is cited by
-
Eplerenone Versus Spironolactone in Resistant Hypertension: an Efficacy and/or Cost or Just a Men’s Issue?
Current Hypertension Reports (2019)
-
Pro-inflammatory Cytokines and Resistant Hypertension: Potential for Novel Treatments?
Current Hypertension Reports (2019)
-
Association of serum leptin levels with central arterial stiffness in coronary artery disease patients
BMC Cardiovascular Disorders (2016)
-
Positive correlation of serum adipocyte fatty acid binding protein levels with carotid–femoral pulse wave velocity in geriatric population
BMC Geriatrics (2015)
-
Adipokines: another link between obesity and hypertension
Journal of Human Hypertension (2015)