Abstract
Cardiovascular (CV) complications such as myocardial infarction, heart failure, stroke and renal failure are related to both the degree and the duration of blood pressure (BP) increase. Resistant hypertension (RH) is associated with a higher risk of CV complications and a higher prevalence of target organ damage (TOD). The relationship between CV disease and TOD can be bidirectional. Elevated BP in RH may cause CV structural and functional alterations, and the development or persistence of left ventricular hypertrophy, aortic stiffness, atherosclerotic plaques, microvascular disease and renal dysfunction, may render hypertension more difficult to control. Specifically, RH is related to several conditions, including obesity, sleep apnea, diabetes, metabolic syndrome and hyperaldosteronism, characterized by an overexpression of humoral and hormonal factors that are involved in the development and maintenance of TOD. Optimal therapeutic strategies, including pharmacological treatment and innovative invasive methodologies, have been shown to achieve adequate BP control and induce the regression of TOD, thereby potentially improving patient prognosis.
Similar content being viewed by others
Introduction
Resistant hypertension (RH) is defined as a systolic blood pressure (SBP) or a diastolic blood pressure (DBP) that remains elevated (that is, ⩾140/90 mm Hg in the general population) despite adherence to lifestyle measures and to pharmacological treatment with full doses of at least three antihypertensive medications, including one diuretic.1 RH is recognized as a clinical phenotype associated with a high CV risk.1
The risk of clinical complications, including stroke, acute aortic dissection, myocardial infarction, congestive heart failure and renal failure, is higher in patients with RH compared with other types of hypertensive patients, including not only well-controlled subjects, but also those with false resistant and masked hypertension.2, 3, 4
Redon et al.5 followed 86 patients with RH for an average period of 49 months and reported a 24.6% overall incidence of CV events. The incidence of CV events was associated with BP control (assessed by 24-h BP monitoring); the incidence increased progressively from 2.2 per 100 patient-years in the lowest tertile of DBP, to 9.5 in the intermediate tertile and to 13.6 in the highest tertile.
More recently, Daugherty et al.6 confirmed the high rate of CV events (death or myocardial infarction, heart failure, stroke or chronic kidney disease) in patients with RH. Among 205 750 patients with incident hypertension, 1.9% developed RH within a median of 1.5 years from the initial treatment. These resistant hypertensive patients were older, more often men and more frequently diabetics than were the nonresistant patients. CV events rates were significantly higher in those with RH as compared with those without (18.0% vs. 13.5%, P<0.001), and the hazard ratio was 1.47 (confidence interval (CI), 1.33–1.62) after adjusting for patient and clinical characteristics.
Resistant or refractory hypertension (RH) represents a subset of uncontrolled BP strongly associated with organ involvement, particularly at the cardiac, renal and vascular levels.7 The relationship between RH and CV disease/target organ damage (TOD) may be bidirectional. RH may directly cause the development and worsening of TOD through the persistent elevation of BP. Similarly, the presence of CV TOD may worsen the resistance to treatment, rendering hypertension more difficult to control.8, 9
In patients with renal disease, microvascular disease, left ventricular hypertrophy (LVH), aortic stiffness, cerebrovascular disease or those with secondary hypertension, the prevalence and incidence of RH is commonplace.
A number of studies have analyzed the association between RH and some aspects of TOD, but only few studies have evaluated the presence of damage to multiple organs. Other markers of CV risk, such as serum biomarkers, remain unexplored in these very high-risk patients.
The present review aims to update the currently available data on the relationship between RH and subclinical TOD at different levels (heart, kidney and micro- and macrocirculation) and to present select original data.
RH and cardiac organ damage
Among the different features of hypertensive heart disease, LVH, left ventricular dysfunction, left atrial enlargement and aortic root dilatation have been reported in RH patients.
The most frequent abnormality described in RH is LVH, assessed by both electrocardiography and echocardiography (Figure 1).
Cuspidi et al.10 identified 11 cross-sectional and longitudinal studies with 3325 patients at outpatient hypertension clinics, and observed that prevalence rates of echocardiographic LVH, as assessed by updated criteria, ranged from 55 to 75% of patients with RH, peaking at 91% in the patient subgroup with concomitant ECG LV strain. This analysis confirmed the author’s previous results.11 Treatment-induced reductions in ECG–LVH improved CV prognosis.
Significant data on ECG and echocardiographic findings in RH have been reported by a number of studies conducted in Brazil by Salles et al.12, 13, 14, 15, 16, 17
In these studies, true RH patients were identified by ambulatory BP monitoring, ruling out the presence of white-coat RH. In 471 RH patients, the prevalence rates of ECG (Cornell product >240 mV ms−1) and echocardiographic LVH (LV mass index (LVMI) >116 g m−2 in men and >104 g m−2 in women) were 29% and 81%, respectively. The authors assessed the relationship between QT interval-derived parameters and echocardiographic LVH, and observed that a QTc interval >440 ms and a Cornell product >240 mV ms−1 were associated with a 2.0- and 2.6-fold increased risk, respectively, of increased left ventricular mass as measured by echocardiogram.12 When the presence of a prolonged QT interval and an increased Cornell product were combined, the relative risk of echocardiographic LVH increased by 5.3- to 9.3-fold.
Salles et al.13 thereafter investigated the clinical significance of ECG strain pattern, identified in 101 RH patients (23%). In these patients, the prevalence of echocardiographic LVH was 91%. Patients with strain were more frequently men and exhibited lower body mass indices, more target organ damage, higher 24-h BP, higher serum creatinine and 24-h microalbuminuria and prolonged QT intervals than did patients without strain. In a multivariate analysis, the presence of ECG strain was associated with increased LV mass (P<0.001), higher 24-h-SBP (P<0.001), prolonged maximum QTc interval duration (P<0.001), lower waist circumference (P=0.009), male gender (P=0.011), physical inactivity (P=0.020), higher serum creatinine (P=0.031) and fasting glycemia (P=0.027), and the presence of coronary heart disease (P=0.001) and peripheral arterial disease (P=0.045).
With respect to echocardiographic LVH, in a smaller group of 60 RH patients (mean age 59±8 years, 63% women, mean body mass index 30±5 kg m−2, type 2 diabetes prevalence 28%), Hernandez-del Rey et al.18 observed 36 participants with good quality echocardiograms, 18 (50%) of whom exhibited LVH (LVMI >125 g m−2). The LVH prevalence rose to 67% when gender-specific criteria for LVH were used (that is, LV mass >134 g m−2 in men and >110 g m−2 in women). When patients with true RH and white-coat RH were compared, no differences in the prevalence of LVH were noted. The same prevalence was confirmed in a larger group (n=103) of true resistant hypertensive patients.19
Cuspidi et al.11 investigated the prevalence of TOD in the heart, carotid arteries and kidney in 54 true RH patients (mean age 57±10 years) and compared the prevalence to that in age and sex-matched hypertensive patients with well-controlled BP on a combination of two or three drugs. The prevalence of LVH was higher in the RH patients, ranging from 40 to 55% depending on the criteria for LVH used, and was highest with the gender-specific partition value of 51/47 g per m2.7. Concentric LVH was the most common geometric pattern of LVH in RH patients.
Castelpoggi et al.14 have collected the largest number of RH patients with echocardiographic examinations at the Rio de Janiero University. They studied 600 patients at high or very high CV risk (23% coronary heart disease and 15% previous cerebrovascular events) and observed LVH (LVMI >125 g m−2 in men and 110 g m−2 in women) in 75% of the patients.
The same group of authors was able to assess the prognostic value of alterations in ECG repolarization and voltage parameters in a large group of 538 RH patients (75% with echo LVH, according to the gender-specific LVMI >125/110 g m−2) prospectively followed for an average of 4.8 years.15 The authors demonstrated that among all repolarization parameters, only the QTc interval duration was an independent predictor of CV mortality and overall mortality.
In a subsequent analysis of the same database,16 the prognostic significance of serial changes in LV strain pattern (present at baseline in 21% of RH patients) was evaluated. The persistence or development of strain during the follow-up was associated with an increased risk of stroke (hazard ratio 3.09, 95% CI 1.40–6.81) and death from all causes (hazard ratio 1.99, 95% CI 1.10–3.61).
Finally, the prognostic significance of serial changes in LVH voltage criteria was analyzed in a slightly larger group of 552 patients.17 The presence of Cornell voltage and product criteria at baseline, but not the presence of Sokolow-Lyon voltage, was independently associated with an increased incidence of CV morbidity and mortality and with all-cause mortality during the follow-up. In addition, the regression or the absence of ECG–LVH from baseline to follow-up was associated with a lower incidence of major CV events.17
In the largest database of patients with RH, confirmed by 24-h ambulatory monitoring, ∼20% of patients satisfied the criteria for LVH by electrocardiogram.20
These data strongly suggest the importance of evaluating cardiac TOD in patients with RH, both at the initial evaluation as well as during treatment. Despite the evidence for the prognostic significance of LVH regression in several studies,21, 22 few studies have addressed the effect of antihypertensive treatment on LVH and LV mass changes in RH patients.23, 24
More recently, Gaddam et al.25 assessed in 34 RH patients the effects of spironolactone (25–50 mg per day) on LV mass, right ventricular mass and LV volumes as measured by magnetic resonance imaging. After 3 months of treatment with an aldosterone antagonist, a significant decrease was observed in LV mass, LV wall thickness and volumes, and left atrial size; the effect was greater in the group of 19 patients with RH due to primary aldosteronism.
The effect of renal denervation on echocardiographic LV mass was demonstrated by Brandt et al.26 in 46 RH patients compared with 18 controls who were receiving only medical treatment (mean number of drugs 4.7). The echocardiographic examinations performed 1 and 6 months after baseline revealed a significant reduction in LVM index and the E/E′ ratio (index of increased LV filling pressure) after the renal denervation procedure, whereas these parameters did not change during medical treatment. In the entire group of patients, the improvement in LVMI and the E/E′ ratio was related to the decrease in BP induced by treatment, although improvement was also observed in those patients who were defined as ‘nonresponders’ based on clinic BP values, thus suggesting some additional effect of sympathetic renal denervation of cardiac organ damage, possibly due to the more pronounced reduction of aortic stiffness, central BP and augmentation index27 (Figure 1).
RH and macrovascular damage
According to Towsend,28 a relationship exists between vascular calcification, arterial stiffness and RH. In patients with RH, the presence of TOD in large caliber vessels, such as the carotid arteries and aorta, may have a significant impact on BP control.29
In some studies, the increased prevalence of carotid walls thickness, atherosclerotic plaques and aortic stiffness has been demonstrated in RH patients.
Cuspidi et al.11 were the first authors to document the increased prevalence of intima-media thickening (⩾0.9 mm) or plaques (58% and 65%, respectively) in the carotid arteries of RH patients compared with a group of patients treated with a combination of antihypertensive drugs despite controlled BP values in the clinic and during 24 h BP monitoring (29% and 32%, respectively).
It has also been noted that among patients with carotid arteries stenosis, the prevalence of patients with RH, possibly secondary to renovascular hypertension, is elevated. Spence et al.30 analyzed 170 patients with carotid stenosis who participated in the North American Symptomatic Carotid Endarterectomy Trial or the Asymptomatic Carotid Artery Study, and these authors observed that among 79 patients with RH (mean arterial pressure >130 mm Hg despite treatment), 20 patients exhibited renovascular hypertension and 7 patients exhibited adrenocortical hyperplasia.
More recently, Schmieder et al.31 analyzed the presence of vascular TOD in 42 RH patients in terms of cerebral microangiopathy, as investigated by cerebral magnetic resonance imaging. Twenty-three patients exhibited cerebral microangiopathy that was associated with a lower heart rate and higher SBP during the nighttime. In addition, RH patients with cerebral microangiopathy exhibited similar carotid intima-media thickness, but higher pulse wave velocity (PWV), central pulse pressure and aortic augmentation pressure.
Other studies have evaluated the increase in aortic stiffness in patients with RH. Figueiredo et al.32 measured carotid-femoral PWV in 44 patients with RH, 35 patients with controlled BP values and 25 normotensive subjects, demonstrating a significant increase in PWV in patients with RH compared with the other two groups. Because endothelial function may contribute to the regulation of large artery elasticity, the authors evaluated flow-mediated changes in vessel diameter as an indicator of endothelial function by ultrasound examination of the brachial artery. The authors observed that a greater decrease in brachial artery flow-mediated vasodilation was more evident in RH patients compared with well-controlled hypertensive patients.
In the largest cross-sectional study of 600 resistant hypertensive patients without peripheral arterial disease, Castelpoggi et al.14 assessed arterial stiffness by aortic PWV measurements. The authors reported that 168 patients (28%) exhibited aortic PWV >12 m s−1. Patients with increased PWV were older and exhibited a higher prevalence of CV risk factors than those patients with normal PWV. A blunted nocturnal decrease in BP was independently associated with increased aortic stiffness in RH patients, as were older age, diabetes, microalbuminuria, low level of high-density lipoprotein-cholesterol and a widened 24-h pulse pressure.
In another study, 43 patients with controlled BP treated with four or more antihypertensive medications (‘controlled RH’) were compared with 47 uncontrolled RH patients. The two groups differed only in body mass index, the aldosterone-renin ratio, PWV and the degree of LVH, all of which were significantly higher in uncontrolled RH patients.33
Very recently, in a group of 120 patients with RH, the effect of renal denervation on aortic stiffness (and central BP) was assessed.27 The prevalence of an increased carotid-femoral PWV was 38% at baseline, and a significant reduction in PWV was observed after 6 months of treatment.
RH and microvascular damage
In hypertension, small artery remodeling is the most prevalent form and one of the first manifestations of TOD. The magnitude of remodeling of small resistance arteries in hypertension exhibits prognostic significance, with worse prognosis in patients with more significant remodeling.34
The presence of structural alterations in small arteries dissected from subcutaneous tissue biopsies has been observed in hypertensive patients using the micromyographic method, which directly investigates the abnormalities in small vessel wall and diameter.
The available evidence demonstrates that in patients with secondary hypertension (and a greater prevalence of RH), the increase in the media to lumen ratio (index of eutrophic remodeling) is particularly pronounced compared with that in both normotensive and essential hypertensive patients.35 Most interestingly, in patients with renovascular hypertension and to a lesser extent in those with primary aldosteronism, a more evident contribution of cell growth, leading to the development of hypertrophic remodeling, (indicating smooth muscle cell growth), has been observed. In addition, more pronounced tunica media fibrosis, with greater total collagen and an increase in collagen type III, has been demonstrated in patients with primary aldosteronism.36 Growth factors, especially endothelin-1 and angiotensin II, has a role in hypertrophic remodeling, although the mechanisms leading to eutrophic remodeling are less clear. Endothelin-1 is a powerful vasoconstrictor and mitogen, contributing to the elevation in BP and related vascular remodeling and TOD. The vascular effects of aldosterone may be mediated, as suggested by Schiffrin et al.,37 by the stimulation of endothelin production; in patients with RH, endothelin-1 levels are significantly higher than those in mild hypertensive patients or normotensive controls.
The evaluation of retinal vessels may represent a method for the evaluation of microcirculation TOD. Cuspidi et al.11 observed that RH patients undergoing traditional fundoscopic examination exhibited a very high rate of retinal vascular changes (narrowings and arteriovenous crossings) and a greater prevalence of grade 2 and 3 retinopathy (73 and 5%), according to the Keith-Wegener classification, as compared with a control group (38 and 0%).
Another study examining the oculi fundus was performed in 497 patients, of whom 63% exhibited true RH and 37% of whom exhibited white-coat RH; the results confirmed a higher prevalence of retinopathy in true resistant patients (55.2 vs. 40%, P=0.002).38
More recently, measurements of retinal arterioles have been performed in vivo using scanning laser Doppler flowmetry in 40 patients with treatment-RH. All of the parameters indicating the presence of microvascular abnormalities, that is, the wall-to-lumen ratio, the wall thickness and the wall cross section area, were not strongly associated with 24-h BP, but were associated with urinary sodium excretion. In this group of patients, urinary sodium excretion represented the only independent determinant of wall thickness and of wall cross-section area of retinal arterioles. Because retinal arteriolar alterations are related to cerebral vascular structure, these results could have important implications for risk stratification in patients with treatment-RH.39
RH and renal damage
Microalbuminuria is considered to be an early marker of intrarenal vascular dysfunction in arterial hypertension, and its prevalence has been investigated in RH patients.
Cuspidi et al.11 reported that microalbuminuria could be observed in 17% of RH patients (22±32 mg per 24 h; P<0,02) and in 12% of controls subjects (11±13 mg per 24 h; P<0,02). Even if mean urinary albumin excretion was significantly greater in the RH patients, a relatively low prevalence of microalbuminuria (measured with a 24 h urine collection), compared with other markers of TOD, was observed in the RH patients and the control groups, possibly because microalbuminuria may be a less sensitive approach for detecting TOD than echocardiography or vascular ultrasonography. In the present study, no significant differences in serum creatinine were observed between patients with and without refractory hypertension.
Nogueira et al.40 have investigated the association between albuminuria and clinical, laboratory and 24-h ambulatory blood pressure monitoring variables in 187 patients with RH, and have confirmed the high prevalence of microalbuminuria (29.4%). In logistic regression, 24-h, high-density lipoprotein-cholesterol, serum creatinine and diabetes mellitus were independently associated with albuminuria, suggesting that BP control appears to be fundamental for reducing microalbuminuria, and that two measures of kidney function, such as creatinine and albuminuria, should always be assessed in RH patients.
In a group of 84 patients with RH, the renal resistive index was measured in addition to albuminuria and CV abnormalities as a method to assess changes in intrarenal perfusion and as markers of systemic hemodynamic alterations and atherosclerosis. An increase in the renal resistive index (with a threshold of 0.7) indicated aortic and carotid vascular damage, and was associated with the presence of coronary arteries independent of albuminuria.41
In a cross-sectional analysis of 143 patients with the clinical diagnosis of RH, 103 true RH patients exhibited significantly higher LVMI and 24-h urinary albumin excretions than did patients with white-coat RH. In the two groups of RH patients, the prevalence of microalbuminuria was 50% and 18%, respectively.18
The same authors have also observed that in a cohort of 356 patients (mean age 64±11 years; 40.2% females) with RH selected from Spanish hypertension units, microalbuminuria (defined as urinary albumin/creatinine ratio ⩾2.5 mg mmol−1 in males or ⩾3.5 mg mmol−1 in females) was detected in 46.6% of patients. In a logistic regression analysis (adjusting for age and sex), elevated nighttime SBP (multivariate odds ratio, 1.014 (95% CI, 1.001–1.026); P=0.029) and reduced estimated glomerular filtration rate (GFR) (multivariate odds ratio, 2.79 (95% CI, 1.57–4.96); P=0.0005) were independently associated with the presence of microalbuminuria.42
As highlighted previously, the inadequate control of BP appears to be responsible for the high prevalence of subclinical alterations accompanying RH, but conversely, these alterations may contribute to resistance to treatment and to the persistence of a high-risk condition in these patients. In fact, in the Olivetti Heart Study, conducted in Southern Italy in the years 1994–1995, basal BP (systolic, diastolic or pulse pressure), cholesterol and the urinary albumin/creatinine ratio significantly predicted the risk of developing RH using a logistic regression model that also included age as a covariate.43
Significant evidence of the prognostic significance of renal abnormalities and organ damage related to RH has been provided by Salles et al.44, 45 at the University of Rio de Janeiro, Brazil, in a rather large cohort of patients with refractory hypertension. These authors measured the urinary albumin excretion rate at baseline and after 2 years of follow-up in 531 patients with RH, and observed a 33% prevalence of microalbuminuria at baseline. In addition, baseline microalbuminuria was a powerful risk predictor of CV morbidity and mortality and of all-cause mortality in patients with RH, independent of traditional CV risk factors, renal function and ambulatory BP levels. More interestingly, the adverse impact of microalbuminuria was associated with values lower than the traditional cutoff for microalbuminuria (12.5–18 mg/24 h). The finding that changes in microalbuminuria from baseline to follow-up were also associated with a parallel change in CV events44 is of fundamental importance, as it reinforces the need to be more aggressive to improve both BP control and TOD regression, particularly in patients with RH.
Authors have expanded these results by taking into account the prognostic importance of both a reduced GFR and the presence of microalbuminuria as prognostic predictors in the same group of RH patients. The presence of a reduced GFR (in 69% of patients) was one of the most important predictors of fatal and non-fatal CV events, and the presence or absence of microalbuminuria added further prognostic information. These data suggest that both kidney TOD measures should be used for CV risk assessment, not only in patients with essential hypertension but also in patients with RH.45
Because few studies have evaluated the presence of damage in more than one target organ,11, 31, 38 we considered it to be worthwhile to assess the prevalence of RH and of associated cardiac, vascular and renal TOD in 317 hypertensive individuals (173 treated) selected from a larger general population sample living in a small town in Northern Italy and who were participating in a prospective epidemiological study aimed at measuring the association between CV risk factors and TOD (Vobarno study).46, 47
All subjects underwent all laboratory investigations, including renal function evaluation (estimated GFR, calculated according to the Modification of Diet in Renal Disease, MDRD formula), M-mode, 2D Doppler echocardiographic examination, ultrasound examination of carotid arteries and measurement of carotid-femoral PWV (for details see study by Muiesan et al.48).
LVH was determined according to the European Society of Hypertension European Society of Cardiology (ESH-ESC) guidelines (LVMI >125 and 110 g m−2 body surface area in men and women, respectively). An additional criterion was also used (LVMI >47 g per m2.7 in women or 50 g per m2.7 in men).49
According to the criteria proposed by the guidelines,50 a normal wall was classified as having an intima-media thickness (IMT) <0.9 mm, wall thickening was defined as an IMT >0.9 mm and <1.3 mm, and a plaque was defined as the presence of a focal IMT > 1.3 mm. An increase in PWV exceeding 9.6 m s−1 was defined as vascular TOD.51
According to the definition proposed by Calhoun et al.,1 that is, the presence of BP values >140/90 mm Hg despite adherence to lifestyle measures and to pharmacological treatment with full doses of at least three antihypertensive medications, including one diuretic, the prevalence of RH was 9.5% among all hypertensive patients and increased to 17.3% when only treated hypertensive patients were analyzed.
In Table 1, the demographic and clinical characteristics of treated patients with (n=30) and without RH (n=143) are reported. RH patients were older, more often females and exhibited higher fasting glycemia.
Lower values of estimated GFR (72±17 vs. 80±16 ml min−1 per 173 m2; P=0.01) and a higher prevalence of CKD (estimated GFR <60 ml min−1 per 173 m2; 27% vs. 8.5%, P=0.01) were observed in patients with RH than in patients with controlled HT.
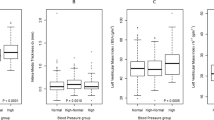
In RH, a significantly higher LVMI was observed, compared with that in controlled patients using two different indexations of LV mass (LVMI g per m2.7 48±11 vs. 41±10 g per m2.7; P=0.001 and LVMI g m−2 body surface area 101.6±23 vs. 89±21 g m−2, P=0.004). Accordingly, the prevalence of LVH was twofold higher in RH patients (40% vs. 21%; P=0.05).
The relative wall thickness was also greater in RH patients (0.420±0.08 vs. 0.38±0.06, P=0.001), suggesting a more concentric pattern of LVH (concentric geometry 40% vs. 22% in RH and controlled hypertensive patients, respectively, P=0.04). In RH patients, the mean common carotid and bifurcation maximal IMT (CBmax IMT, 1.48±0.42 mm vs. 1.25±0.31 mm; P<0.001) and the mean maximum IMT (Meanmax IMT, 1.47±0.42 vs. 1.21±0.32 mm; P=0.0001) were significantly higher in RH than in controlled treated hypertensive patients. The prevalence of carotid plaques was quite high in the entire population, but was greater in the group of RH patients (97% vs. 83%, P=0.04).
Finally, aortic stiffness (according to the measurement of carotid-femoral PWV) was increased in RH patients compared with subjects with satisfactory BP control (13.3±2.8 vs. 11.8±2.6 m s−1; P=0.03), and the prevalence of PWV >9.6 m s−1 was 71%, and 44%, P=0.04, respectively (Figure 2).
Our data confirm that RH is not a rare clinical condition, with a prevalence similar to that observed in previous studies in the United States.52 We were able to detect an increase in the prevalence and severity of TOD in the heart, kidney and macrovasculature, possibly reflecting the differences in age, glycemia and body mass index, but also reflecting the longer duration and severity of arterial hypertension. With respect to other studies, we assessed the simultaneous presence of subclinical alterations, including aortic stiffness, as few prior studies have accomplished.11, 31, 38 The presence of TOD in different vascular districts, including the heart and kidney, may explain the increased resistance to medical treatment. Furthermore, the presence of TOD is associated with a very high absolute CV risk, as recently underlined;6 thus, an urgent need exists to appropriately recognize and identify patients with RH and to achieve TOD regression to obtain adequate BP control.
References
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM . American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117: e510–e526.
Hall WD . Resistant hypertension, secondary hypertension, and hypertensive crises. Cardiol Clin. 2002; 20: 281–219.
Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, Caldarella MP, Neri M, Cuccurullo F, Mezzetti A . Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens 2005; 18: 1422–1428.
Papadopoulos DP, Papademetriou V . Resistant hypertension: diagnosis and management. J Cardiovasc Pharmacol Ther 2006; 11: 113–118.
Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM . Prognostic value of ambulatory blood pressure monitoring in refractory hypertension. A prospective study. Hypertension 1998; 31: 712–718.
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O'Connor PJ, Selby JV, Ho PM . Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012; 125: 1635–1642.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B . 2007 Guidelines for the management of arterial hypertension. The Task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
McAlister FA, Lewanczuk RZ, Teo KK . Resistant hypertension: an overview. Can J Cardiol 1996; 12: 822–828.
Ram CVS . Management of refractory hypertension. Am J Therapeut. 2003; 10: 122–126.
Cuspidi C, Vaccarella A, Negri F, Sala C . Resistant hypertension and left ventricular hypertrophy: an overview. J Am Soc Hypertens 2010; 4: 319–324.
Cuspidi C, Macca G, Sampieri L, Michev I, Salerno M, Fusi V, Severgnini B, Meani S, Magrini F, Zanchetti A . High prevalence of cardiac and extracardiac target organ damage in refractory hypertension. J Hypertens 2001; 19: 2063–2070.
Salles G, Leocadio S, Bloch K, Nogueira AR, Muxfeldt E . Combined QT interval and voltage criteria improve left ventricular hypertrophy detection in resistant hypertension. Hypertension 2005; 46: 1207–1212.
Salles G, Cardoso C, Nogueira AR, Bloch K, Muxfeldt E . Importance of the electrocardiographic strain pattern in patients with resistant hypertension. Hypertension 2006; 48: 437–442.
Castelpoggi CH, Pereira VS, Fiszman R, Cardoso CRL, Muxfeldt ES, Salles G . A blunted decrease in nocturnal blood pressure is independently associated with increased aortic stiffness in patients with resistant hypertension. Hypertens Res 2009; 32: 591–596.
Salles G, Cardoso CRL, Muxfeldt E . Prognostic value of ventricular repolarization prolongation in resistant hypertension: a prospective cohort study. J Hypertens 2009; 27: 1094–1101.
Salles G, Cardoso CRL, Fiszman R, Muxfeldt ES . Prognostic significance of baseline and serial changes in electrocardiographic strain pattern in resistant hypertension. J Hypertens 2010; 28: 1715–1733.
Salles G, Cardoso CRL, Fiszman R, Muxfeldt ES . Prognostic impact of baseline and serial changes in electrocardiographic left ventricular hypertrophy in resistant hypertension. Am Heart J 2010; 159: 833–840.
Hernandez-del Rey R, Armario P, Martin-Baranera M, Sanchez P, Cardenas G, Pardell H . Target-organ damage and cardiovascular risk profile in resistant hypertension. Influence of the white-coat effect. Blood Press Monit 1998; 3: 331–337.
Oliveras A, Armario P, Hernández-Del Rey R, Arroyo JA, Poch E, Larrousse M, Roca-Cusachs A, de la Sierra A . Urinary albumin excretion is associated with true resistant hypertension. J Hum Hypertens 2010; 24: 27–33.
de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, Oliveras A, Ruilope LM . Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 2011; 57: 898–902.
Armstrong AC, Gidding S, Gjesdal O, Wu C, Bluemke DA, Lima JA . LV mass assessed by echocardiography and CMR, cardiovascular outcomes, and medical practice. JACC Cardiovasc Imaging 2012; 5: 837–848.
Muiesan ML, Salvetti M, Rizzoni D, Castellano M, Donato F, Agabiti-Rosei E . Association of change in left ventricular mass with prognosis during long-term antihypertensive treatment. J Hypertens 1995; 13: 1091–1095.
de Faire U, Lindwall K, Andersson G, Eriksson S . Regression of left ventricular hypertrophy on long-term treatment with captopril of severe hypertensives refractory to standard triple treatment. Eur J Clin Pharmacol 1989; 37: 291–294.
Julien J, Dufloux MA, Prasquier R, Chatellier G, Menard D, Plouin PF, Menard J, Corvol P . Effects of captopril and minoxidil on left ventricular hypertrophy in resistant hypertensive patients: a 6 month double-blind comparison. J Am Coll Cardiol 1990; 16: 137–142.
Gaddam K, Corros C, Pimenta E, Ahmed M, Denney T, Aban I, Inusah S, Gupta H, Lloyd SG, Oparil S, Husain A, Dell'Italia LJ, Calhoun DA . Rapid reversal of left ventricular hypertrophy and intracardiac volume in patients with resistant hypertension and hyperaldosteronism. A prospective clinical study. Hypertension 2010; 55: 1137–1142.
Brandt MC, Mahfoud F, Reda S, Schirmer SH, Erdmann E, Böhm M, Hoppe UC . Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol 2012; 59: 901–909.
Brandt MC, Reda S, Mahfoud F, Lenski M, Böhm M, Hoppe UC . Effects of renal sympathetic denervation on arterial stiffness and central hemodynamics in patients with resistant hypertension. J Am Coll Cardiol 2012; 60: 1956–1965.
Townsend RR . Vascular compliance and arterial calcification: impact on blood pressure reduction. Curr Opin Nephrol Hypertens 2008; 17: 93–98.
Pickering TG . Arterial stiffness as a cause of resistant hypertension? J Clin Hypertens 2007; 9: 390–395.
Spence JD . Management of resistant hypertension in patients with carotid stenosis: high prevalence of renovascular hypertension. Cerebrovasc Dis 2000; 10: 249–254.
Schmieder RE, Schmidt BM, Raff U, Bramlage P, Dörfler A, Achenbach S, Schwab J, Kolominsky-Rabas P . Cerebral microangiopathy in treatment-resistant hypertension. Clin Hypertens 2011; 13: 582–587.
Figueiredo VN, Yugar-Toledo JC, Martins LC, Martins LB, de Faria AP, de Haro Moraes C, Sierra C, Coca A, Moreno H . Vascular stiffness and endothelial dysfunction: correlations at different levels of blood pressure. Blood Press 2012; 21: 31–38.
Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, Demacq C, Pimenta E, Calhoun DA, Moreno H Jr . Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens 2011; 25: 532–538.
Rizzoni D, Porteri E, Boari GE, De Ciuceis C, Sleiman I, Muiesan ML, Castellano M, Miclini M, Agabiti-Rosei E . Prognostic significance of small-artery structure in hypertension. Circulation 2003; 108: 2230–2235.
Rizzoni D, Porteri E, Castellano M, Bettoni G, Muiesan ML, Muiesan P, Giulini SM, Agabiti Rosei E . Vascular hypertrophy and remodeling in secondary hypertension. Hypertension 1996; 28: 785–790.
Rizzoni D, Paiardi S, Rodella L, Porteri E, De Ciuceis C, Rezzani R, Boari GE, Zani F, Miclini M, Tiberio GA, Giulini SM, Rosei CA, Bianchi R, Agabiti Rosei E . Changes in extracellular matrix in subcutaneous small resistance arteries of patients with primary aldosteronism. J Clin Endocrinol Metab 2006; 91: 2638–2642.
Schiffrin EL, Deng LY, Sventek P, Day R . Enhanced expression of endothelin-1 gene in resistance arteries in severe human essential hypertension. J Hypertens 1997; 15: 57–63.
Muxfeldt ES, Bloch KV, Nogueira Ada R, Salles GF . True resistant hypertension: is it possible to be recognized in the office? Am J Hypertens 2005; 18: 1534–1540.
Raff U, Harazny JM, Titze SI, Schmidt BM, Michelson G, Schmieder RE . Salt intake determines retinal arteriolar structure in treatment resistant hypertension independent of blood pressure. Atherosclerosis 2012; 222: 235–240.
Nogueira Ada R, Fernandes AS, Coutinho ES, Salles GF, Muxfeld ES, Bloch KV . Factors associated with microalbuminuria in resistant hypertension. Int J Cardiol 2007; 121: 86–87.
Raff U, Schmidt BM, Schwab J, Schwarz TK, Achenbach S, Bär I, Schmieder RE . Renal resistive index in addition to low-grade albuminuria complements screening for target organ damage in therapy-resistant hypertension. J Hypertens 2010; 28: 608–614.
Oliveras A, Armario P, Martell-Clarós N, Ruilope LM, de la Sierra A, Spanish Society of Hypertension-Resistant Hypertension Registry. Urinary albumin excretion is associated with nocturnal systolic blood pressure in resistant hypertensives. Hypertension 2011; 57: 556–560.
Barbato A, Galletti F, Iacone R, Cappuccio FP, Rossi G, Ippolito R, Venezia A, Farinaro E, Strazzullo P . Predictors of resistant hypertension in an unselected sample of an adult male population in Italy. Intern Emerg Med 2012; 7: 343–351.
Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES . Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis 2011; 216: 199–204.
Salles GF, Cardoso CR, Pereira VS, Fiszman R, Muxfeldt ES . Prognostic significance of a reduced glomerular filtration rate and interaction with microalbuminuria in resistant hypertension: a cohort study. J Hypertens 2011; 29: 2014–2023.
Muiesan ML, Pasini G, Salvetti M, Calebich S, Zulli R, Castellano M, Rizzoni D, Bettoni G, Cinelli A, Porteri E, Corsetti V, Agabiti-Rosei E . Cardiac and vascular structural changes. Prevalence and relation to ambulatory blood pressure in a middle-aged general population in northern Italy: the Vobarno Study. Hypertension 1996; 27: 1046–1052.
Muiesan ML, Salvetti M, Zulli R, Pasini GF, Bettoni G, Monteduro C, Rizzoni D, Bettoni G, Cinelli A, Porteri E, Corsetti V, Agabiti-Rosei E . Structural association between the carotid artery and the left ventricle in a general population in Northern Italy: the Vobarno study. J Hypertens 1998; 16 (Pt 1): 1805–1812.
Muiesan ML, Salvetti M, Paini A, Monteduro C, Rosei CA, Aggiusti C, Belotti E, Bertacchini F, Galbassini G, Stassaldi D, Castellano M, Rosei EA . Pulse wave velocity and cardiovascular risk stratification in a general population: the Vobarno study. J Hypertens 2010; 28: 1935–1943.
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, Alderman MH . Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992; 20: 1251–1260.
Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Cifkova R, Clément D, Coca A, Dominiczak A, Erdine S, Fagard R, Farsang C, Grassi G, Haller H, Heagerty A, Kjeldsen SE, Kiowski W, Mallion JM, Manolis A, Narkiewicz K, Nilsson P, Olsen MH, Rahn KH, Redon J, Rodicio J, Ruilope L, Schmieder RE, Struijker-Boudier HA, Van Zwieten PA, Viigimaa M, Zanchetti A . Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens 2009; 27: 2121–2158.
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace-Raso FU, Protogerou AD, Schillaci G, Segers P, Vermeersch S, Weber T . Artery Society; European Society of Hypertension Working Group on Vascular Structure and Function; European Network for Noninvasive Investigation of Large Arteries. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens 2012; 30: 445–448.
Persell SD . Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 2011; 57: 1076–1080.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muiesan, M., Salvetti, M., Rizzoni, D. et al. Resistant hypertension and target organ damage. Hypertens Res 36, 485–491 (2013). https://doi.org/10.1038/hr.2013.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.30
Keywords
This article is cited by
-
Revisiting the diagnosis of ‘resistant hypertension’: what should we do nowadays’
Journal of Human Hypertension (2022)
-
The effect of resistant hypertension on in-hospital mortality in patients hospitalized with COVID-19
Journal of Human Hypertension (2022)
-
Machine learning approach to predict subtypes of primary aldosteronism is helpful to estimate indication of adrenal vein sampling
High Blood Pressure & Cardiovascular Prevention (2022)
-
A New Minimally Invasive Method of Transverse Aortic Constriction in Mice
Journal of Cardiovascular Translational Research (2022)
-
Clinical Outcomes in OSA—SLEEP GOAL—a More Holistic Approach
Current Otorhinolaryngology Reports (2019)