Abstract
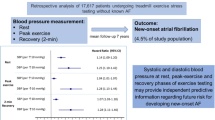
The relationship between blood pressure (BP) response during exercise and future cardiovascular events remains unclear. We assessed the association between an increase in early systolic BP (SBP) during exercise tests and future cardiovascular events in patients with sustained hypertension (sHT). Between 2002 and 2005, we enrolled 300 patients newly diagnosed with mild-to-moderate sHT without complications from the Asan Ambulatory Blood Pressure Monitoring registry. All the patients successfully performed treadmill tests, achieving target heart rate according to the Naughton/Balke protocol. The patients were divided into quartiles according to their SBP at 8 min (7.4 metabolic equivalent tasks). The primary outcome was the composite of all-cause death, new-onset ischemic heart disease and stroke. The 5-year survival rates did not differ significantly among quartiles 1–4 (100% vs. 96.6% vs. 94.4% vs. 98.3%, P=0.211). Relative to quartile 1, the 5-year event-free survival rates were significantly lower in patients in quartiles 3 (86.9% vs. 98.3%, P=0.023) and 4 (88.2% vs. 98.3%, P=0.023). After multivariable adjustment for covariates, the risk for the composite end point was higher for patients in quartiles 3 (Hazard ratio (HR) 4.69, 95% confidence interval (CI) 1.28–17.13, P=0.020) and 4 (HR 3.65, 95% CI 0.92–14.50, P=0.065) than in quartiles 1 and 2. Cardiovascular risk was significantly higher in patients with stage 4 SBP (>180 mm Hg) even after adjustment (HR 4.00, 95% CI 1.19–13.44, P=0.025). Increased submaximal SBP response to exercise may be a predictor of future cardiovascular events in patients with mild-to-moderate sHT.
Similar content being viewed by others
Introduction
Although the exercise tolerance test (ETT) has been widely used in clinical practice, the value of blood pressure (BP) response to ETT remains unclear,1, 2, 3, 4, 5, 6, 7, 8, 9, 10 especially regarding the relationship between BP response during exercise and future cardiovascular events. The current guidelines include exercise-induced hypertension as a marker for future hypertension but not for cardiovascular morbidity and mortality outcomes.11, 12 Several recent studies have shown that BP response at submaximal rather than at maximal workload was associated with future cardiovascular disease (CVD) in normotensive patients,6, 8, 10 but the prognostic value of BP response during ETT in hypertensive patients has not yet been determined. At our center, a diagnosis of hypertension is based on 24-h ambulatory blood pressure monitoring (ABPM), with ETT using the Naughton/Balke protocol utilized for cardiac rehabilitation and risk stratification. Because almost all the patients in our registry, the Asan-ABPM registry, underwent ETT at initial evaluation, we assessed the prognostic value of submaximal systolic BP (SBP) response during exercise for future cardiovascular events in patients with mild-to-moderate sustained hypertension (sHT) diagnosed by 24-h ABPM.
Methods
We enrolled patients aged ⩾18 years who were registered in the Asan-ABPM registry between May 2002 and October 2005. Patients were excluded if they had a history of coronary artery disease or stroke at the time of hospital visit, symptomatic congestive heart failure or failed to achieve the target heart rate. Of the 1017 patients screened, 886 (87.1%) were taking antihypertensive medications at the time of ETT, whereas 131 (12.9%) were not. We identified 541 patients diagnosed with sHT by ABPM. We excluded 190 patients who had not achieved target heart rate, 42 with previous ischemic heart disease (IHD) or stroke and 9 with stage 3 hypertension. Therefore, our study population consisted of 300 patients with sHT (Figure 1). The study protocol was approved by the Ethical Committee of our institution.
All the patients receiving antihypertensive medications were asked to discontinue them for at least five half-lives of the drug. Clinical BPs were measured by the physician investigators using a mercury sphygmomanometer, with SBP and diastolic BP (DBP) at rest measured in the left brachial artery after at least 5–10 min of rest, with two readings taken 5 min apart. Ambulatory BP was measured using 24-h ABPM with a portable SpaceLabs 90207 (Issaquah, WA, USA) noninvasive recorder with a BP cuff fitted on the nondominant arm. The unit was programmed to record BP and heart rate at 15-min intervals from 0600 to 2200 hours (daytime period) and at 30-min intervals from 2200 to 0600 hours (night period); awake and asleep periods were calculated from diary entries. sHT was defined as a daytime BP ⩾135/85 mm Hg and a night BP ⩾120/70 mm Hg.12
We also assessed the clinical and family history of each patient, as well as the results of physical examination, laboratory parameters, echocardiography and exercise treadmill tests. We also calculated the Framingham general cardiovascular risk score for each patient.13
ETTs were performed using a symptom-limited Naughton/Balke treadmill protocol. Attainment of 85% of target heart rates (age- and sex-predicted maximal heart rate) was considered adequate. Target heart rates were not considered predetermined end points, rather subjects underwent symptom-limited treadmill tests. Throughout the ETT, BP and heart rate were measured using a SunTech Medical Tango BP monitoring system (Raleigh, NC, USA), with baseline measurements taken with the subject at rest in a sitting position prior to exercise. Heart rate (HR) was monitored continuously using a 12-lead echocardiogram. SBP and DBP were measured by auscultation for 30 s before the end of each 2-min incremental stage. Multi-lead ECG recordings were taken at rest and at the same interval until the end of the recovery period to exclude ischemia or arrhythmia. Exercise capacity was calculated as the total metabolic equivalent tasks achieved. All the patients were categorized into quartiles based on their absolute value of SBP response at stage 4 of the Naughton/Balke treadmill protocol (7.4 metabolic equivalent tasks). We also assessed DBP at stage 4 and SBP and DBP at the maximal workload for each individual. If a patient was unable to reach stage 4, the highest SBP through stage 3 was used.
The primary outcome of this study was the composite of all-cause death, new-onset IHD and stroke. The cause and date of death were confirmed by information gathered from the national population registry of the Korean national statistical office, together with a review of all the available clinical records. Follow-up data were also collected by direct telephone interview and a review of medical records. IHD was diagnosed in patients with typical angina symptoms and positive results on at least one stress test (ETT, thallium scan or dobutamine stress echocardiography). Stroke was diagnosed by an independent neurologist based on brain imaging. The patients were followed for a median of 66 months (interquartile range 34–79 months).
All the statistical analyses were performed using SPSS (version 18.0; SPSS Inc, Chicago, IL, USA). Summary statistics are presented as frequencies and percentages, mean±s.d. or medians with interquartile ranges. Between-group differences in continuous variables were assessed by analysis of variance and turkey’s tests, whereas between-group differences in the frequency of categorical variables were assessed using the Chi-square or Fisher’s exact tests, as appropriate. Relationship between BP variables measured during ETT was evaluated by calculation of Spearman’s rank correlation coefficient. Cumulative survival and event-free rate curves were calculated by the Kaplan–Meier method and compared using the log-rank test. We used three-step adjustment using Cox proportional hazard models to adjust for confounding variables. In model 1, unadjusted HR was adjusted for resting SBP and DBP during ETT. In model 2, HR was further adjusted for Framingham general cardiovascular risk score and other confounding variables were adjusted in model 3. All P-values were two-sided, and P<0.05 was considered statistically significant.
Results
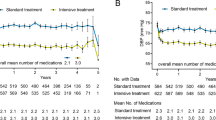
The study participants were middle aged (mean 50.4±11.17 years old) with more men (56.7%) included (Table 1). The 300 participants showing SBP increases during exercise were divided into quartiles based on their BP responses at stage 4 of the ETT. The clinical and exercise characteristics of the study population are shown in Table 2. Compared with participants who had the lowest quartile of SBP increases, those with increases in the highest quartile were older, had higher body mass index and Framingham scores, as well as had higher clinical SBP, DBP and night SBP. During ETT, patients in quartile 4 showed the earliest target-HR achievement and lowest exercise capacity. There was no significant difference in alcohol consumption, smoking history and lipid profile across the quartiles. Distributions of BP responses during exercise are shown in Table 3. Participants in the highest quartile showed a greater increase in SBP and a lesser decrease in DBP at submaximal and maximal exercise BP. In the correlation matrix (Table 4), the absolute value of stage 4 SBP showed strong positive correlation with the change of SBP at stage 4 (r=0.791, P=0.001) and the absolute SBP value at maximal workload (r=0.680, P=0.001), whereas relationship with the DBP variables were weaker.
Unadjusted survival analysis using the Kaplan–Meier method showed that the 5-year overall survival rate did not differ significantly among quartiles 1–4 (100% vs. 96.6% vs. 94.4% vs. 98.3%, P=0.211). However, there was a trend of lower 5-year event-free survival rate in a higher quartile (98.3% vs. 95.0% vs. 88.2% vs. 86.9%, P=0.064). Compared with patients in quartile 1, the 5-year event-free survival rate was significantly lower for patients in quartiles 3 (86.9% vs. 98.3%, P=0.022) and 4 (88.2% vs. 98.3%, P=0.023). The details of composite outcomes are described in Table 5. During 5 years, more cardiovascular events occurred in a higher quartile (1.3% vs. 3.9% vs. 10.3% vs. 9.9%, P=0.028) and the difference in event-free survival was mainly driven by new-onset IHD.
Results of multivariable models relating exercise BP to the composite risk of death, IHD and stroke are shown in Table 6. After adjusting for resting SBP and DBP, we found that, compared with patients in quartiles 1 and 2, those in quartiles 3 (HR 4.52, 95% confidence interval (CI) 1.33–15.29, P=0.015) and 4 (HR 5.16, 95% CI 1.42–18.88, P=0.013) were at significantly higher risk of composite outcomes (see Table 6). These differences remained significant after adjusting for Framingham risk scores. In Model 3, even after adjustment for known risk factors, exercise capacity and ABPM data, patients in quartiles 3 and 4 tended to have higher risks of composite outcomes than those in quartile 1, however, the difference was not significant for those in quartile 4. However, when assessing quartiles as a continuous variable, multivariate analysis models showed that each 8-min SBP increment was associated with an increase in HR of 1.76 (95% CI 1.12–2.78, P=0.010), which remained significant after adjusting for resting SBP, DBP, Framingham score and all the other variables. (HR 1.74, 95% CI 1.04–2.89, P=0.035). Further analysis comparing 8-min SBP >180 (upper 50% of total population) and ⩽180 mm Hg (lower 50% of total population) showed that the former group was at significantly increased risk of composite end points (HR 3.74, 95% CI 1.24–11.28, P=0.019), even after adjustment for all the other variables (HR 4.00, 95% CI 1.19–13.44, P=0.025).
Discussion
The most important finding of this study of patients with uncomplicated mild-to-moderate sHT was that those in higher quartiles were associated with higher risk of the composite end point in unadjusted analysis. During ETT, patients in higher quartiles showed greater incremental increases in SBP and lower decrements in DBP. Clinically, patients in higher quartiles had higher daytime and night SBP during ABPM, as well as more risk factors for CVD, including higher Framingham score and body mass index and lower exercise capacity. Moreover, patients in higher quartiles were at high risk of the composite end point, even after adjustment for known CVD risk factors.
Although most prior studies focused on peak SBP at maximal workload,1, 3, 4, 7, 9, 10 we considered SBP at submaximal workload in the Naughton/Balke protocol as more valuable for several reasons. First, because submaximal workload was easily achieved by patients with lower exercise capacity, we could include representative data from more patients. Second, because the Naughton/Balke protocol used smaller increments in workload, this protocol could more accurately portray functional capacity than the Bruce protocol, as well as minimizing contamination by mental factors. Third, we regarded data from a treadmill test as more valuable than data from a bicycle ergometer because maximal oxygen uptake is generally lower on the latter.14 Moreover, because the legs of individuals from east Asia are usually shorter than those of Caucasians, a bicycle ergometer may underestimate the exact workload of exercise. In addition, all of our patients underwent ABPM monitoring at the beginning of treatment, thus, confirming sHT and allowing ABPM data to be integrated into multivariate analysis models. As a result, our study included a homogeneous group of patients with mild-to-moderate sHT relevant to clinical practice, allowing the independent prognostic value of ETT results to be determined.
Large population studies have shown an association between SBP response during submaximal ETT and CVD. For example, the relationship between submaximal SBP and cardiovascular mortality was assessed in normotensive patients using a bicycle ergometer.10 That study showed that 6-min SBP, representing 55% of the mean exercise capacity of the entire population, was associated with cardiovascular mortality after multivariate adjustment, a finding consistent with our results despite our inclusion of only hypertensive patients. In addition, a study of >6000 patients found an association between Bruce stage 2 SBP ⩾180 mm Hg and future CVD in non-hypertensive patients.8 In extending these findings to hypertensive patients, we found that a greater increase in BP was associated with higher morbidity and mortality rates and was a clinical risk factor for CVD.
The mechanism underlying the association between exercise SBP response and CVD has not yet been determined. In healthy patients, an increase in cardiac output is usually accompanied by an increase in SBP, but may be attenuated by adaptive vasodilatation of peripheral vessels.15 An exaggerated SBP response during ETT has been regarded as a consequence of mismatching between these two mechanisms. Interestingly, outcomes in our patients were exactly the opposite of that in patients with known IHD, in that exaggerated exercise SBP had protective effects on outcomes, which may be associated with better cardiac output augmentation.2, 16 Because we excluded patients with impaired cardiac output augmentation, impaired adaptive vasodilatation may be a more important mechanism in our study. Several studies have shown a relationship between impaired vasodilatation and greater BP response.17, 18, 19, 20 This mechanism may be reflected in the characteristics of the BP response in the patients in higher quartiles of the present study, including greater SBP increment and reduced DBP decrement, despite lower exercise capacity, higher daytime and night SBP during ABPM monitoring. A continuous exposure to high BP during daily activity may lead to a high CVD rate for patients in the upper quartiles.21, 22, 23
In addition to their differing SBP response, the differences in baseline characteristics among patients in different quartiles may have affected the clinical outcomes. Patients in higher quartiles were older, had higher body mass index and clinical and ABPM BP, and lower exercise capacity than those in lower quartiles. In particular, the Framingham general CVD score, a strong prognostic factor, was significantly higher for patients in quartile 4.13 The submaximal ETT response among our patients was well correlated with their general CVD risk factors, resulting in differences in primary outcomes on unadjusted survival analysis. Thus, in addition to being an independent prognostic factor, higher SBP response during ETT may itself be a marker of future CVD risk.
The primary limitations of our study were the relatively small patient cohort and short follow-up period, resulting in a relatively low incidence of clinical events. The limitation in cohort size was mainly due to the exclusion of patients with pre-existing CVD and those at high risk of CVD. A follow-up period of 5 years may be too short to show the clinical significance in patients at mild-to-moderate risk. To overcome the limited numbers of patients and observed events, we had to use the Framingham risk score as a surrogate marker of many cardiovascular risk factors such as age, sex, smoking status and lipid profiles. As a result, age and sex itself were not included in our three-step models because of the limited number of observed events and multicollinearity. And we had to summate the quartiles 1 and 2 as a reference to calculate the HR of quartiles 3 and 4. However, our exclusion criteria enabled our assessment of new CVD in a homogeneous patient group, and these patients could be intensively followed-up because the study was performed in a single center. Because some of our patients may have become fatigued before reaching their maximal exercise capacities, we may have underestimated maximal BP. However, the submaximal SBP we observed was likely correct because almost all of the patients exercised for more than stage 4.
Conclusion
In conclusion, the submaximal SBP response at stage 4 (8 min) of the Naughton/Balke protocol may be a good predictor of future cardiovascular events in patients with mild-to-moderate sHT. And patients with stage 4 SBP >180 mm Hg were at significantly higher cardiovascular risk, even after adjustment for other risk factors, than those with lower SBP.
References
Allison TG, Cordeiro MA, Miller TD, Daida H, Squires RW, Gau GT . Prognostic significance of exercise-induced systemic hypertension in healthy subjects. Am J Cardiol 1999; 83: 371–375.
Bouzas-Mosquera A, Peteiro J, Broullon FJ, Alvarez-Garcia N, Garcia-Bueno L, Mosquera VX, Prada O, Casas S, Castro-Beiras A . Prognostic value of an exaggerated exercise blood pressure response in patients with diabetes mellitus and known or suspected coronary artery disease. Am J Cardiol 2010; 105: 780–785.
Fagard R, Staessen J, Thijs L, Amery A . Prognostic significance of exercise versus resting blood pressure in hypertensive men. Hypertension 1991; 17: 574–578.
Filipovsky J, Ducimetiere P, Safar ME . Prognostic significance of exercise blood pressure and heart rate in middle-aged men. Hypertension 1992; 20: 333–339.
Habibzadeh MR, Farzaneh-Far R, Sarna P, Na B, Schiller NB, Whooley MA . Association of blood pressure and heart rate response during exercise with cardiovascular events in the heart and soul study. J Hypertens 2010; 28: 2236–2242.
Lewis GD, Gona P, Larson MG, Plehn JF, Benjamin EJ, O'Donnell CJ, Levy D, Vasan RS, Wang TJ . Exercise blood pressure and the risk of incident cardiovascular disease (from the framingham heart study). Am J Cardiol 2008; 101: 1614–1620.
Mundal R, Kjeldsen SE, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Exercise blood pressure predicts cardiovascular mortality in middle-aged men. Hypertension 1994; 24: 56–62.
Weiss SA, Blumenthal RS, Sharrett AR, Redberg RF, Mora S . Exercise blood pressure and future cardiovascular death in asymptomatic individuals. Circulation 2010; 121: 2109–2116.
Mundal R, Kjeldsen SE, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Exercise blood pressure predicts mortality from myocardial infarction. Hypertension 1996; 27: 324–329.
Kjeldsen SE, Mundal R, Sandvik L, Erikssen G, Thaulow E, Erikssen J . Supine and exercise systolic blood pressure predict cardiovascular death in middle-aged men. J Hypertens 2001; 19: 1343–1348.
Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O'Reilly MG, Winters WL, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Russell RO, Smith SC . ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the american college of cardiology/american heart association task force on practice guidelines (committee to update the 1997 exercise testing guidelines). Circulation 2002; 106: 1883–1892.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC task force on the management of arterial hypertension. J Hypertens 2007; 25: 1751–1762.
D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB . General cardiovascular risk profile for use in primary care: The framingham heart study. Circulation 2008; 117: 743–753.
Myers J, Arena R, Franklin B, Pina I, Kraus WE, McInnis K, Balady GJ . Recommendations for clinical exercise laboratories: A scientific statement from the american heart association. Circulation 2009; 119: 3144–3161.
Francis GS. . Hemodynamic and neurohumoral responses to dynamic exercise: normal subjects versus patients with heart disease. Circulation 1987; 76: VI11–VI17.
Campbell L, Marwick TH, Pashkow FJ, Snader CE, Lauer MS . Usefulness of an exaggerated systolic blood pressure response to exercise in predicting myocardial perfusion defects in known or suspected coronary artery disease. Am J Cardiol 1999; 84: 1304–1310.
Tzemos N, Lim PO, MacDonald TM . Is exercise blood pressure a marker of vascular endothelial function? QJM 2002; 95: 423–429.
Stewart KJ, Sung J, Silber HA, Fleg JL, Kelemen MD, Turner KL, Bacher AC, Dobrosielski DA, DeRegis JR, Shapiro EP, Ouyang P . Exaggerated exercise blood pressure is related to impaired endothelial vasodilator function. Am J Hypertens 2004; 17: 314–320.
Tzemos N, Lim PO, MacDonald TM . Exercise blood pressure and endothelial dysfunction in hypertension. Int J Clin Pract 2009; 63: 202–206.
Otsuki T, Maeda S, Kesen Y, Yokoyama N, Tanabe T, Sugawara J, Miyauchi T, Kuno S, Ajisaka R, Matsuda M . Age-related reduction of systemic arterial compliance induces excessive myocardial oxygen consumption during sub-maximal exercise. Hypertens Res 2006; 29: 65–73.
Kikuya M, Ohkubo T, Asayama K, Metoki H, Obara T, Saito S, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y . Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality: The ohasama study. Hypertension 2005; 45: 240–245.
Suzuki Y, Kuwajima I, Aono T, Kanemaru A, Nishinaga M, Shibata H, Ozawa T . Prognostic value of nighttime blood pressure in the elderly: A prospective study of 24-hour blood pressure. Hypertens Res 2000; 23: 323–330.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, Den Hond E, McCormack P, Staessen JA, O'Brien E . Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: The dublin outcome study. Hypertension 2005; 46: 156–161.
Acknowledgements
We would like to thank Seung-Bong Han, PhD, for providing excellent assistance in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Cho, M., Jang, SJ., Lee, C. et al. Association of early systolic blood pressure response to exercise with future cardiovascular events in patients with uncomplicated mild-to-moderate hypertension. Hypertens Res 35, 922–927 (2012). https://doi.org/10.1038/hr.2012.52
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.52
Keywords
This article is cited by
-
Higher blood pressure during light exercise is associated with increased left ventricular mass index in normotensive subjects
Hypertension Research (2018)
-
Renal denervation improves exercise blood pressure: insights from a randomized, sham-controlled trial
Clinical Research in Cardiology (2016)