Abstract
Elevated blood pressure (BP) during childhood and adolescence increases the risk of hypertension in later life. Although physical activity is known to positively moderate BP, data regarding this relationship are limited in prepubertal children. We aimed to assess the association between a range of physical activities (including indoor and outdoor activity) and BP in a large community-based sample of prepubertal schoolchildren. Eligible year-1 schoolchildren (n=1765; mean age 6.7±0.4 years) from a random cluster sample of 34 schools in Sydney, Australia, were examined. Parents completed detailed questionnaires about their child's activity. Height and weight were measured, and body mass index (BMI) was calculated. BP was measured using a standard protocol, and elevated BP was defined using published guidelines. Physical activity was classified as low, medium or high (that is, as tertiles). After adjusting for age, sex, ethnicity, height, BMI, parental qualifications and family history of hypertension and/or cardiovascular disease, children in the highest tertile of outdoor and indoor activities had significantly lower diastolic BP (∼1.5 mm Hg; Ptrend=0.01) and systolic BP (∼1.3 mm Hg; Ptrend=0.03), respectively, compared with those in the lowest tertile (reference). Linearly, time spent in indoor activities (each hour per day) was associated with ∼2.4 mm Hg decrease in diastolic BP (P=0.001). Physical activity was independently associated with lower BP in this sample of prepubertal children. The findings emphasize the importance of ensuring regular physical activity programs in primary schools to potentially reduce the risk of elevated BP in childhood and in later life.
Similar content being viewed by others
Introduction
Elevated blood pressure (BP) during childhood and adolescence is associated with increased risk of hypertension and cardiovascular disease (CVD),1 and the development of early pathological lesions of atherosclerosis.2, 3 Thus, the recognition and management of elevated BP at an early age, and the identification of modifiable risk factors, may be an important strategy for limiting the overall public health disease burden caused by hypertension.4, 5
Physical activity is a key component of the therapeutic lifestyle changes recommended for preventing and treating elevated BP and hypertension in children and adolescence.6, 7 There is evidence that levels of physical activity, aerobic fitness and CVD risk factors track from childhood and adolescence into adulthood.8 A number of observational studies have investigated associations between physical activity and BP in children and adolescents,9, 10, 11, 12 but the findings from these studies have been equivocal. Recently, a UK study of 5505 children aged 11–12 years showed that higher levels of physical activity were associated with lower BP, and the authors concluded that the volume of activity may be more important than the intensity.10 In contrast, several studies reported no or a positive association, whereas others reported inverse associations, but not always consistently for systolic and diastolic BP in both males and females.11, 13 Moreover, although many studies have examined the association between physical activity and adiposity in younger children,14, 15 very few large population-based studies (and none conducted in Australia to date) have assessed the relationship with BP during prepuberty.
This study used a large population-based sample of Sydney schoolchildren, aged 6 years, to assess the association between indicators of physical activity (that is, outdoor and indoor activities) and BP, while controlling for potential confounders. The study is novel, as it is the first population-based study to simultaneously assess the influence of differing types of physical activity (outdoor and indoor activity) on systolic and diastolic BP in young, prepubertal children.
Methods
Study population
The Sydney Childhood Eye Study is a population-based survey of eye conditions in school children living within the Sydney Metropolitan Area, New South Wales, Australia. It was approved by the Human Research Ethics Committee, University of Sydney, the NSW Department of Education and Training, and the Catholic Education Office. We obtained informed written consent from at least one parent of each child, as well as verbal assent from every child before the examinations. Study methods have been previously described.16 Year-1 students were selected from a stratified random cluster sample of 34 primary schools across Sydney (mean age 6.7 years, hereafter referred to as the 6-year-old sample). Stratification was based on socioeconomic status data from the Australian Bureau of Statistics (available at http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012006?OpenDocument), and included a proportional mix of public, private and religious primary schools. Data were collected by trained field officers at schools during 2003 and 2004.
Assessment of physical activity
Information on the children's physical activity and sedentary behaviors was reported by the child's parent because the evidence shows that children younger than 9–10 years do not have the cognitive capacity to recall or assess their physical activity and sedentary behavior.17, 18, 19 The questions relating to physical activity comprised a list of nine common activities in which early primary school-aged children participate: (a) dancing, gymnastics and calisthenics; (b) athletics; (c) swimming; (d) football, soccer, rugby league and Australian football; (e) netball and basketball; (f) tennis; (g) Kanga cricket (modified Australian version of cricket for children); (h) skating, riding a scooter and rollerblading; and (i) baseball and softball. Parents were asked to report the number of hours per week their child spent in each activity, and whether the activity was done outdoors or indoors (hall gym and classroom). The time spent in each activity was summed, and the average hours per day spent were calculated separately for outdoor activities, indoor activities and the total activity time (that is, sum of outdoor and indoor activities).
BP measurements
BP was measured on the school premises according to a standard protocol.16 After 5 min of resting, BP was measured in a seated position using an automated sphygmomanometer (HEM 907; Omron Healthcare, Bannockburn, IL, USA) with appropriate cuff size. We followed general recommendations on selecting cuff size to ensure that the bladder length was ∼80% and width was ⩾40% of the arm circumference, covering the upper arm without obscuring the antecubital fossa.20 Three separate BP measurements were taken, and averaged for analysis. Mean arterial BP was calculated as one-third of the systolic BP plus two thirds of the diastolic BP. The children were categorized as having ‘high BP’ by computing specific systolic and diastolic BP percentiles, adjusted for height, age and sex, using the formulae in Appendix B of the 2004 US ‘Fourth Report on the Diagnosis, Evaluation, and Treatment of High BP in Children and Adolescents’.21, 22 Briefly, the most recent Centers for Disease Control growth charts were used to convert the height to a height z-score relative to boys and girls of the same age.22 Additionally, regression coefficients from BP regression models (provided in the fourth report) were used to compute the specific systolic and diastolic BP percentiles for boys and girls separately.21 High BP was then defined as systolic and/or diastolic BP ⩾95th percentile.21
Collection of other information
Parents were asked to provide comprehensive sociodemographic information on behalf of their children, including ethnicity, country of birth and education. Parents were asked whether the biological mother and/or father have had or currently have hypertension and/or heart disease. If they answered yes to either question, then the child was considered as having a family history of hypertension and/or CVD. We defined parental education as the highest level of education completed by either parent. This ranged from never having attended school to having completed a higher degree such as a Masters or PhD. The ethnicity of the child was determined only if both parents shared that ethnic origin. Ethnicity was classified on the basis of self-identification by the parents, combined with information about the place of birth of the child. Ethnic categories were consistent with the Australian Standard Classification of Cultural and Ethnic groups (available at http://www.abs.gov.au, document number 1249.0).23
Each child's weight was measured, and height was measured with shoes off using a freestanding SECA height rod (Model 220, Hamburg, Germany). Weight in kilograms was measured using a standard portable weighing machine after removal of any heavy clothing. Body mass index (BMI) was calculated as weight divided by height squared (kg m−2).
Statistical analysis
Statistical analyses were performed using SAS (SAS v8.2, SAS Institute, Cary, NC, USA). We used mixed models, and generalized estimating equations were used to adjust for cluster-sampling effects. Time spent in physical activity, including outdoor and indoor activities and total physical activity, was either analyzed as categorical (that is, tertiles) or continuous variables (that is, each hour per day). Regression models were used to examine possible linear relationships between physical activity time (that is, total physical activity, outdoor and indoor activities) and BP levels. Multivariate modeling was conducted with BP as the outcome and the types of physical activity (hours per day) as the independent variable in linear models adjusted for age, sex, ethnicity, height, BMI, parental education and family history of hypertension and/or CVD. Analysis of covariance was used to assess differences in mean systolic and diastolic BP measures stratified by tertiles of physical activity (low, medium and high). Multivariable logistic regression analysis was used to calculate adjusted odds ratios and 95% confidence intervals for associations between physical activity and elevated/high BP. Significance was taken as P<0.05.
Results
Of 2238 eligible children, 1765 children were given parental permission to participate and 1741 underwent examination (77.7%). Of these, 1426 had information on both physical activity and BP measures. Table 1 shows the characteristics of participants by tertiles of total physical activity levels. The mean age of children was 6.7 years (±0.4); 51.7% were boys and 68.5% were Caucasians. Children in the highest tertile of total physical activity were more likely to be Caucasian, have a family history of hypertension and/or CVD, and have a higher body weight and BMI compared with children in the lowest tertile of total physical activity. Mean time spent in hours per day (±s.d.) in: total physical activity was 0.6 (±0.6), outdoor activity was 0.5 (±0.6) and indoor activity was 0.1 (±0.2).
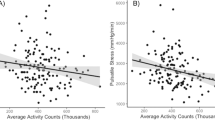
Table 2 shows the unadjusted and adjusted associations between the type of physical activity (in tertiles) and systolic and diastolic BP. Six-year-old children in the highest tertile of outdoor activity had significantly lower diastolic BP (that is, a decrease of 1.5 mm Hg) than those in the lowest tertile of activity after adjusting for age, sex, ethnicity, height, BMI, parental education and family history of hypertension and/or CVD, Ptrend=0.01 (Table 2). A significant decrease in diastolic BP was also observed with increasing time spent in total physical activity, Ptrend=0.02. Similarly, children in the highest tertile of indoor activities had significantly lower systolic BP compared with children in the lowest tertile, Ptrend=0.03. Significant associations were not observed between tertiles of physical activity and mean arterial BP (data not shown).
Table 3 shows that for each hour per day spent in total physical activity, diastolic BP decreased by 1.01 mm Hg, and there was a significant association between time spent in total physical activity and mean arterial BP (P=0.04). Similarly, for each hour per day spent in indoor activities, there was a 2.35 and 2.15 mm Hg decrease in diastolic BP (P=0.001) and mean arterial BP (P=0.004), respectively.
Among 6-year-old children, there was a significant association between indoor activities (assessed continuously) and elevated BP (as classified by the fourth report21) after adjusting for age, sex, ethnicity, height, BMI, parental qualifications and family history of hypertension and/or CVD, odds ratio 0.50 (95% confidence interval 0.27–0.92), P=0.03. There was no significant association between total physical activity and elevated BP, multivariable-adjusted odds ratio 1.01 (95% 0.79–1.28). Significant associations were also not observed with outdoor activities (P=0.50).
Discussion
The potential value of long-term approaches to hypertension control based on moderating BP in children is increasingly recognized.24 The findings from this representative population-based sample of 6-year-old children indicate that increased time spent in outdoor activities was significantly and inversely associated with diastolic BP, whereas increased time spent in indoor activities was associated with lower systolic BP and a 50% reduced likelihood of having elevated BP.
The magnitude of change in diastolic and systolic BP (∼1.4 mm Hg) with increasing levels of physical activity is relatively similar to that observed in other childhood studies. For example, the Avon Longitudinal Study of Parents and Children10 demonstrated a 1.6 mm Hg decrease in diastolic BP with increasing total physical activity in children aged 11–12 years. Similarly, the Child Heart And health Study in England showed a 1.37 mm Hg decrease in diastolic BP with an increase in physical activity among 9- to 10-year-old Caucasians compared with other ethnicities.25 Given that the current findings are based on an even younger cohort of children, suggests that interventions to promote increased physical activity among prepubertal children could have direct positive health effects. Further, because lifestyle behaviors are established early in life, programs that encourage greater physical activity among young children have the potential to promote lifelong participation in physical activity. Successful strategies to increase early primary school children's physical activity include playground markings and games that focus on developing their fundamental movement skills, which are the building blocks for many physical activities.26, 27
A key finding of this study, not previously examined, was the differing association between the type of physical activity and systolic and diastolic BP in young children. The physiological differences between systolic and diastolic BP are likely to be the underlying mechanisms for the difference in associations with physical activity. For example, unlike systolic BP, diastolic pressure remains similar in brachial and central arteries during exercise.28 Further, it was previously reported that systolic BP is affected by changes in peripheral vascular resistance to a much lesser extent than diastolic BP, which was shown to be consistent with the lack of association between metabolic factors influencing vascular reactivity and changes to systolic BP.28 In addition, the underlying differences between indoor and outdoor activities could influence the association with BP differently. Although studies have shown that outdoor physical activity among children is associated with higher physical activity,29, 30 no study to date has examined the differences in the level of energy expenditure between indoor and outdoor activities among prepubertal children. Potentially, the underlying differences in the intensity of participating in indoor and outdoor activities could differentially influence systolic and diastolic BP. For example, the nature of indoor activities (for example, basketball) compared with outdoor sports (for example, soccer) may involve shorter sessions of more intense activity because indoor sports are typically played on smaller areas so that participants cover less total distance.
It has been hypothesized that the association between physical activity and BP may be mediated partially or wholly by the effects of physical activity on obesity.25 However, in this sample of 6-year olds, the influence of physical activity on BP appears to be, at least, partly independent of BMI. This suggests, in keeping with data from two other UK studies,10, 25 that other biological mechanisms could explain some of the beneficial effects of increased physical activity on BP during childhood, and perhaps to a lesser degree on CVD risk later in adolescence and/or adulthood.25 To this extent, a number of direct mechanisms have been hypothesized for the BP-lowering effects of physical activity, such as neurohumoral, vascular and structural adaptations.10, 31 Decreases in catecholamines and total peripheral resistance, improved insulin sensitivity and alterations in vasodilators and vasoconstrictors are some of the postulated pathways for the antihypertensive effects of physical activity.31 Specifically, increased capillary formation may lead to increased blood flow and oxygen supply, which then leads to a reduction in BP.13 Emerging data also suggest genetic links to the BP reductions associated with acute and chronic endurance exercise.31
Assuming that the observed strength of association between physical activity and BP is causal, and that the effects of physical inactivity are reversible,25 our data indicate that increasing the time spent in total physical activity by ∼25 min per day (from the lowest to highest tertile of total activity) would lead to reduced diastolic BP (∼1.4 mm Hg). If these associations translate into those of similar magnitude in adulthood, the effects of physical activity could be of importance in public health terms.10 For example, a meta-analysis demonstrated that a reduction of 5 mm Hg in diastolic BP was associated with a decrease of at least 34% for stroke and 21% for coronary heart disease.10, 32 Together with data showing that elevated BP present in childhood is an important risk factor for future cardiovascular morbidity and mortality,1, 33, 34 our findings suggest that lower BP in prepubertal children could potentially lead to reductions in these diseases in the future. Hence, relatively cost-effective strategies such as ensuring the curriculum for children in primary school includes the mandatory 120 min per week of structured physical activity35 and that free play is promoted could potentially translate into long-term health benefits such as reducing the burden of hypertension-related complications in later life. Indeed, a Danish intervention study in 137 children aged 9–11 years demonstrated the utility of increased physical activity to reduce BP after 8 months of three additional physical education classes per week.36
Strengths of this study include its random cluster sample of a large number of representative prepubertal schoolchildren from the Sydney metropolitan region, the satisfactory response rate and the use of standardized BP measurement protocols. Moreover, these young, healthy children are largely free of known systemic CVDs, and thus, these findings are not likely to be subjected to confounding effects. A limitation was the use of parent proxy reporting rather than an objective measurement of time spent in physical and sedentary activities. The use of self-reported questionnaires in large population surveys is a common practice,37 given the costs ($US300 per unit), logistics and expertise required to use criterion measures such as accelerometers. Further, parental reports are relatively accurate in estimating time spent by their children in activities.38 Moreover, the consensus from many reviews is that self-reporting should not be used in children younger than 9–10 years, as they do not have the cognitive capacity to recall or assess their physical activity behavior,17, 18, 19 and from 9–15 years, self-reports should be used cautiously.17, 39 Second, the study design is cross-sectional, which does not permit causal inference from the observed associations. It is unlikely that BP levels would be high enough in this age group so as to lead to a reduction in physical activity levels.38 Nevertheless, a 5-year follow-up of this study is currently underway, and will provide longitudinal data on this relationship. Finally, of the target population that was not examined because parents did not give consent (22.3%), collection of information such as sociodemographic factors, anthropometric measures and BP levels were not determined because of logistic barriers. Hence, generalization of our findings to the entire population needs to be made with caution.
In summary, this large population-based study showed a significant and independent, albeit modest, association between time spent in physical activity and systolic and diastolic BP in prepubertal children. Further research incorporating both objective (for example, accelerometers) and self-report measures of physical activity is required to ascertain the differential effects of indoor versus outdoor activities on BP among young children. The study findings do, however; suggest that even moderate increases in time spent in physical activity could be a potentially important strategy to reduce the prevalence of elevated BP during prepuberty.
References
Raitakari OT, Juonala M, Kahonen M, Taittonen L, Laitinen T, Maki-Torkko N, Jarvisalo MJ, Uhari M, Jokinen E, Ronnemaa T, Akerblom HK, Viikari JS . Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 2003; 290: 2277–2283.
Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA . Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998; 338: 1650–1656.
Brion MA, Ness AR, Davey SG, Leary SD . Association between body composition and blood pressure in a contemporary cohort of 9-year-old children. J Hum Hypertens 2007; 21: 283–290.
Labarthe DR . Prevention of cardiovascular risk factors in the first place. Prev Med 1999; 29: S72–S78.
Chiolero A, Paradis G, Madeleine G, Hanley JA, Paccaud F, Bovet P . Discordant secular trends in elevated blood pressure and obesity in children and adolescents in a rapidly developing country. Circulation 2009; 119: 558–565.
Mark AE, Janssen I . Dose-response relation between physical activity and blood pressure in youth. Med Sci Sports Exerc 2008; 40: 1007–1012.
Williams CL, Hayman LL, Daniels SR, Robinson TN, Steinberger J, Paridon S, Bazzarre T . Cardiovascular health in childhood: a statement for health professionals from the Committee on Atherosclerosis, Hypertension, and Obesity in the Young (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2002; 106: 143–160.
Malina RM . Tracking of physical activity and physical fitness across the lifespan. Res Q Exerc Sport 1996; 67: S48–S57.
Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M . Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol 2009; 54: 2396–2406.
Leary SD, Ness AR, Smith GD, Mattocks C, Deere K, Blair SN, Riddoch C . Physical activity and blood pressure in childhood: findings from a population-based study. Hypertension 2008; 51: 92–98.
Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA . Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet 2006; 368: 299–304.
Ekelund U, Brage S, Froberg K, Harro M, Anderssen SA, Sardinha LB, Riddoch C, Andersen LB . TV viewing and physical activity are independently associated with metabolic risk in children: the European Youth Heart Study. PLoS Med 2006; 3: e488.
Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, Froberg K . Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS). Diabetes Care 2004; 27: 2141–2148.
Aeberli I, Kaspar M, Zimmermann MB . Dietary intake and physical activity of normal weight and overweight 6 to 14 year old Swiss children. Swiss Med Wkly 2007; 137: 424–430.
Trost SG, Kerr LM, Ward DS, Pate RR . Physical activity and determinants of physical activity in obese and non-obese children. Int J Obes Relat Metab Disord 2001; 25: 822–829.
Ojaimi E, Rose KA, Smith W, Morgan IG, Martin FJ, Mitchell P . Methods for a population-based study of myopia and other eye conditions in school children: the Sydney Myopia Study. Ophthalmic Epidemiol 2005; 12: 59–69.
Sallis J, Owen N . Physical Activity and Behavioral Medicine. Sage Publications, Thousand Oaks, CA, USA, 1999.
Saris WH . Habitual physical activity in children: methodology and findings in health and disease. Med Sci Sports Exerc 1986; 18: 253–263.
Montoye H, Kemper H, Saris WH . Measuring Physical Activity and Energy Expenditure. Human Kinetics Publishers, Champaign, IL, USA, 1996.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ . Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 2005; 45: 142–161.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114: 555–576.
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL . Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002; 109: 45–60.
ABS. Australian Standard Classification of Cultural and ethnic groups (ASCCEG). 2nd edn (1249.0), Commonwealth of Australia: Canberra, 2005, 1–134.
Jenner DA, Vandongen R, Beilin LJ . Relationships between blood pressure and measures of dietary energy intake, physical fitness, and physical activity in Australian children aged 11–12 years. J Epidemiol Community Health 1992; 46: 108–113.
Owen CG, Nightingale CM, Rudnicka AR, Sattar N, Cook DG, Ekelund U, Whincup PH . Physical activity, obesity and cardiometabolic risk factors in 9- to 10-year-old UK children of white European, South Asian and black African-Caribbean origin: the Child Heart And health Study in England (CHASE). Diabetologia 2010; 53: 1620–1630.
Nielsen G, Taylor R, Williams S, Mann J . Permanent play facilities in school playgrounds as a determinant of children's activity. J Phys Act Health 2010; 7: 490–496.
Branta C, Haubenstricker J, Seefeldt V . Age changes in motor skills during childhood and adolescence. Exerc Sport Sci Rev 1984; 12: 467–520.
Brett SE, Ritter JM, Chowienczyk PJ . Diastolic blood pressure changes during exercise positively correlate with serum cholesterol and insulin resistance. Circulation 2000; 101: 611–615.
Cooper AR, Page AS, Wheeler BW, Hillsdon M, Griew P, Jago R . Patterns of GPS measured time outdoors after school and objective physical activity in English children: the PEACH project. Int J Behav Nutr Phys Act 2010; 7: 31.
Burdette HL, Whitaker RC, Daniels SR . Parental report of outdoor playtime as a measure of physical activity in preschool-aged children. Arch Pediatr Adolesc Med 2004; 158: 353–357.
Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA . American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc 2004; 36: 533–553.
MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, Abbott R, Godwin J, Dyer A, Stamler J . Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990; 335: 765–774.
Pardee PE, Norman GJ, Lustig RH, Preud’homme D, Schwimmer JB . Television viewing and hypertension in obese children. Am J Prev Med 2007; 33: 439–443.
Berenson GS, Srnivasan SR . Cardiovascular risk factors in youth with implications for aging: the Bogalusa Heart Study. Neurobiol Aging 2005; 26: 303–307.
Cleland V, Dwyer T, Blizzard L, Venn A . The provision of compulsory school physical activity: associations with physical activity, fitness and overweight in childhood and twenty years later. Int J Behav Nutr Phys Act 2008; 5: 14.
Hansen HS, Froberg K, Hyldebrandt N, Nielsen JR . A controlled study of eight months of physical training and reduction of blood pressure in children: the Odense schoolchild study. BMJ 1991; 303: 682–685.
Wells JC, Hallal PC, Reichert FF, Menezes AM, Araujo CL, Victora CG . Sleep patterns and television viewing in relation to obesity and blood pressure: evidence from an adolescent Brazilian birth cohort. Int J Obes (Lond) 2008; 32: 1042–1049.
Martinez-Gomez D, Tucker J, Heelan KA, Welk GJ, Eisenmann JC . Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med 2009; 163: 724–730.
Sirard JR, Pate RR . Physical activity assessment in children and adolescents. Sports Med 2001; 31: 439–454.
Acknowledgements
The Sydney Myopia Study (Sydney Childhood Eye Study) was supported by the Australian National Health and Medical Research Council (Grant no. 253732); the Westmead Millennium Institute, University of Sydney; and the Vision Co-operative Research Centre, University of New South Wales, Sydney, Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gopinath, B., Hardy, L., Teber, E. et al. Association between physical activity and blood pressure in prepubertal children. Hypertens Res 34, 851–855 (2011). https://doi.org/10.1038/hr.2011.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.46
Keywords
This article is cited by
-
Physical activity and eating behaviors patterns associated with high blood pressure among Chinese children and adolescents
BMC Public Health (2023)
-
The high-intensity interval training introduced in physical education lessons decrease systole in high blood pressure adolescents
Scientific Reports (2022)
-
Impact of long-term exposure to local PM10 on children’s blood pressure: a Chinese national cross-sectional study
Air Quality, Atmosphere & Health (2018)
-
Does local ambient temperature impact children’s blood pressure? A Chinese National Survey
Environmental Health (2016)
-
Sodium Intake and Blood Pressure in Children
Current Hypertension Reports (2013)