Abstract
Inappropriately (relative to dietary Na+) elevated plasma aldosterone concentrations (PAC), or aldosteronism, have been incriminated in both the appearance of the cardiometabolic syndrome (CMS) and its progressive nature. The deleterious dual consequences of elevated PAC and dietary Na+ have been linked to several components of the CMS, including salt-sensitive hypertension. Moreover, their adverse consequences are considered to be synergistic, culminating in a pro-oxidant phenotype with oxidative injury involving the heart and systemic tissues, including peripheral blood mononuclear cells (PBMC). Our experimental studies in rats receiving aldosterone/salt treatment have identified a common pathogenic event that links aldosteronism to the induction of oxidative stress. Herein, we review these findings and the important role of excessive intracellular Ca2+ accumulation (EICA), or intracellular Ca2+ overloading, which occurs in the heart and PBMC, leading to, respectively, cardiomyocyte necrosis with a replacement fibrosis and an immunostimulatory state with consequent coronary vasculopathy. The origin of EICA is based on elevations in plasma parathyroid hormone, which are integral to the genesis of secondary hyperparathyroidism that accompanies aldosteronism and occurs in response to plasma-ionized hypocalcemia and hypomagnesemia whose appearance is the consequence of marked urinary and fecal excretory losses of Ca2+ and Mg2+. In addition, we found intracellular Ca2+ overloading to be intrinsically coupled to a dyshomeostasis of intracellular Zn2+, which together regulate the redox state of cardiac myocytes and mitochondria via the induction of oxidative stress and generation of antioxidant defenses, respectively. To validate our hypothesis, a series of site-directed, sequential pharmacological and/or nutriceutical interventions targeted along cellular–molecular cascades were carried out to either block downstream events leading to the pro-oxidant phenotype or to enhance antioxidant defenses. In each case, the interventions were found to be cardioprotective. These cumulative salutary responses raise the prospect that pharmacological agents and nutriceuticals capable of influencing extra- and intracellular Ca2+ and Zn2+ equilibrium could prevent adverse cardiac remodeling and thereby enhance the management of aldosteronism.
Similar content being viewed by others
Introduction
The clinical concurrence of diabetes mellitus, dyslipidemia, obesity and hypertension has been termed a cardiometabolic syndrome (CMS).1, 2, 3 Its pathophysiological expressions and pathogenic origins are of considerable clinical interest. In this context, inappropriately (relative to dietary Na+) elevated plasma aldosterone concentrations (PAC), or aldosteronism, have been incriminated in both the appearance of CMS and its progressive nature. The deleterious dual consequences of elevated PAC and dietary Na+ have been linked to several components of the CMS.1, 2, 3, 4, 5 Moreover, their adverse progressive consequences are considered synergistic, culminating in oxidative stress where the rate of reactive oxygen species (ROS) generation exceeds their rate of detoxification by antioxidant defenses. There follows oxidative injury involving the heart and systemic tissues.
Our experimental studies in rats receiving aldosterone/salt treatment (ALDOST) have identified a common pathogenic event that links aldosteronism to the induction of oxidative stress in the heart, and in such diverse tissues as peripheral blood mononuclear cells (PBMC). Herein, we review these major findings and our view of the important role of excessive intracellular Ca2+ accumulation (EICA), also referred to as intracellular Ca2+ overloading. The origin of EICA is based on elevations in plasma parathyroid hormone (PTH), which is integral to the genesis of secondary hyperparathyroidism (SHPT) that occurs in response to plasma-ionized hypocalcemia and hypomagnesemia, whose appearance is the consequence of marked urinary and fecal excretory losses of Ca2+ and Mg2+ that accompany chronic aldosteronism.
Aldosteronism defined and stimuli that regulate adrenal ALDO production
Definitions
Elevations in PAC are adaptive and homeostatically appropriate when dietary Na+ intake is markedly restricted or intravascular volume is reduced. In the absence of these co-morbidities, elevations in PAC are maladaptive and inappropriate. This is the scenario when elevated PAC are associated with normal or enhanced dietary Na+, such as occurs with congestive heart failure (CHF), where secondary aldosteronism arises from reduced renal perfusion and elaboration of renin by the underperfused kidneys. It also epitomizes the scenario in primary aldosteronism.
Stimuli to ALDO production
Various stimuli provoke zona glomerulosa cells of the adrenal gland to produce ALDO (see Figure 1). Some are considered major factors, whereas other agents are short-lived and, therefore, considered minor stimuli. However, this disparity disappears when minor stimuli are persistently elevated. Renin-dependent elevations in circulating angiotensin II and elevation in extracellular or plasma K+ are major stimuli. Minor stimuli, which become important when their plasma concentrations are chronically elevated during stressor states include: (a) adrenocorticotropin hormone (ACTH) released by an activated hypothalamic-pituitary-adrenal axis; (b) catecholamines also seen in response to hypothalamic-pituitary-adrenal axis activation; and (c) PTH, which accompanies the SHPT seen in response to ionized hypocalcemia with chronic aldosteronism.6, 7 A lipid-soluble ALDO-releasing factor elaborated by adipocytes has recently been implicated.8
Major and minor stimuli to aldosterone production by zona glomerulosa cells of the adrenal glands. Major stimuli include renin-dependent angiotensin II formation and increased extracellular or plasma K+ concentrations. Minor stimuli include adrenocorticotropin hormone (ACTH) and catecholamines derived through an activation of the hypothalamic-pituitary-adrenal (HPA) axis in response to a stressor state. Catecholamine-mediated intracellular Ca2+ overloading and augmented Ca2+ excretion each contribute to the appearance of ionized hypocalcemia. In turn, hypocalcemia promotes secondary hyperparathyroidism with elevated circulating levels of parathyroid hormone (PTH). This calcitropic hormone also leads to intracellular Ca2+ overloading of diverse tissues, including cardiomyocytes and their mitochondria, with an induction of oxidative stress.
Circumstances may exist, such as high dietary Na+ intake (see Figure 2), whereby plasma renin activity and angiotensin II levels are each suppressed, whereas PAC are inappropriately increased owing to zona glomerulosa cell provocation by ACTH, catecholamines and/or PTH. Yet another mechanism for a sustained ALDO-like state has implicated ROS in targeting and activating mineralocorticoid receptors.9, 10, 11 In keeping with the pathophysiological roles, aldosteronism and oxidative stress are salutary responses to mineralocorticoid receptor antagonism.12, 13, 14, 15, 16
A high-salt diet (for example, 8% NaCl) is accompanied by the suppression of plasma renin activity (PRA) and circulating levels of angiotensin (Ang) II and plasma aldosterone concentration (PAC). However, the accompanying hypercalciuria leads to plasma-ionized hypocalcemia, which, in turn, promotes secondary hyperparathyroidism with elevated plasma parathyroid hormone (PTH), and ultimately bone resorption. An activation of the hypothalamic-pituitary-adrenal (HPA) axis likewise accompanies hypocalcemia with ensuing elevations in plasma levels of adrenocorticotropin hormone (ACTH) and catecholamines. PTH, ACTH and catecholamines represent three different stimuli to the adrenal glands’ production of aldosterone. As a result, increased PAC can be found.
An experimental model of aldosteronism
Aldosterone/salt treatment
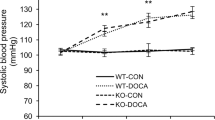
We have worked extensively with the ALDOST model, wherein eight-week-old male Sprague–Dawley rats are first uninephrectomized to reduce renal mass available for Na+ excretion. An osmotic minipump filled with ALDO is implanted subcutaneously; it releases ALDO (0.75 μg h−1) to raise PAC to levels found in patients with congestive heart failure, whereas drinking water is fortified with 1% NaCl to create inappropriate aldosteronism and 0.4% KCl to prevent hypokalemia and associated cardiac pathology.17 Plasma renin activity and circulating angiotensin II levels are each suppressed during ALDOST. Other factors that theoretically could contribute to ALDO production and raise PAC (for example, ACTH, catecholamines and PTH as seen in Figure 1) are irrelevant as the minipump provides an autonomous and continuous source of ALDO release with persistent elevations in PAC. Thus, ALDOST rats, which can be followed for up to 6 weeks, provide an excellent experimental model of chronic inappropriate elevations in PAC independent of the systemically derived stimuli. Furthermore, it represents a unique state of inappropriate aldosteronism as elevations in PAC are present together with the modest increase in dietary Na+ derived from drinking water supplemented with 1% NaCl (vis-à-vis a high salt diet with 8% NaCl). Appropriate aldosteronism would include the minipump combined with dietary Na+ deprivation and which is not associated with cardiac pathology.12, 18 The same is true for 1% NaCl diet alone or for uninephrectomy alone.18
The increment in Na+ excretion that accompanies ALDOST is coupled with a marked augmentation in urinary and fecal excretion of Ca2+ and Mg2+. At the distal segment of the nephron and colon, urinary and fecal Na+ are reabsorbed by ALDO-driven epithelial Na+ channels. Co-treatment with spironolactone (Spiro), an ALDO receptor antagonist, attenuates the excretion of Ca2+ and Mg2+ at these sites.
During weeks 1 and 2, rats appear healthy and are gaining weight comparable to untreated controls (a pre-clinical stage). At week 3, they become lethargic and anorectic with a progressive failure to gain weight (a clinical stage), whereas at week 4 (the pathological stage), lesions appear for the first time in the previously normal heart, as well as the systemic vasculature that includes the kidneys and mesentery.13
Cardiac remodeling in aldosteronism
Cardiac pathology in rats receiving ALDOST includes multiple foci of microscopic scarring and a perivascular fibrosis of the intramural coronary circulation with extensions into the contiguous interstitial space. The scars and perivascular/interstitial fibrosis are scattered throughout the right and left heart.13, 19
In morphological terms, the accumulation of collagen in the myocardium can present as: (a) reactive fibrosis, or perivascular fibrosis in response to proinflammatory coronary phenotype; and (b) as a replacement fibrosis (that is, scar tissue), which replaces cardiomyocytes lost to necrotic cell death to preserve the structural integrity of myocardium (reviewed in Laurent20). Apoptotic cell death, devoid of inflammatory cell or fibroblast responses, is not accompanied by fibrosis. In biophysical terms, fibrosis is expressed as an increase in myocardial hydroxyproline concentration, an amino acid specific to collagen. Depending on its site and magnitude, collagen fiber crosslinking and relative abundance of type I and III collagens will determine the stiffness and where type 1 collagen fibers resemble the tensile strength of steel.21 Fibrosis can adversely increase myocardial stiffness leading to diastolic heart failure, or as more recently coined heart failure with preserved ejection fraction (reviewed in Zile and Brutsaert22, 23 and Díez24). Diastolic heart failure is commonly seen with the concentric hypertrophy that accompanies arterial hypertension. Hypertensive heart disease represents a major etiologic factor that accounts for heart failure. The failing heart in hypertensive heart disease may present as predominant diastolic heart failure or systolic heart failure. The clinical syndrome congestive heart failure, with its characteristic signs and symptoms, can accompany either diastolic heart failure or systolic heart failure. Its origins are rooted in a salt-avid state mediated by effector hormones of the renin–angiotensin–aldosterone system. Left ventricular hypertrophy is a distinguishing feature of hypertensive heart disease; so too is fibrosis, which is found throughout the right and left heart.25, 26, 27 It is not the quantity, rather the quality (structural remodeling) of myocardium that contributes to hypertensive heart disease.
Cardiac remodeling: role of hemodynamic factors
A series of studies have concluded that hemodynamic factors are not directly involved (reviewed in Weber28). This viewpoint was primarily based on: (a) the presence of fibrosis in non-pressure-overloaded right atrium and ventricle; (b) the absence of fibrosis when the LV pressure overload is created by infrarenal aortic banding without subsequent renin–angiotensin–aldosterone system activation or when treatment is based on ALDO together with a low-Na+ diet, or when 1% NaCl alone is given; and (c) the prevention of fibrosis with either a small (non-depressor) or large (depressor) dose of Spiro, which respectively fails to or does prevent hypertension. An intracerebroventricular infusion of a mineralocorticoid receptor antagonist prevents hypertension, but not fibrosis.29 The upregulation of ALDO synthase in the heart accounts for increased tissue levels of ALDO, but are not accompanied by fibrosis.30 Thus, the evidence gathered to date indicates the adverse myocardial remodeling during ALDOST is both independent of hypertension and unrelated to plasma- or tissue-derived ALDO per se. Therefore, some other circulating factor that accompanies aldosteronism must be operative (vide infra).
Sodium: the facilitator in aldosteronism
Hypercalciuria and hypermagnesuria
Our studies showed the early and persisting elevation in urinary and fecal excretion of Ca2+ and Mg2+ in rats during ALDOST. The marked loss of Ca2+ and Mg2+ was evident during pre-clinical and clinical stages of ALDOST and involved renal and gastrointestinal sites of excretion, both of which have high-density ALDO receptor binding.31 Hypercalciuria accompanies the short-term treatment of man or animals with a mineralocorticoid plus dietary salt.32, 33, 34, 35, 36, 37 It is present in patients with primary aldosteronism, where it is accentuated by dietary Na+ loading.36, 38 The increment in urinary Ca2+ excretion, which occurs in the distal segment of the nephron, is dietary Na+ dependent. Urinary Mg2+ excretion also rises with dietary Na+ loading in rats treated with a mineralocorticoid, whereas the hypermagnesuria found in patients with primary aldosteronism is abrogated by either Spiro or surgical removal of diseased adrenal tissue.39, 40, 41 In rats receiving 4 weeks ALDOST, we found Spiro co-treatment to, respectively, attenuate or abrogate the enhanced urinary and fecal excretion of each cation beginning at week 1 onward.
The stimulus responsible for the hypercalciuria and hypermagnesuria that accompanies ALDOST is not fully clear. However, elevations in arterial pressure or the mineralocorticoid hormone itself (in the absence of dietary Na+) have each been discounted.32, 33 A role for such metabolic derangements as polydipsia and metabolic alkalosis that accompany chronic mineralocorticoid/salt treatment have likewise been eliminated.37 In both rats and man, marked Na+ loading alone (for example, a 8% NaCl diet) is accompanied by hypercalciuria, SHPT with bone loss and a proinflammatory vascular phenotype.42, 43, 44, 45, 46, 47, 48, 49, 50 The likely mechanism is thought to be related to an expansion of the extravascular space, resulting in decreased proximal tubular resorption and thereby increased distal delivery of Na+, Ca2+ and Mg2+, with the mineralocorticoid promoting distal tubular Na+ resorption without retarding Ca2+ or Mg2+ excretion.32, 33, 34, 35, 36 This may be further accentuated by nitric oxide-mediated increments in medullary blood flow.51, 52
Secondary hyperparathyroidism
The sustained urinary and fecal loss of Ca2+ and Mg2+, which accompanies ALDOST, leads to a progressive fall in plasma-ionized concentrations of these divalent cations and ultimately to a reduction in bone mineral density. Plasma-ionized [Ca2+]o and [Mg2+]o were markedly reduced at week 4, whereas each of these cations had already begun to fall during the pre-clinical stage at weeks 1 and 2 ALDOST. Ionized hypocalcemia and hypomagnesemia each regulate PTH secretion.53, 54 Bone and its mineral stores are the primary reserve for these cations, with bone resorption facilitated by PTH. Elevations in PTH, elaborated in response to reduced plasma-ionized [Ca2+]o and [Mg2+]o, would be expected in the setting of sustained hypercalciuria and hypermagnesuria. We indeed found elevated plasma PTH levels, consistent with SHPT, during weeks 1–4 ALDOST. Both serum-ionized [Ca2+]o and total plasma Ca2+ are reduced in response to deoxycorticosterone/salt treatment,37 together with increased serum PTH and urinary excretion of cAMP, a biomarker of parathyroid activity. SHPT has been reported in patients with primary aldosteronism,41, 55, 56, 57 where expected aberrations in serum-ionized and total Ca2+, together with elevations in PTH, were normalized by either adrenal surgery or Spiro.41, 57
Our second major finding, and further evidence in keeping with persistent SHPT, is the marked and progressive reduction in bone mineral density and bone mineral content of tibia and femur that appeared by week 4 ALDOST and was more evident at weeks 5 and 6. This hitherto unappreciated fall in bone mineral density and bone mineral content was rapid and accompanied by a corresponding reduction in bone strength. Urinary hydroxyproline, a marker of bone resorption, is increased during ALDOST or deoxycorticosterone/salt treatment,58 whereas the hypercalciuria seen with 8% NaCl loading alone is likewise accompanied by SHPT, with a loss of bone Ca2+ and Mg2+ and increased urinary excretion of various markers of bone resorption.42, 44, 46
Cellular and molecular pathways leading to cardiomyocyte necrosis
Pathways accounting for cardiomyocyte necrosis and subsequent scarring of myocardium found at 4 weeks ALDOST have been examined and the pathogenic role of circulating factors elucidated.
Oxidative stress
Evidence of oxidative stress in the myocardium is found during chronic mineralocorticoidism.13, 59, 60, 61, 62 This includes: the presence of 3-nitrotyrosine, a byproduct of the reaction involving superoxide and nitric oxide; an activation of the gp91phox subunit of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase found in inflammatory cells invading the injured myocardium that contributes to superoxide generation; upregulated redox-sensitive nuclear transcription factor-κB and a proinflammatory gene cascade it regulates that includes intercellular adhesion molecule (ICAM)-1, monocyte chemoattractant protein (MCP)-1 and tumor necrosis factor-α; and increased tissue levels of 8-isoprostane and malondialdehyde, biomarkers of lipid peroxidation.13, 62 There is also considerable evidence of oxidative stress in blood and urine consistent with the systemic nature of an altered redox state during chronic aldosteronism.
Intracellular Ca2+ overloading and SHPT
Our hypothesis for the induction of oxidative stress during ALDOST draws upon Albrecht Fleckenstein's original concept that intracellular Ca2+ overloading of the heart is an integral and adverse pathophysiological feature leading to myocardial necrosis.63 In rats receiving 1 and 4 weeks ALDOST, we monitored intracellular Ca2+ levels in several tissues that included the heart and PBMC. We found increased Ca2+ levels in the myocardium and PBMC during pre-clinical, clinical and pathological stages, accompanied by biomarker evidence of oxidative stress that included increased levels of malondialdehyde and 8-isoprostane in the heart and increased H2O2 production by PBMC.14, 62, 64, 65
Metabolic studies accounted for the marked increase in urinary and fecal excretion of Ca2+ and Mg2+ during ALDOST, which leads to plasma-ionized hypocalcemia and hypomagnesemia. The calcium-sensing receptor of the parathyroid glands, in turn, responds to hypocalcemia with increased secretion of PTH. Accordingly, plasma PTH levels were elevated at weeks 1–4 ALDOST,14 with SHPT as evidenced by bone resorption.66 We therefore hypothesized that the intracellular Ca2+ overloading and induction of oxidative stress that accompanies ALDOST leading to cardiomyocyte necrosis and fibrosis is mediated by the calcitropic hormone, PTH and not ALDO (see Figure 3). This represents an example of the SHPT-associated Ca2+ paradox as characterized by Fujita and Palmieri.67 The elegant studies of Massry et al.68 have shown PTH-mediated intracellular Ca2+ overloading of cardiomyocytes that included: cardiac myocytes incubated with PTH; and cells harvested from normal rats receiving a 2-week infusion of PTH or rats with chronic renal failure having SHPT.69 In each case, co-treatment with verapamil, a Ca2+ channel blocker, prevented the rise in intracellular Ca2+. PTH also regulates cardiomyocyte Ca2+ channel opening.70 Using radiolabeled PTH, Nordquist and Palmieri71 found that PTH not only penetrates plasmalemma but also localizes within the cytoplasm of renal tubular cells and predominantly in the mitochondria, in which its mechanism of transport and function remain to be fully elucidated. Rasmussen and other investigators found PTH to alter mitochondrial [Ca2+]m and respiration.72, 73, 74, 75, 76 EICA in cardiomyocytes and consequent generation of ROS alter intracellular signaling events, including their perpetuation of intracellular Ca2+ overloading via L-type Ca2+ channel entry and inhibition of Ca2+ efflux by Ca2+-ATPase.77, 78 A Na+/Ca2+ exchanger involved in regulating Na+-dependent Ca2+ efflux from mitochondria may also be contributory.79, 80
Aldosterone/salt treatment (ALDOST) in rats and associated increments in urinary and fecal Ca2+ excretion leads to plasma-ionized hypocalcemia with secondary hyperparathyroidism and elevated plasma parathyroid hormone (PTH) levels. In turn, and what is considered a Ca2+ paradox, PTH promotes intracellular Ca2+ overloading. In the case of cardiomyocytes, this includes increased cytosolic free [Ca2+]i and mitochondrial [Ca2+]m. Ca2+-overloaded mitochondria elaborate reactive oxygen species and, together with the ensuing oxidative stress, account for the pathological opening of the mitochondria permeability transition pore (mPTP) and entry of solutes that lead to osmotic swelling and destruction of these organelles. Cardiomyocyte necrosis follows with the escape, or leak, or troponins and a wound-healing response with a replacement fibrosis, or myocardial scarring. Adapted from Whitted AD, et al. Am J Med Sci 2010; 340: 48–53, with permission.
PTH-mediated intracellular Ca2+ overloading is coupled to an induction of oxidative stress in diverse tissues that includes cardiomyocytes and their mitochondria, as well as PBMC. The generation of ROS and reactive nitrogen species appear to overwhelm their rate of detoxification by the cumulative capacity of antioxidant defenses. In mitochondria, Ca2+ overloading and oxidative stress lead to a non-physiological opening of the mitochondria permeability transition pore, with the ensuing osmotic-based structural and functional degeneration of these organelles that triggers the downhill final common cell death pathway leading to cardiomyocyte necrosis and subsequent replacement fibrosis.81
Interventions preventing cardiomyocyte necrosis
A series of site-directed, sequential pharmacological interventions targeted along the cellular–molecular cascades to block downstream events leading to cardiomyocyte necrosis and myocardial scarring were conducted (see Figure 4). These observations collectively validated our hypothesis with regard to the pathological sequelae of events leading to this structural remodeling of myocardium in rats with chronic aldosteronism. Various co-treatments were used, which included: Spiro, an ALDO receptor antagonist, which attenuated the enhanced urinary and fecal losses of these cations to prevent hypocalcemia and hypomagnesemia and thereby ensuing SHPT;14 a Ca2+- and Mg2+-supplemented diet, together with vitamin D3 to enhance Ca2+ absorption, which prevented hypocalcemia and SHPT;82 parathyroidectomy, performed before starting ALDOST, prevented SHPT83 and has been found to prevent vascular lesions and the rise in aortic tissue Ca2+ content during deoxycorticosterone/salt treatment;84 cinacalcet, a calcimimetic that resets the threshold of the parathyroid glands’ Ca2+-sensing receptor prevents SHPT, despite hypocalcemia;85 amlodipine, a Ca2+ channel blocker, which prevents intracellular Ca2+ overloading;64 and N-acetylcysteine, an antioxidant that abrogated oxidative stress.13
Various interventions were carried out to target specific components of the paradigm linking aldosterone/salt treatment (ALDOST) to intracellular Ca2+ overloading and the induction of oxidative stress leading to cardiomyocyte necrosis. These included: spironolactone (Spiro), an aldosterone receptor antagonist; a Ca2+- and Mg2+-supplemented diet, together with vitamin D3 to enhance the absorption of these cations; parathyroidectomy (PTx); cinacalcet, a calcimimetic to reset the threshold of the parathyroid glands’ Ca2+-sensing receptor; amlodipine, a Ca2+ channel blocker; and NAC, N-acetylcysteine, an antioxidant. Adapted from Kamalov G, et al. Am J Med Sci 2009; 338: 28–33, with permission.
Taken together, the multitude of evidence gathered to date congruently supports that PTH-mediated intracellular Ca2+ overloading is the most likely mechanism that leads to the induction of oxidative stress during aldosteronism, in which ROS and reactive nitrogen species, primarily derived from the mitochondria in cardiomyocytes and NADPH oxidase in vascular tissue, overwhelm cellular antioxidant defenses. This scenario begs the question whether the overall consequence of an excessive generation of pro-oxidants or cumulative endogenous antioxidant defenses in combating ROS and reactive nitrogen species had been compromised. In this context, we next addressed plausible association of Zn2+ dyshomeostasis during ALDOST, given its relevance to these endogenous defenses, including Cu/Zn-superoxide dismutase (SOD).
Zinc dyshomeostasis in aldosteronism
Chronic inappropriate excess of ALDO is accompanied by increased urinary and fecal excretory Zn2+ losses, hypozincemia and a fall in plasma Cu/Zn-SOD activity.86 The hyperzincuria seen with ALDOST is related to urinary acidification, which contributes to the consequent metabolic alkalosis of aldosteronism.62 Also contributory to hypozincemia is a coordinated selective translocation of Zn2+ to the sites of tissue injury, facilitated by corresponding upregulation of a Zn2+-binding protein, metallothionein (MT)-1 in targeted tissues.62, 86
We also used 65Zn to systematically monitor Zn2+ kinetics during 1 and 4 weeks of ALDOST. A simultaneous fall in plasma 65Zn, and a selective accumulation of 65Zn, was found at sites of injury that included its translocation to freshly incised skin at week 1 caused by osmotic minipump implantation, as well as the injured heart and kidneys at week 4. This intracellular trafficking of 65Zn to injured tissues was facilitated by the upregulation of MT-1.87 However, at week 4 there was a contemporaneous decline in 65Zn in healed skin and bone, which serve as Zn2+ reservoirs in an attempt to resolve hypozincemia. Thus, the preferential translocation of circulating Zn2+ to injured tissues contributes to hypozincemia found with ALDOST, in which increased tissue Zn2+ is essential in wound healing at these sites.88 As dyshomeostasis of Zn2+ proved to be another integral feature of aldosteronism, it became crucial to investigate whether the increased tissue Zn2+ in the injured myocardium involved both its cardiac myocytes and mitochondria.
Zinc and antioxidant defenses
Cardiac myocytes and mitochondria were harvested from rats with 4 weeks of ALDOST associated with the pathological stage, as well as from experimental controls. We found increased cytosolic free [Zn2+]i in cardiac myocytes and total [Zn2+]m concentration in the mitochondria.62 The rise in cardiomyocyte [Zn2+]i was facilitated by the increased expression of membranous Zn2+ transporters. Increased [Zn2+]i serves to augment the antioxidant defenses of cardiomyocytes, including their upregulation of MT-1 and activation of metal-responsive transcription factor-1, which encodes genes related to various antioxidant defenses, such as Cu/Zn-SOD, MT-1 and glutathione synthase. Thus, intracellular Zn2+ loading in chronic aldosteronism is contemporaneous with intracellular Ca2+ overloading and relevant biomarkers of oxidative stress.89 Pathophysiologically and in terms of innate redox states, Zn2+ appears to serve as antioxidant and Ca2+ as pro-oxidant in our experimental model (see Figure 5). This concept offers the prospect of exploiting Zn2+ supplementation as a novel therapeutic strategy to uncouple the intrinsically coupled Ca2+ and Zn2+ dyshomeostasis in favor of increasing [Zn2+]i, thus enhancing the overall endogenous antioxidant defense capacity that simultaneously attenuate adverse myocardial remodeling.
The intrinsically coupled dyshomeostasis of Ca2+ and Zn2+ found in aldosterone/salt treatment (ALDOST). Increased excretory losses of these divalent cations lead to hypocalcemia and hypozincemia. Secondary hyperparathyroidism with persistent elevations in circulating parathyroid hormone (PTH) follows and are accompanied by uncontrolled Ca2+ entry via L-type Ca2+ channels (LTCC) to saturate intracellular binding and storage sites, and ultimately to [Ca2+]i overloading and excessive [Ca2+]m within the mitochondria. An induction of oxidative stress and generation of reactive oxygen species (ROS) ensues arising from the mitochondria. The rise in [Zn2+]i and [Zn2+]m involves increased Zn2+ entry via LTCC to a minor extent, whereas the majority of [Zn2+]i is regulated by membrane-bound Zn transporters, including Zip1 and ZnT-1, and its binding to metallothionein (Zn/MT). ROS serve as signals that initiate an activation of molecular transducers. These include: stress-response kinases, MAPKs, and their activation of redox-sensitive nuclear transcription factor (NF)-κB and a proinflammatory gene cascade it induces, including adhesion molecules (ICAM-1), chemokines (MCP-1) and cytokines tumor necrosis factor-α (TNF-α) and tumor growth factor-β (TGF-β); and the activation of inducible or endothelial nitric oxide synthases (iNOS and eNOS), where nitric oxide (NO) generation releases Zn2+ from the Zn/MT complex. Increased [Zn2+]i serves to activate its sensor, metal-response element transcription factor (MTF)-1, and the antioxidant genes it induces. These include MT-1, Cu/Zn-SOD and glutathione (GSH) synthase. Increased [Ca2+]i and [Ca2+]m are pro-oxidants, which in toxic amounts threaten the fate of cardiomyocytes, whereas increments in [Zn2+]i and [Zn2+]m are antioxidants. Reprinted from Kamalov G, et al. J Cardiovasc Pharmacol 2009; 53: 414–423, with permission.
The efficacy of a Zn2+ supplement in augmenting intracellular [Zn2+]i, and thereby antioxidant defenses, in rats receiving ALDOST was explored using ZnSO4.62 Co-treatment of ALDOST rats with ZnSO4 prevented hypozincemia and a fall in plasma Cu/Zn-SOD activity, whereas significantly increasing cardiomyocyte cytosolic [Zn2+]i. It also attenuated biomarkers of oxidative stress, such as cardiac 8-isoprostane, and microscopic scarring. Thus, validating our concept that increased tissue Zn2+ in the heart serves as an antioxidant, and intracellular Ca2+ overloading as pro-oxidant, in the genesis of cardiomyocyte necrosis that highlights the intrinsic co-dependency of these two biologically essential and dynamic divalent cations (vide infra). Others have also reported a Zn2+ supplement to be cardioprotective in mice with streptozocin-induced diabetic cardiomyopathy, in rat hearts with ischemia/reperfusion injury or following isoproterenol administration.62, 90, 91, 92
Coupled Ca2+ and Zn2+ dyshomeostasis
The dyshomeostasis of extra- and intracellular Ca2+ and Zn2+ that accompanies ALDOST contributes to a deleterious, but reversible disequilibrium between pro- and antioxidants. We hypothesized that intrinsic coupling of intracellular Ca2+ and Zn2+ dyshomeostasis inherently regulate the redox state of cardiac myocytes and mitochondria. To test our hypothesis, we monitored each of these two cations using relevant fluorescent tags and fluorescence microscopy in cardiac myocytes and mitochondria harvested from rats receiving 4 weeks ALDOST alone or in combination with Spiro or amlodipine co-treatment. Compared with untreated, age-/sex-matched controls, we found increased cardiomyocyte cytosolic free [Ca2+]i and [Zn2+]i, together with elevated mitochondrial [Ca2+]m and [Zn2+]m, each of which could be prevented by Spiro and significantly attenuated by amlodipine co-treatment.89 These salutary iterations in divalent cation composition corroborated well with the levels of 3-nitrotyrosine and 4-hydroxy-2-nonenal in cardiomyocytes, together with altered H2O2 production, malondialdehyde and oxidized glutathione in the mitochondria that were co-incident with increased activities of Cu/Zn-SOD and glutathione peroxidase.62, 81, 89 Furthermore, adaptive alterations in intracellular [Zn2+]i were accompanied by the contemporaneous upregulation of MT-1, a Zn2+ importer and exporter (Zip1 and ZnT-1, respectively) and metal-responsive transcription factor-1.
Thus, in cardiac myocytes and mitochondria from the remodeled myocardium, an intrinsically coupled dyshomeostasis of intracellular Ca2+ and Zn2+ serves to regulate the redox state via induction of oxidative stress and generation of antioxidant defenses, respectively. These findings underscore the clinical relevance of combining pharma- and nutriceutical strategies that can uncouple the coupled dyshomeostasis of these biologically essential cations, and preferentially modulate them in favor of sustained antioxidant defenses. The coupled Ca2+ and Zn2+ dyshomeostasis seen in aldosteronism resembles the Ca2+ overloading and oxidative stress mirrored in the hearts of hamsters with hereditary muscular dystrophy, which is also accompanied by increased tissue Zn2+.93, 94, 95, 96, 97 This divalent cation dyshomeostasis seen in muscular dystrophy could be prevented by parathyroidectomy or a Ca2+ channel blocker.95, 96 Furthermore, our findings with ALDOST resemble the protective role of increased [Zn2+]i induced by a Zn2+ supplement or Zn2+ ionophore, when intracellular [Ca2+]i overloading of the heart is present.98
The temporal response to coupled Ca2+ and Zn2+ dyshomeostasis
Intracellular [Ca2+]i overloading, coupled with the induction of oxidative stress, is present at 4 weeks ALDOST. This pro-oxidant reaction in cardiac myocytes and mitochondria accounts for necrotic cell death and subsequent myocardial scarring. The rise in [Ca2+]i, a pro-oxidant, is intrinsically linked to increased [Zn2+]i serving as antioxidant. We addressed the temporal responses in coupled Ca2+ and Zn2+ dyshomeostasis, reflecting the pro-oxidant:antioxidant equilibrium, by examining pre-clinical and pathological stages of ALDOST, and by observing whether endogenous antioxidant defenses were ultimately overwhelmed accounting for the delay in cardiac remodeling. Responses in [Ca2+]i and [Zn2+]i and mitochondrial total [Ca2+]m and [Zn2+]m, together with biomarkers of oxidative stress and antioxidant defenses, during 1 and 4 weeks ALDOST were monitored and compared. At week 1 and compared with controls, we found: (i) elevations in [Ca2+]i and [Ca2+]m to be coupled with [Zn2+]i and [Zn2+]m; (ii) increased mitochondrial H2O2 production, cardiomyocyte xanthine oxidase activity, and cardiac and mitochondrial 8-isoprostane levels, counterbalanced by increased activity of antioxidant proteins, enzymes and the non-enzymatic antioxidants that can be considered together as cumulative antioxidant capacity. Some of these enzymes and proteins (for example, MT-1, Cu/Zn-superoxide, glutathione synthase) are regulated by metal-responsive transcription factor-1; and (iii) although these augmented antioxidant defenses were sustained at week 4, overall they fell short in combating the persistent intracellular Ca2+ overloading and the consequential marked rise in cardiac tissue 8-isoprostane and mitochondria permeability transition pore opening.
Thus, the intrinsically coupled Ca2+ and Zn2+ dyshomeostasis occurs early during ALDOST in cardiac myocytes and mitochondria that regulate redox equilibrium until week 4, when ongoing intracellular Ca2+ overloading and accelerated rate of pro-oxidant generation overwhelm their rate of detoxification by antioxidant defenses. These observations support our contention that intracellular [Ca2+]i overloading accounts for the induction of oxidative stress that leads to necrotic cell death and consequent replacement fibrosis or myocardial scarring.
Uncoupling the coupled dyshomeostasis of Ca2+ and Zn2+
The pro-oxidant response to Ca2+ overloading in cardiac myocytes and mitochondria has been shown to be intrinsically coupled to simultaneous increased Zn2+ entry serving as an antioxidant.89 Later, we investigated whether Ca2+ and Zn2+ dyshomeostasis and pro-oxidant:antioxidant disequilibrium seen at 4 weeks, the pathological stage of ALDOST, could be uncoupled in favor of antioxidants, using co-treatment with a ZnSO4 supplement (see Figure 5), pyrrolidine dithiocarbamate (PDTC), a Zn2+ ionophore, or ZnSO4 in combination with a Ca2+ channel blocker, amlodipine. Responses in cardiomyocyte free [Ca2+]i and [Zn2+]i, together with biomarkers of oxidative stress in cardiac myocytes and mitochondria, were monitored and contrasted. At week 4 ALDOST and compared with controls, we found: (i) an elevation in [Ca2+]i was coupled with [Zn2+]i; and (ii) increased mitochondrial H2O2 production, and increased mitochondrial and cardiac 8-isoprostane levels. Co-treatment with the ZnSO4 supplement alone, PDTC alone or ZnSO4+amlodipine augmented the rise in cardiomyocyte [Zn2+]i beyond that seen with ALDOST alone, while attenuating the rise in [Ca2+]i, which together served to reduce oxidative stress. Furthermore, ZnSO4, PDTC and ZnSO4+amlodipine were cardioprotective and attenuated necrosis and myocardial scarring.13, 62, 98
Thus, the intrinsically coupled dyshomeostasis of intracellular Ca2+ and Zn2+ found in cardiac myocytes and mitochondria during 4 weeks ALDOST could be uncoupled in favor of antioxidant defenses by selectively increasing free [Zn2+]i and/or reducing [Ca2+]i using co-treatment with ZnSO4, PDTC alone or ZnSO4+amlodipine in combination. Each of these interventions proved to be cardioprotective. These cumulative salutary observations raise the therapeutic prospect that nutriceuticals capable of favorably influencing extra- and intracellular Ca2+ and Zn2+ balance, which is pivotal to oxidative injury, could prevent cardiac myocyte necrosis and myocardial scarring. This contrasts to the central nervous system, where Zn2+ is considered to be cytotoxic.99
Cellular and molecular pathways leading to proinflammatory coronary vascular phenotype
The proinflammatory coronary vascular phenotype
An adaptive upregulation of adhesion molecules and chemoattractant chemokines appears early within the endothelium of the affected vasculature during ALDOST. They include: ICAM-1, vascular cell adhesion molecule-1, platelet-endothelial cell adhesion molecule-1; and MCP-1 and osteopontin.13, 60, 100, 101, 102, 103, 104, 105, 106, 107 MCP-1 has been shown to be integral to the homing of inflammatory cells into cardiovascular tissue. Within invading inflammatory cells, there is evidence of an activation of a redox-sensitive nuclear transcription factor-κB and increased expression of a proinflammatory mediator cascade that it regulates, including ICAM-1, MCP-1 and tumor necrosis factor-α. Also, there is an activation of NADPH oxidase, a source of superoxide formation; increased NADPH oxidase activity; and 3-nitrotyrosine labeling, a stable tyrosine residue indicative of the formation of peroxynitrite, a reactive nitrogen species and product of the reaction between nitric oxide and superoxide.13, 60, 61, 107, 108, 109 Thus, the cumulative evidence points to an induction of oxi/nitrosative stress in promoting this phenotype.
The induction of oxi/nitrosative stress
In rats with ALDOST or another mineralocorticoid, deoxycorticosterone/salt treatment, the accompanying elevations in arterial pressure have been held responsible for the induction of oxi/nitrosative stress in cardiovascular tissue.59, 110, 111, 112 Such evidence, however, is also found in post-capillary venules,113 in which elevations in intraluminal pressure are not expected. In addition, an altered redox state is not seen with comparable elevations in arterial pressure induced by norepinephrine.110 An alternative mechanism of action therefore needs to be explored.
In returning to the proinflammatory phenotype, ALDOST reduces cytosolic free concentrations of [Mg2+]i in various cultured cells, including lymphocytes.114, 115 An efflux of Mg2+ from the cell by a Na+/Mg2+ exchanger, a compartmentalization of this cation within organelles, or its enhanced binding to ATP may be responsible. [Mg2+]i is the biologically active component of this important divalent cation. A reduction in [Mg2+]i can lead to intracellular Ca2+ loading and subsequent induction of oxi/nitrosative stress. Mechanisms responsible for augmented intracellular Ca2+ inevitably relate to PTH-mediated Ca2+ entry and the presence of SHPT. A hyperadrenergic state also accompanies chronic mineralocorticoidism and therefore catecholamine-mediated EICA must also be considered. Evidence in support of Ca2+ overload leading to an altered redox state with the activation of immune cells includes: (i) reduced [Mg2+]i in circulating monocytes and lymphocytes of rats treated with ALDOST or in man having primary aldosteronism;65, 115, 116 (ii) elevated [Ca2+]i and total Ca2+ concentration of PBMC in response to ALDOST and which occurs before tissue invasion, together with increased H2O2 production by monocytes and lymphocytes;65 (iii) PTH regulated T-cell activation;117, 118, 119, 120 (iv) parathyroidectomy prevented PBMC Ca2+ overloading and vascular lesions;83, 84 (v) upregulated expression of antioxidant defenses in these cells; and (vi) prevention of Ca2+ loading and oxi/nitrosative stress by co-treatment with either Spiro or an antioxidant.13, 65, 116 The presence of oxi/nitrosative stress at a systemic level in these models is evidenced by increased serum levels of thiobarbituric acid-reacting substances and reduced activity of plasma α1-antiproteinase.60, 61, 116 This early immunostimulatory state that features PBMC activation is further evidenced by: B-cell activation with increased expression of immunoglobulins; an expansion of the B-cell lymphocyte subset; an increase in major histocompatibility complex class II-expressing lymphocytes; and increased expression of ICAM-1, integrin-α1, CC and CXC chemokine proteins and receptors, interleukin-1β and its receptor type 2, and interferon-γ.65, 116 There is also evidence of autoreactivity, which may explain the delayed appearance of vascular remodeling (for example, first seen at week 4 ALDO/salt treatment). The prospect that H2O2 serves as second messenger to mimic antigen-antigen receptor binding121 is also raised by these findings given that the heart remains intact before the appearance of vascular lesions. In future studies, decoding the PBMC molecular phenotype (that is, their transcriptome and proteome) may yield novel non-invasive biomarkers of risk, onset and progression of vascular remodeling.
Intervention(s) preventing the appearance of an immunostimulatory state
In recognizing the pathogenic roles of hormone-induced, redox state-transduced activation of immune cells in leading to the proinflammatory vascular phenotype, the prevention of such adverse structural remodeling related to underlying pathophysiological mechanisms can be developed. The reduction in arterial pressure is becoming less relevant and indeed may prove an indirect outcome to successful immunomodulation. A paradigm depicting the pathophysiological scenario—inflammation to fibrosis—is shown in Figure 6, together with potential pharmacological interventions. Cumulative experimental evidence is emerging to suggest the therapeutic role of these agents as immunomodulators. These include: attacking the neuroendocrine-immune interface via antagonists to AT1,101, 106, 122 ALDO,12, 13, 104, 123, 124 or endothelinA60, 100, 107, 125 receptors; and preventing intracellular Ca2+ loading, which is responsible for the induction of oxi/nitrosative stress, by using a dihydropyridine receptor blocker103, 126 or T-type127 Ca2+ channel blocker. Shoring up endogenous antioxidant defenses with the administration of an antioxidant, such as PDTC, N-acetylcysteine or probucol,13, 105, 108, 109, 128, 129, 130, 131 represent other avenues. Agents that are active in modulating oxidative stress and influencing the transcription of genes, which promote the proinflammatory vascular phenotype, such as 3-hydroxy-3-methyglutaryl coenzyme A reductase102, 132, 133, 134 and ligands to peroxisome proliferator-activated receptor-gamma and -alpha,135, 136, 137, 138, 139 also prove to be cardio- and renoprotective. Selective inhibition of phosphodiesterase isoforms, which iterate cyclic nucleotide second messengers (cAMP and cGMP) to downregulate mitogen- and antigen-induced T-cell proliferation, Th-1- and Th-2-derived proinflammatory cytokines and adhesion molecule expression in these cells have also been reported to be cardioprotective.140 Furthermore, mycophenolate mofetil, which selectively inhibits T-cell proliferation,141 was renoprotective.130
An immunostimulatory state with activated peripheral blood mononuclear cells (PBMC) accompanies aldosterone/salt treatment (ALDOST) in rats, and is based on intracellular Ca2+ overloading and induction of oxi/nitrosative stress derived from nicotinamide adenine dinucleotide phosphate (NADPH) oxidase. Activation of a redox-sensitive nuclear transcription factor (NF)-κB leads to the upregulation of a proinflammatory gene cascade it regulates that includes: intracellular adhesion molecule (ICAM)-1, monocyte chemoattractant protein (MCP)-1 and tumor necrosis factor (TNF)-α. The invasion of intramural vessels by these monocytes and lymphocytes accounts for a vasculopathy and, together with fibroblast-like cells, eventuates in a perivascular fibrosis. Various targeted interventions have been shown to be capable of ablating this sequence of events. These include: spironolactone (Spiro); a Ca2+ channel blocker (CCB); an antioxidant, such as NAC, N-acetylcysteine, an antioxidant; and peroxisome proliferator-activated receptor (PPAR), 3-hydroxy-3-methyglutaryl coenzyme A (HMG-CoA), phosphodiesterase isoform (PDEI) and mycophenolate mofetil (MMF). Adapted from Weber KT. Hypertension 2004; 43: 716–719, with permission.
Summary and conclusions
EICA accompanies inappropriate (relative to dietary Na+) elevations in PAC, or aldosteronism, and leads to a pro-oxidant phenotype involving such diverse tissues as the heart and PBMC. The deleterious dual consequences of elevated PAC and dietary Na+ are linked to the induction of oxidative stress via PTH-mediated intracellular Ca2+ overloading, and which may relate to the pathogenesis of the CMS and its components. The genesis of this SHPT occurs in response to plasma-ionized hypocalcemia and hypomagnesemia, whose appearance is the consequence of marked urinary and fecal excretory losses of Ca2+ and Mg2+ that accompany chronic aldosteronism.
Sustained EICA has its pathological consequences. In the case of cardiac myocytes and mitochondria, intracellular Ca2+ overloading leads to an induction of oxidative stress and opening of the mitochondrial permeability transition pore with ensuing organellar destruction and cellular necrosis, with subsequent replacement fibrosis, or scarring. In PBMC, the EICA and resultant oxidative stress contributes to the activation of lymphocytes and monocytes with this immunostimulatory state eventuating in a vasculopathy of the intramural coronary vasculature and appearance of a perivascular fibrosis. Intracellular Ca2+ overloading serves as pro-oxidant; it is intrinsically coupled to intracellular Zn2+ dyshomeostasis serving as antioxidant. Pharmaceutical and/or nutriceuticals used as targeted interventions of the cellular and molecular pathways leading to EICA or intracellular Zn2+-based antioxidant defenses protect against adverse myocardial remodeling, and thereby are cardioprotective. These cumulative salutary responses raise the prospect that therapeutic interventions, capable of favorably influencing extra- and intracellular Ca2+ and Zn2+ equilibrium, could potentially optimize the management of aldosteronism.
References
Ando K, Fujita T . Metabolic syndrome and oxidative stress. Free Radic Biol Med 2009; 47: 213–218.
Fujita T . Aldosterone in salt-sensitive hypertension and metabolic syndrome. J Mol Med 2008; 86: 729–734.
Whaley-Connell A, Johnson MS, Sowers JR . Aldosterone: role in the cardiometabolic syndrome and resistant hypertension. Prog Cardiovasc Dis 2010; 52: 401–409.
Kidambi S, Kotchen JM, Grim CE, Raff H, Mao J, Singh RJ, Kotchen TA . Association of adrenal steroids with hypertension and the metabolic syndrome in blacks. Hypertension 2007; 49: 704–711.
Kotchen TA, Kotchen JM, Grim CE, Krishnaswami S, Kidambi S . Aldosterone and alterations of hypertension-related vascular function in African Americans. Am J Hypertens 2009; 22: 319–324.
Rosenberg J, Pines M, Hurwitz S . Response of adrenal cells to parathyroid hormone stimulation. J Endocrinol 1987; 112: 431–437.
Rosenberg J, Pines M, Hurwitz S . Stimulation of chick adrenal steroidogenesis by avian parathyroid hormone. J Endocrinol 1988; 116: 91–95.
Ehrhart-Bornstein M, Lamounier-Zepter V, Schraven A, Langenbach J, Willenberg HS, Barthel A, Hauner H, McCann SM, Scherbaum WA, Bornstein SR . Human adipocytes secrete mineralocorticoid-releasing factors. Proc Natl Acad Sci USA 2003; 100: 14211–14216.
Wang H, Shimosawa T, Matsui H, Kaneko T, Ogura S, Uetake Y, Takenaka K, Yatomi Y, Fujita T . Paradoxical mineralocorticoid receptor activation and left ventricular diastolic dysfunction under high oxidative stress conditions. J Hypertens 2008; 26: 1453–1462.
Goodfriend TL, Ball DL, Egan BM, Campbell WB, Nithipatikom K . Epoxy-keto derivative of linoleic acid stimulates aldosterone secretion. Hypertension 2004; 43: 358–363.
Payet MD, Goodfriend TL, Bilodeau L, Mackendale C, Chouinard L, Gallo-Payet N . An oxidized metabolite of linoleic acid increases intracellular calcium in rat adrenal glomerulosa cells. Am J Physiol Endocrinol Metab 2006; 291: E1160–E1167.
Brilla CG, Matsubara LS, Weber KT . Anti-aldosterone treatment and the prevention of myocardial fibrosis in primary and secondary hyperaldosteronism. J Mol Cell Cardiol 1993; 25: 563–575.
Sun Y, Zhang J, Lu L, Chen SS, Quinn MT, Weber KT . Aldosterone-induced inflammation in the rat heart. Role of oxidative stress. Am J Pathol 2002; 161: 1773–1781.
Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, Smith RA, Gerling IC, Weber KT . Hyperparathyroidism and the calcium paradox of aldosteronism. Circulation 2005; 111: 871–878.
Takeda Y . Effects of eplerenone, a selective mineralocorticoid receptor antagonist, on clinical and experimental salt-sensitive hypertension. Hypertens Res 2009; 32: 321–324.
Manning Jr RD, Tian N, Meng S . Oxidative stress and antioxidant treatment in hypertension and the associated renal damage. Am J Nephrol 2005; 25: 311–317.
Brilla CG, Janicki JS, Weber KT . Impaired diastolic function and coronary reserve in genetic hypertension: role of interstitial fibrosis and medial thickening of intramyocardial coronary arteries. Circ Res 1991; 69: 107–115.
Brilla CG, Weber KT . Mineralocorticoid excess, dietary sodium and myocardial fibrosis. J Lab Clin Med 1992; 120: 893–901.
Brilla CG, Pick R, Tan LB, Janicki JS, Weber KT . Remodeling of the rat right and left ventricle in experimental hypertension. Circ Res 1990; 67: 1355–1364.
Laurent GJ . Dynamic state of collagen: pathways of collagen degradation in vivo and their possible role in regulation of collagen mass. Am J Physiol 1987; 252: C1–C9.
López B, González A, Díez J . Circulating biomarkers of collagen metabolism in cardiac diseases. Circulation 2010; 121: 1645–1654.
Zile MR, Brutsaert DL . New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 2002; 105: 1387–1393.
Zile MR, Brutsaert DL . New concepts in diastolic dysfunction and diastolic heart failure: Part II: causal mechanisms and treatment. Circulation 2002; 105: 1503–1508.
Díez J . Towards a new paradigm about hypertensive heart disease. Med Clin North Am 2009; 93: 637–645.
Pearlman ES, Weber KT, Janicki JS, Pietra G, Fishman AP . Muscle fiber orientation and connective tissue content in the hypertrophied human heart. Lab Invest 1982; 46: 158–164.
Huysman JAN, Vliegen HW, Van der Laarse A, Eulderink F . Changes in nonmyocyte tissue composition associated with pressure overload of hypertrophic human hearts. Pathol Res Pract 1989; 184: 577–581.
Sun Y, Ramires FJA, Weber KT . Fibrosis of atria and great vessels in response to angiotensin II or aldosterone infusion. Cardiovasc Res 1997; 35: 138–147.
Weber KT . Aldosterone in congestive heart failure. N Engl J Med 2001; 345: 1689–1697.
Young M, Fullerton M, Dilley R, Funder J . Mineralocorticoids, hypertension, and cardiac fibrosis. J Clin Invest 1994; 93: 2578–2583.
Garnier A, Bendall JK, Fuchs S, Escoubet B, Rochais F, Hoerter J, Nehme J, Ambroisine ML, De Angelis N, Morineau G, d’Estienne P, Fischmeister R, Heymes C, Pinet F, Delcayre C . Cardiac specific increase in aldosterone production induces coronary dysfunction in aldosterone synthase-transgenic mice. Circulation 2004; 110: 1819–1825.
Sheppard K, Funder JW . Mineralocorticoid specificity of renal type I receptors: in vivo binding studies. Am J Physiol 1987; 252 (Part 1): E224–E229.
Suki WN, Schwettmann RS, Rector Jr FC, Seldin DW . Effect of chronic mineralocorticoid administration on calcium excretion in the rat. Am J Physiol 1968; 215: 71–74.
Massry SG, Coburn JW, Chapman LW, Kleeman CR . The effect of long-term desoxycorticosterone acetate administration on the renal excretion of calcium and magnesium. J Lab Clin Med 1968; 71: 212–219.
Gehr MK, Goldberg M . Hypercalciuria of mineralocorticoid escape: clearance and micropuncture studies in the rat. Am J Physiol 1986; 251 (Part 2): F879–F888.
Cappuccio FP, Markandu ND, MacGregor GA . Renal handling of calcium and phosphate during mineralocorticoid administration in normal subjects. Nephron 1988; 48: 280–283.
Rastegar A, Agus Z, Connor TB, Goldberg M . Renal handling of calcium and phosphate during mineralocorticoid ‘escape’ in man. Kidney Int 1972; 2: 279–286.
Zikos D, Langman C, Gafter U, Delahaye B, Lau K . Chronic DOCA treatment increases Ca absorption: role of hypercalciuria and vitamin D. Am J Physiol 1986; 251 (Part 1): E279–E284.
Rossi E, Perazzoli F, Negro A, Sani C, Davoli S, Dotti C, Casoli MC, Regolisti G . Acute effects of intravenous sodium chloride load on calcium metabolism and on parathyroid function in patients with primary aldosteronism compared with subjects with essential hypertension. Am J Hypertens 1998; 11: 8–13.
Berthelot A, Pernot F, Gairard A . Influence of the thyroid and parathyroid glands on magnesium metabolism during mineralocorticoid treatment (DOCA+NaCl) in the rat. Ann Nutr Metab 1983; 27: 349–354.
Horton R, Biglieri EG . Effect of aldosterone on the metabolism of magnesium. J Clin Endocrinol Metab 1962; 22: 1187–1192.
Rossi E, Sani C, Perazzoli F, Casoli MC, Negro A, Dotti C . Alterations of calcium metabolism and of parathyroid function in primary aldosteronism, and their reversal by spironolactone or by surgical removal of aldosterone-producing adenomas. Am J Hypertens 1995; 8: 884–893.
Sellmeyer DE, Schloetter M, Sebastian A . Potassium citrate prevents increased urine calcium excretion and bone resorption induced by a high sodium chloride diet. J Clin Endocrinol Metab 2002; 87: 2008–2012.
Chan EL, Swaminathan R . Effect of different amounts of sodium intake for 4 months on calcium metabolism in normal and oophorectomized rats. J Bone Miner Res 1993; 8: 1185–1189.
Goulding A, Campbell D . Dietary NaCl loads promote calciuria and bone loss in adult oophorectomized rats consuming a low calcium diet. J Nutr 1983; 113: 1409–1414.
Goulding A, Gold E . Effects of dietary sodium chloride loading on parathyroid function, 1,25-dihydroxyvitamin D, calcium balance, and bone metabolism in female rats during chronic prednisolone administration. Endocrinology 1986; 119: 2148–2154.
Creedon A, Cashman KD . The effect of high salt and high protein intake on calcium metabolism, bone composition and bone resorption in the rat. Br J Nutr 2000; 84: 49–56.
Teucher B, Dainty JR, Spinks CA, Majsak-Newman G, Berry DJ, Hoogewerff JA, Foxall RJ, Jakobsen J, Cashman KD, Flynn A, Fairweather-Tait SJ . Sodium and bone health: impact of moderately high and low salt intakes on calcium metabolism in postmenopausal women. J Bone Miner Res 2008; 23: 1477–1485.
Yu HC, Burrell LM, Black MJ, Wu LL, Dilley RJ, Cooper ME, Johnston CI . Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation 1998; 98: 2621–2628.
Lal A, Veinot JP, Leenen FH . Prevention of high salt diet-induced cardiac hypertrophy and fibrosis by spironolactone. Am J Hypertens 2003; 16: 319–323.
Titze J, Rittweger J, Dietsch P, Krause H, Schwind KH, Engelke K, Lang R, Kirsch KA, Luft FC, Hilgers KF . Hypertension, sodium retention, calcium excretion and osteopenia in Dahl rats. J Hypertens 2004; 22: 803–810.
Zou AP, Cowley Jr AW . Role of nitric oxide in the control of renal function and salt sensitivity. Curr Hypertens Rep 1999; 1: 178–186.
Granger JP, Kassab S, Novak J, Reckelhoff JF, Tucker B, Miller MT . Role of nitric oxide in modulating renal function and arterial pressure during chronic aldosterone excess. Am J Physiol 1999; 276 (Part 2): R197–R202.
Morrissey JJ, Cohn DV . The effects of calcium and magnesium on the secretion of parathormone and parathyroid secretory protein by isolated porcine parathyroid cells. Endocrinology 1978; 103: 2081–2090.
Mayer GP, Hurst JG . Comparison of the effects of calcium and magnesium on parathyroid hormone secretion rate in calves. Endocrinology 1978; 102: 1803–1814.
Fertig A, Webley M, Lynn JA . Primary hyperparathyroidism in a patient with Conn's syndrome. Postgrad Med J 1980; 56: 45–47.
Hellman DE, Kartchner M, Komar N, Mayes D, Pitt M . Hyperaldosteronism, hyperparathyroidism, medullary sponge kidneys, and hypertension. JAMA 1980; 244: 1351–1353.
Resnick LM, Laragh JH . Calcium metabolism and parathyroid function in primary aldosteronism. Am J Med 1985; 78: 385–390.
Palmieri GM, Hawrylko J . Effects of aldosterone on the urinary excretion of total and non-dialyzable hydroxyproline. Horm Metab Res 1977; 9: 507–509.
Somers MJ, Mavromatis K, Galis ZS, Harrison DG . Vascular superoxide production and vasomotor function in hypertension induced by deoxycorticosterone acetate-salt. Circulation 2000; 101: 1722–1728.
Pu Q, Neves MF, Virdis A, Touyz RM, Schiffrin EL . Endothelin antagonism on aldosterone-induced oxidative stress and vascular remodeling. Hypertension 2003; 42: 49–55.
Virdis A, Neves MF, Amiri F, Viel E, Touyz RM, Schiffrin EL . Spironolactone improves angiotensin-induced vascular changes and oxidative stress. Hypertension 2002; 40: 504–510.
Gandhi MS, Deshmukh PA, Kamalov G, Zhao T, Zhao W, Whaley JT, Tichy JR, Bhattacharya SK, Ahokas RA, Sun Y, Gerling IC, Weber KT . Causes and consequences of zinc dyshomeostasis in rats with chronic aldosteronism. J Cardiovasc Pharmacol 2008; 52: 245–252.
Fleckenstein A, Frey M, Fleckenstein-Grun G . Consequences of uncontrolled calcium entry and its prevention with calcium antagonists. Eur Heart J 1983; 4 (Suppl H): 43–50.
Ahokas RA, Sun Y, Bhattacharya SK, Gerling IC, Weber KT . Aldosteronism and a proinflammatory vascular phenotype. Role of Mg2+, Ca2+ and H2O2 in peripheral blood mononuclear cells. Circulation 2005; 111: 51–57.
Ahokas RA, Warrington KJ, Gerling IC, Sun Y, Wodi LA, Herring PA, Lu L, Bhattacharya SK, Postlethwaite AE, Weber KT . Aldosteronism and peripheral blood mononuclear cell activation. A neuroendocrine–immune interface. Circ Res 2003; 93: e124–e135.
Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, Smith RA, Gerling IC, Weber KT . Loss of bone minerals and strength in rats with aldosteronism. Am J Physiol Heart Circ Physiol 2004; 287: H2023–H2026.
Fujita T, Palmieri GM . Calcium paradox disease: calcium deficiency prompting secondary hyperparathyroidism and cellular calcium overload. J Bone Miner Metab 2000; 18: 109–125.
Smogorzewski M, Zayed M, Zhang YB, Roe J, Massry SG . Parathyroid hormone increases cytosolic calcium concentration in adult rat cardiac myocytes. Am J Physiol 1993; 264: H1998–H2006.
Perna AF, Smogorzewski M, Massry SG . Effects of verapamil on the abnormalities in fatty acid oxidation of myocardium. Kidney Int 1989; 36: 453–457.
Rampe D, Lacerda AE, Dage RC, Brown AM . Parathyroid hormone: an endogenous modulator of cardiac calcium channels. Am J Physiol 1991; 261 (Part 2): H1945–H1950.
Nordquist RE, Palmieri MA . Intracellular localization of parathyroid hormone in the kidney. Endocrinology 1974; 95: 229–237.
Deluca HF, Engstrom GW, Rasmussen H . The action of vitamin D and parathyroid hormone in vitro on calcium uptake and release by kidney mitochondria. Proc Natl Acad Sci USA 1962; 48: 1604–1609.
Sallis JD, Deluca HF, Rasmussen H . Parathyroid hormone-dependent uptake of inorganic phosphate by mitochondria. J Biol Chem 1963; 238: 4098–4102.
Sallis JD, DeLuca HF . Action of parathyroid hormone on mitochondria. Magnesium- and phosphate-independent respiration. J Biol Chem 1966; 241: 1122–1127.
Kimmich GA, Rasmussen H . The effect of parathyroid hormone on mitochondrial ion transport in the terminal portion of the cytochrome chain. Biochim Biophys Acta 1966; 113: 457–466.
Rasmussen H, Ogata E . Parathyroid hormone and the reactions of mitochondria to cations. Biochemistry 1966; 5: 733–745.
Massry SG, Smogorzewski M . Mechanisms through which parathyroid hormone mediates its deleterious effects on organ function in uremia. Semin Nephrol 1994; 14: 219–231.
Touyz RM . Reactive oxygen species as mediators of calcium signaling by angiotensin II: implications in vascular physiology and pathophysiology. Antioxid Redox Signal 2005; 7: 1302–1314.
Palty R, Silverman WF, Hershfinkel M, Caporale T, Sensi SL, Parnis J, Nolte C, Fishman D, Shoshan-Barmatz V, Herrmann S, Khananshvili D, Sekler I . NCLX is an essential component of mitochondrial Na+/Ca2+ exchange. Proc Natl Acad Sci USA 2010; 107: 436–441.
Kuo TH, Zhu L, Golden K, Marsh JD, Bhattacharya SK, Liu BF . Altered Ca2+ homeostasis and impaired mitochondrial function in cardiomyopathy. Mol Cell Biochem 2002; 238: 119–127.
Kamalov G, Ahokas RA, Zhao W, Johnson PL, Shahbaz AU, Bhattacharya SK, Sun Y, Gerling IC, Weber KT . Temporal responses to intrinsically coupled calcium and zinc dyshomeostasis in cardiac myocytes and mitochondria during aldosteronism. Am J Physiol Heart Circ Physiol 2010; 298: H385–H394.
Goodwin KD, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT . Preventing oxidative stress in rats with aldosteronism by calcitriol and dietary calcium and magnesium supplements. Am J Med Sci 2006; 332: 73–78.
Vidal A, Sun Y, Bhattacharya SK, Ahokas RA, Gerling IC, Weber KT . Calcium paradox of aldosteronism and the role of the parathyroid glands. Am J Physiol Heart Circ Physiol 2006; 290: H286–H294.
Yang F, Nickerson PA . Effect of parathyroidectomy on arterial hypertrophy, vascular lesions, and aortic calcium content in deoxycorticosterone-induced hypertension. Res Exp Med (Berl) 1988; 188: 289–297.
Selektor Y, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT . Cinacalcet and the prevention of secondary hyperparathyroidism in rats with aldosteronism. Am J Med Sci 2008; 335: 105–110.
Thomas M, Vidal A, Bhattacharya SK, Ahokas RA, Sun Y, Gerling IC, Weber KT . Zinc dyshomeostasis in rats with aldosteronism. Response to spironolactone. Am J Physiol Heart Circ Physiol 2007; 293: H2361–H2366.
Selektor Y, Parker RB, Sun Y, Zhao W, Bhattacharya SK, Weber KT . Tissue 65Zinc translocation in a rat model of chronic aldosteronism. J Cardiovasc Pharmacol 2008; 51: 359–364.
Aureli L, Gioia M, Cerbara I, Monaco S, Fasciglione GF, Marini S, Ascenzi P, Topai A, Coletta M . Structural bases for substrate and inhibitor recognition by matrix metalloproteinases. Curr Med Chem 2008; 15: 2192–2222.
Kamalov G, Deshmukh PA, Baburyan NY, Gandhi MS, Johnson PL, Ahokas RA, Bhattacharya SK, Sun Y, Gerling IC, Weber KT . Coupled calcium and zinc dyshomeostasis and oxidative stress in cardiac myocytes and mitochondria of rats with chronic aldosteronism. J Cardiovasc Pharmacol 2009; 53: 414–423.
Wang J, Song Y, Elsherif L, Song Z, Zhou G, Prabhu SD, Saari JT, Cai L . Cardiac metallothionein induction plays the major role in the prevention of diabetic cardiomyopathy by zinc supplementation. Circulation 2006; 113: 544–554.
Karagulova G, Yue Y, Moreyra A, Boutjdir M, Korichneva I . Protective role of intracellular zinc in myocardial ischemia/reperfusion is associated with preservation of protein kinase C isoforms. J Pharmacol Exp Ther 2007; 321: 517–525.
Chvapil M, Owen JA . Effect of zinc on acute and chronic isoproterenol induced heart injury. J Mol Cell Cardiol 1977; 9: 151–159.
Lossnitzer K, Janke J, Hein B, Stauch M, Fleckenstein A . Disturbed myocardial calcium metabolism: a possible pathogenetic factor in the hereditary cardiomyopathy of the Syrian hamster. Recent Adv Stud Cardiac Struct Metab 1975; 6: 207–217.
Bhattacharya SK, Johnson PL, Thakar JH . Reversal of impaired oxidative phosphorylation and calcium overloading in the in vitro cardiac mitochondria of CHF-146 dystrophic hamsters with hereditary muscular dystrophy. J Neurol Sci 1993; 120: 180–186.
Palmieri GM, Nutting DF, Bhattacharya SK, Bertorini TE, Williams JC . Parathyroid ablation in dystrophic hamsters. Effects on Ca content and histology of heart, diaphragm, and rectus femoris. J Clin Invest 1981; 68: 646–654.
Bhattacharya SK, Palmieri GM, Bertorini TE, Nutting DF . The effects of diltiazem in dystrophic hamsters. Muscle Nerve 1982; 5: 73–78.
Crawford AJ, Bhattacharya SK . Excessive intracellular zinc accumulation in cardiac and skeletal muscles of dystrophic hamsters. Exp Neurol 1987; 95: 265–276.
Kamalov G, Ahokas RA, Zhao W, Zhao T, Shahbaz AU, Johnson PL, Bhattacharya SK, Sun Y, Gerling IC, Weber KT . Uncoupling the coupled calcium and zinc dyshomeostasis in cardiac myocytes and mitochondria seen in aldosteronism. J Cardiovasc Pharmacol 2010; 55: 248–254.
Sensi SL, Paoletti P, Bush AI, Sekler I . Zinc in the physiology and pathology of the CNS. Nat Rev Neurosci 2009; 10: 780–791.
Muller DN, Mervaala EM, Schmidt F, Park JK, Dechend R, Genersch E, Breu V, Löffler BM, Ganten D, Schneider W, Haller H, Luft FC . Effect of bosentan on NF-κB, inflammation, and tissue factor in angiotensin II-induced end-organ damage. Hypertension 2000; 36: 282–290.
Müller DN, Mervaala EM, Dechend R, Fiebeler A, Park JK, Schmidt F, Theuer J, Breu V, Mackman N, Luther T, Schneider W, Gulba D, Ganten D, Haller H, Luft FC . Angiotensin II (AT1) receptor blockade reduces vascular tissue factor in angiotensin II-induced cardiac vasculopathy. Am J Pathol 2000; 157: 111–122.
Park JK, Muller DN, Mervaala EM, Dechend R, Fiebeler A, Schmidt F, Bieringer M, Schafer O, Lindschau C, Schneider W, Ganten D, Luft FC, Haller H . Cerivastatin prevents angiotensin II-induced renal injury independent of blood pressure- and cholesterol-lowering effects. Kidney Int 2000; 58: 1420–1430.
Park JK, Fiebeler A, Muller DN, Mervaala EM, Dechend R, Abou-Rebyeh F, Luft FC, Haller H . Lacidipine inhibits adhesion molecule and oxidase expression independent of blood pressure reduction in angiotensin-induced vascular injury. Hypertension 2002; 39 (Part 2): 685–689.
Rocha R, Rudolph AE, Frierdich GE, Nachowiak DA, Kekec BK, Blomme EA, McMahon EG, Delyani JA . Aldosterone induces a vascular inflammatory phenotype in the rat heart. Am J Physiol 2002; 283: H1802–H1810.
Muller DN, Dechend R, Mervaala EM, Park JK, Schmidt F, Fiebeler A, Theuer J, Breu V, Ganten D, Haller H, Luft FC . NF-κB inhibition ameliorates angiotensin II-induced inflammatory damage in rats. Hypertension 2000; 35 (Part 2): 193–201.
Mervaala EM, Müller DN, Park JK, Schmidt F, Löhn M, Breu V, Dragun D, Ganten D, Haller H, Luft FC . Monocyte infiltration and adhesion molecules in a rat model of high human renin hypertension. Hypertension 1999; 33 (Part 2): 389–395.
Ammarguellat FZ, Gannon PO, Amiri F, Schiffrin EL . Fibrosis, matrix metalloproteinases, and inflammation in the heart of DOCA-salt hypertensive rats: role of ETA receptors. Hypertension 2002; 39 (Part 2): 679–684.
Mervaala E, Finckenberg P, Lapatto R, Muller DN, Park JK, Dechend R, Ganten D, Vapaatalo H, Luft FC . Lipoic acid supplementation prevents angiotensin II-induced renal injury. Kidney Int 2003; 64: 501–508.
Theuer J, Dechend R, Muller DN, Park JK, Fiebeler A, Barta P, Ganten D, Haller H, Dietz R, Luft FC . Angiotensin II induced inflammation in the kidney and in the heart of double transgenic rats. BMC Cardiovasc Disord 2002; 2: 3.
Laursen JB, Rajagopalan S, Galis Z, Tarpey M, Freeman BA, Harrison DG . Role of superoxide in angiotensin II-induced but not catecholamine-induced hypertension. Circulation 1997; 95: 588–593.
Haugen EN, Croatt AJ, Nath KA . Angiotensin II induces renal oxidant stress in vivo and heme oxygenase-1 in vivo and in vitro. Kidney Int 2000; 58: 144–152.
Beswick RA, Zhang H, Marable D, Catravas JD, Hill WD, Webb RC . Long-term antioxidant administration attenuates mineralocorticoid hypertension and renal inflammatory response. Hypertension 2001; 37 (Part 2): 781–786.
Piqueras L, Kubes P, Alvarez A, O’Connor E, Issekutz AC, Esplugues JV, Sanz MJ . Angiotensin II induces leukocyte–endothelial cell interactions in vivo via AT1 and AT2 receptor-mediated P-selectin upregulation. Circulation 2000; 102: 2118–2123.
Touyz RM, Schiffrin EL . Angiotensin II and vasopressin modulate intracellular free magnesium in vascular smooth muscle cells through Na+-dependent protein kinase C pathways. J Biol Chem 1996; 271: 24353–24358.
Delva P, Pastori C, Degan M, Montesi G, Brazzarola P, Lechi A . Intralymphocyte free magnesium in patients with primary aldosteronism: aldosterone and lymphocyte magnesium homeostasis. Hypertension 2000; 35: 113–117.
Gerling IC, Sun Y, Ahokas RA, Wodi LA, Bhattacharya SK, Warrington KJ, Postlethwaite AE, Weber KT . Aldosteronism: an immunostimulatory state precedes the proinflammatory/fibrogenic cardiac phenotype. Am J Physiol Heart Circ Physiol 2003; 285: H813–H821.
Perry III HM, Chappel JC, Bellorin-Font E, Tamao J, Martin KJ, Teitelbaum SL . Parathyroid hormone receptors in circulating human mononuclear leukocytes. J Biol Chem 1984; 259: 5531–5535.
Klinger M, Alexiewicz JM, Linker-Israeli M, Pitts TO, Gaciong Z, Fadda GZ, Massry SG . Effect of parathyroid hormone on human T cell activation. Kidney Int 1990; 37: 1543–1551.
Alexiewicz JM, Gaciong Z, Klinger M, Linker-Israeli M, Pitts TO, Massry SG . Evidence of impaired T cell function in hemodialysis patients: potential role for secondary hyperparathyroidism. Am J Nephrol 1990; 10: 495–501.
Ori Y, Korzets A, Malachi T, Gafter U, Breitbart H . Impaired lymphocyte calcium metabolism in end-stage renal disease: enhanced influx, decreased efflux, and reduced response to mitogen. J Lab Clin Med 1999; 133: 391–400.
Reth M . Hydrogen peroxide as second messenger in lymphocyte activation. Nat Immunol 2002; 3: 1129–1134.
Fornes P, Richer C, Vacher E, Bruneval P, Giudicelli JF . Losartan's protective effects in stroke-prone spontaneously hypertensive rats persist durably after treatment withdrawal. J Cardiovasc Pharmacol 1993; 22: 305–313.
Fiebeler A, Schmidt F, Müller DN, Park JK, Dechend R, Bieringer M, Shagdarsuren E, Breu V, Haller H, Luft FC . Mineralocorticoid receptor affects AP-1 and nuclear factor-κB activation in angiotensin II-induced cardiac injury. Hypertension 2001; 37 (Part 2): 787–793.
Rocha R, Stier Jr CT, Kifor I, Ochoa-Maya MR, Rennke HG, Williams GH, Adler GK . Aldosterone: a mediator of myocardial necrosis and renal arteriopathy. Endocrinology 2000; 141: 3871–3878.
Park JB, Schiffrin EL . Cardiac and vascular fibrosis and hypertrophy in aldosterone-infused rats: role of endothelin-1. Am J Hypertens 2002; 15: 164–169.
Dworkin LD, Levin RI, Benstein JA, Parker M, Ullian ME, Kim Y, Feiner HD . Effects of nifedipine and enalapril on glomerular injury in rats with deoxycorticosterone-salt hypertension. Am J Physiol 1990; 259 (Part 2): F598–F604.
Ramires FJA, Sun Y, Weber KT . Myocardial fibrosis associated with aldosterone or angiotensin II administration: attenuation by calcium channel blockade. J Mol Cell Cardiol 1998; 30: 475–483.
Nakamura R, Egashira K, Machida Y, Hayashidani S, Takeya M, Utsumi H, Tsutsui H, Takeshita A . Probucol attenuates left ventricular dysfunction and remodeling in tachycardia-induced heart failure: roles of oxidative stress and inflammation. Circulation 2002; 106: 362–367.
Weglicki WB, Kramer JH, Mak IT . The role of antioxidant drugs in oxidative injury of cardiovascular tissue. Heart Fail Rev 1999; 4: 183–192.
Muller DN, Shagdarsuren E, Park JK, Dechend R, Mervaala E, Hampich F, Fiebeler A, Ju X, Finckenberg P, Theuer J, Viedt C, Kreuzer J, Heidecke H, Haller H, Zenke M, Luft FC . Immunosuppressive treatment protects against angiotensin II-induced renal damage. Am J Pathol 2002; 161: 1679–1693.
Hill MF, Singal PK . Antioxidant and oxidative stress changes during heart failure subsequent to myocardial infarction in rats. Am J Pathol 1996; 148: 291–300.
Dechend R, Fiebler A, Lindschau C, Bischoff H, Muller D, Park JK, Dietz R, Haller H, Luft FC . Modulating angiotensin II-induced inflammation by HMG Co-A reductase inhibition. Am J Hypertens 2001; 14 (Part 2): 55S–61S.
Dechend R, Fiebeler A, Park JK, Muller DN, Theuer J, Mervaala E, Bieringer M, Gulba D, Dietz R, Luft FC, Haller H . Amelioration of angiotensin II-induced cardiac injury by a 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor. Circulation 2001; 104: 576–581.
Kido M, Ando K, Oba S, Fujita T . Renoprotective effect of pravastatin in salt-loaded Dahl salt-sensitive rats. Hypertens Res 2005; 28: 1009–1015.
Ishibashi M, Egashira K, Hiasa K, Inoue S, Ni W, Zhao Q, Usui M, Kitamoto S, Ichiki T, Takeshita A . Antiinflammatory and antiarteriosclerotic effects of pioglitazone. Hypertension 2002; 40: 687–693.
Wayman NS, Hattori Y, McDonald MC, Mota-Filipe H, Cuzzocrea S, Pisano B, Chatterjee PK, Thiemermann C . Ligands of the peroxisome proliferator-activated receptors (PPAR-gamma and PPAR-alpha) reduce myocardial infarct size. FASEB J 2002; 16: 1027–1040.
Yue Tl TL, Chen J, Bao W, Narayanan PK, Bril A, Jiang W, Lysko PG, Gu JL, Boyce R, Zimmerman DM, Hart TK, Buckingham RE, Ohlstein EH . In vivo myocardial protection from ischemia/reperfusion injury by the peroxisome proliferator-activated receptor-γ agonist rosiglitazone. Circulation 2001; 104: 2588–2594.
Iglarz M, Touyz RM, Viel EC, Paradis P, Amiri F, Diep QN, Schiffrin EL . Peroxisome proliferator-activated receptor-α and receptor-γ activators prevent cardiac fibrosis in mineralocorticoid-dependent hypertension. Hypertension 2003; 42 (Part 2): 737–743.
Ogata T, Miyauchi T, Sakai S, Takanashi M, Yamaguchi I . A PPAR-α activator inhibits myocardial fibrosis and diastolic dysfunction of the heart in DOCA-salt hypertensive rats, via suppressing inflammatory gene responses by a NF-κB pathway. Circulation 2003; 108 (Suppl IV): IV–59.
Essayan DM . Cyclic nucleotide phosphodiesterases. J Allergy Clin Immunol 2001; 108: 671–680.
Zatz R, Noronha IL, Fujihara CK . Experimental and clinical rationale for use of MMF in nontransplant progressive nephropathies. Am J Physiol Renal Physiol 2002; 283: F1167–F1175.
Acknowledgements
This work was supported, in part, by NIH Grants R01-HL73043 and R01-HL90867 (KTW). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zia, A., Kamalov, G., Newman, K. et al. From aldosteronism to oxidative stress: the role of excessive intracellular calcium accumulation. Hypertens Res 33, 1091–1101 (2010). https://doi.org/10.1038/hr.2010.159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.159
Keywords
This article is cited by
-
Hyperparathyroidism in patients with overt and mild primary aldosteronism
Hormones (2021)
-
Role of the renin–angiotensin–aldosterone system in bone metabolism
Journal of Bone and Mineral Metabolism (2020)
-
Vitamin D deficiency is an independent predictor of mortality in patients with chronic heart failure
European Journal of Nutrition (2019)
-
Evaluation of left ventricle functions by tissue Doppler, strain, and strain rate echocardiography in patients with primary hyperparathyroidism
Endocrine (2014)
-
Salt, the renin–angiotensin–aldosterone system and resistant hypertension
Hypertension Research (2013)