Abstract
The aim of this study was to compare the effects of nifedipine coat-core (once daily formulation) and amlodipine on systemic arterial stiffness in patients with hypertension. Study drugs were assigned by the randomized open-label crossover method. After the blood pressure was maintained below 130/85 mm Hg for 8 months by treatment with either drug in 48 hypertensive patients (aged 63.2±6.9 years; 64.5% men), they were switched to the other drug for another 8 months. The blood pressure, heart rate, plasma catecholamine level and brachial-ankle pulse wave velocity were measured before and after a bicycle ergometer testing. Heart rate recovery was calculated from the change of the heart rate after treadmill exercise testing. The high-frequency and low-frequency components of the heart rate variability spectrum were analyzed from 24-h Holter electrocardiograms. The change of blood pressure after exercise testing showed no significant difference between the two medications. However, the increases of heart rate, noradrenalin and branchial-ankle pulse wave velocity after exercise were significantly smaller with nifedipine treatment than with amlodipine (P=0.0472, P=0.006 and P=0.0472, respectively). Heart rate recovery was significantly faster with nifedipine treatment (P=0.0280). The nighttime high-frequency component of heart rate variability was significantly larger after nifedipine treatment than after amlodipine (P=0.0259), while the nighttime low/high-frequency ratio was significantly smaller with nifedipine (P=0.0429). Nifedipine reduced functional arterial stiffness and improved heart rate recovery by altering the autonomic activity balance in hypertensive patients.
Similar content being viewed by others
Introduction
It has been pointed out that autonomic activity are involved in the development of a cardiovascular event due to arteriosclerosis.1, 2 The imbalance of autonomic activity induced by sympathetic and parasympathetic nervous action, in particular, is closely related with arterial stiffness.3 Increased arterial stiffness may lead to overload on the heart in terms of increases in heart rate (HR) and blood pressure (BP), and adversely influences the prognosis of a patient.4, 5 It is important in the treatment of hypertension to avoid an undesirable influence on the autonomic activity as well as to achieve strict BP reduction. The brachial-ankle pulse wave velocity (Ba-PWV) is currently used as an indicator of arterial stiffness,6, 7 whereas the spectral analysis of heart rate variability8, 9 and measurement of plasma catecholamines are methods of evaluating autonomic function. Long-acting calcium channel blockers (CCBs) have been demonstrated to prevent cardiovascular events in large-scale clinical trials,10, 11 but it remains unclear whether these drugs influence the arterial stiffness and autonomic activity balance. It has also been reported that dihydropyridine CCBs vary with respect to their antihypertensive and antiatherogenic effects.12, 13, 14
This study was designed to compare the effects of long-acting nifedipine (NIF) and amlodipine (AML), which are two CCBs commonly used to treat hypertension, on systemic arterial stiffness and autonomic activity balance in Japanese patients with hypertension.
Methods
Subjects
This study enrolled outpatients of Kitasato University Hospital from March 2004 to March 2006. The study was approved by the Ethics Committee of Kitasato University Hospital, and written informed consent was obtained from all patients after they received a detailed explanation of the study protocol. Forty-eight patients with essential hypertension were enrolled by the continual registration method. Essential hypertension was defined as the mean systolic blood pressure (SBP)>140 mm Hg and/or diastolic blood pressure (DBP)>90 mm Hg at the outpatient clinic on several visits, after a secondary hypertension was ruled out. Inclusion criteria were sinus rhythm on an electrocardiogram (ECG) and current treatment with antihypertensive agents. Exclusion criteria were frequent extrasystoles, significant coronary stenosis, unstable angina pectoris, prior myocardial infarction, heart failure, chronic renal failure, or diabetes mellitus.
Treatments and study design
Using 20 or 40 mg tablets of NIF and 2.5 or 5.0 mg tablets of AML, the dosages were set as follows: AML at 2.5 mg day−1=NIF at 20 mg day−1 and AML at 5.0 mg day−1=NIF at 40 mg day−1. This was done on the basis of previous Japanese clinical studies indicating that these dosages have an equivalent antihypertensive effect.15, 16 The study was performed by the open-label crossover method.
Patients were randomized to the NIF-first group or AML-first group and then took NIF or AML once daily after breakfast for 8 months. If other CCBs were already being administered, those agents were switched to the study drug, while administration of other non-CCB antihypertensive agents was continued without changing the dosage. The dose titration period of each study drug was for 2 months to achieve the target BP, which was less than 130/85 mm Hg. If the target BP was not attained during the dose titration period by study drugs, the patient was a dropout for the study. After the dosage was fixed, each treatment was continued at that dose for 6 months (totally 8 months treatment period). At the end of the first treatment period, exercise tests were done using a bicycle ergometer and a treadmill to assess systemic arterial stiffness and exercise tolerance, respectively, and measurement of biochemical variables was performed. Then the patients were switched to the other study drug for a further 8 months, with exercise testing and laboratory studies being done in the same manner at the end of the second treatment period.
Assessment of systemic arterial stiffness and heart rate recovery
Exercise testing was carried out with a bicycle ergometer (Well Bike BE-360, Fukuda Denshi, Tokyo, Japan) at the end of each 8-month treatment period to assess systemic arterial stiffness by measuring Ba-PWV (Omron Colin, Tokyo, Japan). The BP, HR and Ba-PWV were measured two times in the supine position, that is, after the patient had rested for 15 min and also at 10 min after the exercise test (Figure 1). Then the changes from the baseline BP, HR and Ba-PWV at rest to those determined after exercise were calculated (ΔBP, ΔHR and ΔBa-PWV, respectively) and a functional arterial stiffness was assessed by ΔBa-PWV,7 with a negative value indicating greater vascular compliance. The bicycle ergometer exercise test was performed according to the following protocol. After resting for 15 min, patients started exercise on the ergometer at 15 watts for 3 min (warming-up period). Then the target HR was achieved within 3 min by increasing the workload and was maintained for another 10 min (exercise period). The target HR was set at 75% of the maximum HR measured during a treadmill exercise test performed according to the Bruce protocol.17 After 10 min of rest following 3 min of cooling down, Ba-PWV was re-measured. The 10-min period was enough time to allow the elevated catecholamine levels due to exercise to return to normal.18, 19 All patients were instructed to pedal at 50 r.p.m. during the exercise test. HR and the ECG were monitored continuously using a Stress Test system (ML-1800, Fukuda Denshi), and BP was measured at 1-min intervals by the cuff method using an automatic sphygmomanometer (FB-300, Fukuda Denshi).
Exercise protocol for assessment of functional arterial stiffness. Exercise testing was performed with a bicycle ergometer (3-min warming-up period, 13-min exercise period and 3-min cooling-down period). The target heart rate (HR) was maintained for 10 min during the exercise period, and was set at 75% of the maximum HR reached during a treadmill exercise test using the Bruce protocol. BP: blood pressure, HR: heart rate, Ba-PWV: brachial-ankle pulse wave velocity, NORA: noradrenalin, ADRN: adrenalin, PRA: plasma renin activity, ALDOST: aldosterone.
Heart rate recovery (HRR) was assessed during a treadmill exercise test (ML-6500, Fukuda Denshi) performed according to the Bruce protocol at the end of the 8-month treatment period. It was calculated as the decrease of HR from the maximum during the exercise test to that at 1 min after completion, and was used as an indicator of parasympathetic activity.20
Assessment of autonomic activity
A 24-h Holter ECG recording (FM-300, Fukuda Denshi) was obtained at the end of each treatment period to assess the autonomic activity on the basis of spectral analysis of heart rate variability. The variability of the R-R interval over 24 h was analyzed with MemCalc software (MemCalc, Suwa Trust, Tokyo, Japan) to obtain the low-frequency component (0.04–0.15 Hz) and the high-frequency component (0.15–0.4 Hz) of the power spectrum (LF and HF, respectively), as well as calculating entropy.21 The HF component of the power spectrum is known to reflect parasympathetic activity, and the LF/HF ratio indicates the balance between sympathetic and parasympathetic activity. The average values of the HR, HF component, LF/HF ratio and entropy were calculated over 24 h, during the daytime (0800 to 1700 hours) and during the nighttime (0000 to 0600 hours). Then the daytime/nighttime ratios of these parameters were calculated (HRtotal, HRday, HRnight, HRday/night, HFtotal, HFday, HFnight, HFday/night, LF/HFtotal, LF/HFday, LF/HFnight, LF/HFday/night, Entropytotal, Entropyday, Entropynight and Entropyday/night, respectively).
Plasma concentrations of noradrenalin (NORA) and adrenalin (ADRN), plasma renin activity (PRA) and the plasma aldosterone level (ALDST) were measured before and after the bicycle ergometer test that was performed to assess Ba-PWV. Then the changes from the baseline NORA, ADRN, PRA and ALDST to those after exercise were calculated (ΔNORA, ΔADRN, ΔPRA and ΔBa-PWV, respectively) to determine the response of sympathetic activity to exercise (Figure 1).
Investigation of cardiac and vascular endothelial function
The left atrial dimension (LAD), left ventricular end-diastolic dimension (LVDd), left ventricular end-systolic dimension (LVDs), left ventricular ejection fraction (LVEF) and left ventricular mass (LVM) were measured by echocardiography (Sonos 7500, Philips, Bothell, WA, USA) at the end of each 8-month treatment period. LVM was calculated according to the formula of Devereux and was adjusted for the body surface area.22 All echocardiographic measurements were performed according to the recommendations of the American Society of Echocardiography by an observer who was blinded to the biochemical data.23 Blood samples were obtained from an antecubital vein after an overnight fast for measurement of the serum concentrations of brain natriuretic peptide (BNP), von Willebrand factor (vWF), thrombomodulin and high sensitivity C-reactive protein (hs-CRP) at the end of each treatment period.
Statistical analysis
This was a randomized open crossover study in which NIF coat-core was switched to AML or vice versa. The primary end points were Ba-PWV and the levels of NORA and ADRN after the exercise test. Data were assessed by analysis of variance, including the terms sequence, treatment period, study drug and patient. Results are reported as the mean±s.d. Comparisons of parameters between the two study drugs are also presented as differences between the drugs together with 95% confidence intervals. The paired t-test (two-tailed) was used to compare differences between other variables (LF, HF, Entropy, HRR, BNP, LVEF, LVMI, hs-CRP, vWF, etc.) measured during each treatment period. All statistical analyses were performed with SPSS 12.0J software (SPSS Japan, Tokyo), and P<0.05 was accepted as indicating significance.
Results
The baseline characteristics of the patients are summarized in Table 1. The mean age of the patients was 63.2±6.9 years and they consisted of 31 men and 17 women. Dyslipidemia was detected in 36.7% of the patients and 30.0% were smokers. The average daily doses of NIF and AML were 30.6±13.1 mg and 4.5±1.8 mg, respectively, at the time when the target BP (<130/85 mm Hg) was achieved. The other antihypertensive drugs used concomitantly were angiotensin II receptor blockers (53.3%), angiotensin-converting enzyme inhibitors (10.0%), β-blockers (40.0%), α-blockers (10.0%) and diuretics (23.3%). At the outpatient clinic, the average SBP/DBP and HR after treatments by AML or NIF were 125.3±6.7/67.0±6.6 mm Hg, 67.8±7.9 beats min−1, or 124.7±6.9/66.5±7.1 mm Hg, 66.6±8.0 beats min−1, respectively.
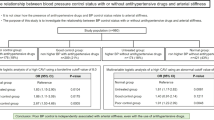
The values of BP, HR, Ba-PWV and neurohumoral factors measured before and after the bicycle ergometer exercise test are shown in Table 2. There were no significant differences of SBP and DBP before or after exercise between the two treatments. According to analysis of variance, there was no influence of the sequence and treatment period. Although no significant differences of baseline HR, Ba-PWV and neurohumoral factors were also shown between the two medications, there were significantly lower HR, Ba-PWV, NORA and PRA after the exercise test following NIF treatment compared with after AML treatment (P=0.0472, P=0.0433, P=0.0006 and P=0.0082, respectively).
The changes of HR and Ba-PWV after the bicycle ergometer exercise test are shown in Figure 2. The increase of ΔHR was significantly smaller with NIF treatment than with AML treatment (P=0.0472). ΔBa-PWV were increased with AML treatment but decreased with NIF treatment (P=0.0433).
Changes of the heart rate (left) and Ba-PWV (right) during the bicycle ergometer exercise test. Open squares: amlodipine, closed squares: nifedipine coat-core. P-values: amlodipine vs. nifedipine coat-core by the paired t-test. HR: heart rate, Ba-PWV: brachial-ankle pulse wave velocity. ΔHR and ΔBa-PWV: the difference between baseline HR or Ba-PWV and the values measured after bicycle ergometer exercise.
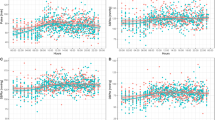
The changes of NORA, ADRN, PRA and ALDST after bicycle ergometer exercise are shown in Figure 3. The increase of ΔNORA and ΔPRA were significantly smaller in NIF treatment than in AML treatment (P=0.0006 and P=0.0093, respectively). There were no significant differences of ΔADRN or ΔALDST between the two medications.
Changes of neurohumoral factors during the bicycle ergometer exercise test. Open squares, amlodipine; closed squares, nifedipine coat-core. P-values, amlodipine vs. nifedipine coat-core by the paired t-test. NORA, noradrenalin; ADRN, adrenalin; PRA, plasma renin activity; ALDOST, aldosterone. ΔNORA, ΔADRN, ΔPRA and ΔBa-PWV; the difference between baseline NORA, ADRN, PRA or ALDST and the values measured after bicycle ergometer exercise.
The HR, HF component, LF/HF ratio and entropy over 24 hours, as well as during the daytime and nighttime, are listed in Table 3. Significantly lower HRnight and higher HRday/night were observed during NIF treatment compared with AML treatment (P=0.0105 and P=0.0083, respectively), although HRtotal showed no significant difference between the two medications. Significantly higher HFnight and lower HFday/night values were observed during NIF treatment compared with AML treatment (P=0.0259 and P=0.0374, respectively). Significantly lower LF/HFnight and higher LF/HFday/night values were also found with NIF treatment than with AML treatment (P=0.0429 and P=0.0166, respectively). Both entropytotal and entropynight showed significantly higher values during NIF treatment than during AML treatment (P=0.0404 and P=0.0358, respectively).
The HRR and cardiac function parameters are summarized in Table 4. Both HRR and LVEF were significantly greater during NIF treatment than during AML treatment (P=0.0280 and P=0.0427, respectively). In contrast, BNP and LVMI values were significantly smaller with NIF treatment than with AML treatment (P=0.0418).
Parameters of vascular endothelial function and inflammation are displayed in Figure 4. Both hs-CRP and vWF were significantly lower with NIF treatment than with AML treatment (P=0.0382 and P=0.0263, respectively).
Discussion
Although there is abundant evidence that long-acting Ca antagonists can improve the prognosis of patients with cardiovascular disease,10, 11, 24 it remains unclear how these drugs correct prognostic factors. This study showed that NIF significantly suppressed the increase of HR and decreased Ba-PWV25 after exercise in hypertensive patients. It is well known that Ba-PWV reflects arterial stiffness more accurately in assessment of arterial pulse-wave velocity.26, 27 Although the antihypertensive effect of NIF was similar to that of AML, its influence on Ba-PWV was significantly stronger. Factors that increase arterial stiffness include hypertension, glucose intolerance, hypercholesterolemia and oxidative stress.28 Arterial stiffness also increases when sympathetic activity is enhanced,3 and such an increase is especially noted during exercise. To clarify the reason why the exercise-related increase of arterial stiffness was suppressed by NIF treatment, we investigated differences in the influence of NIF and AML on heart rate variability and neurohumoral factors. As a result, we found that the HF component (an indicator of parasympathetic activity) was larger and the LF/HF ratio (an indicator of sympathetic activity) was smaller during NIF treatment than during AML treatment. In addition, the increase of entropy was significantly more marked during both daytime and nighttime when patients were receiving NIF than with AML treatment. Entropy is an indicator of the balance of autonomic activity, and an increase of entropy suggests appropriate regulation of autonomic function.29 Nocturnal hypertension is one form of masked hypertension, and it is recognized as an important risk factor for stroke and other cardiovascular events. At night, parasympathetic activity should be dominant and reduce the blood pressure, but sympathetic activity still tends to be dominant in hypertensive patients even in the nighttime. Our findings suggested that NIF may improve the autonomic activity balance compared with the action of AML. This study also showed that ΔNORA and ΔPRA were significantly smaller after exercise during NIF treatment than during AML treatment. Champlain et al.30 compared the effects of AML and NIF in patients with essential hypertension, and reported that the HR and NORA were significantly increased during the latter part of a 6-month treatment period with AML relative to the early part, whereas NORA was significantly reduced during NIF treatment. Our results support those findings and suggest that the significant reduction of ΔBa-PWV observed during NIF treatment is attributable to the improvement of systemic arterial stiffness secondary to correction of the imbalance of autonomic activity. The influence of NIF and AML on HRR, another prognostic factor, was also assessed in this study. Delayed recovery of the heart rate indicates suppression of parasympathetic activity after exercise,31, 32 whereas rapid recovery is considered to be an indicator of a good prognosis in patients with coronary artery disease.33 Our results showed that HRR was significantly faster during NIF treatment than during AML treatment, suggesting that NIF had a more favorable influence on parasympathetic activity than AML.
This study also demonstrated significant improvement of left ventricular hypertrophy along with a decrease of BNP during NIF treatment compared with AML treatment. Cardiac hypertrophy has been reported to progress as a result of reduced nighttime parasympathetic activity,34, 35 so our finding that the nighttime HF component was larger during NIF treatment than during AML treatment may be associated with the inhibitory effect of NIF on ventricular hypertrophy.
The results of 24-h Holter monitoring showed an increase of nighttime parasympathetic activity during NIF treatment compared with AML treatment. Taken together with the difference of HRR after daytime exercise, it seems that NIF rather prevents suppression of parasympathetic activity at night when it should be dominant and improves arterial stiffness by normalizing the autonomic activity balance.
AML and NIF have different effects on sympathetic and parasympathetic activity for the following reasons. First, AML is a highly lipophilic drug with a much higher affinity for cardiac and vascular cell membranes than other dihydropyridines.36 Because AML substantially inhibits Ca channel activity for a long period, it is possible that long-term AML treatment could lead to excessive suppression of vascular compliance so that the vessels no longer respond properly to autonomic regulation. Testa and colleagues37 found that AML treatment had a negative influence on perceived general health, vitality and sleep compared with nifedipine GITS when they surveyed health-related quality of life in hypertensive patients. The controlled-release preparation used in this study maintains an adequate plasma concentration of nifedipine,38 which presumably results in appropriate autonomic regulation of the cardiovascular system. Secondly, our study demonstrated that NIF treatment significantly reduced the levels of hs-CRP and vWF compared with AML, and it suggested that NIF treatment may improve the vascular endothelial function. These findings are supported by reports that NIF has stronger anti-inflammatory activity39 and stronger anti-atherosclerotic effects including an antioxidant action40, 41 than other CCBs. Recently, the ENCORE study from Europe42 demonstrated that long-acting nifedipine GITS improves acetylcholine sensitivity in patients with coronary artery disease, suggesting that NIF treatment could also improve vascular endothelial function.
Study limitations
There are some limitations also on this study as follows: (1) The sample size was not calculated statistically, because the study was exploratory. (2) We have observed the effects of either NIF or AML on arterial stiffness and autonomic balance by measuring of 24-h circadian dynamic change of autonomic activities on 24-h Holter ECG, because the office blood pressures of both drugs were equivalent. We also need to examine nocturnal blood pressure in both drugs by using ambulatory blood pressure monitoring. (3) All of the recruited patients were already treated with any of the CCBs. We could not perform ergometer exercise for baseline measurement after washout of treating CCBs because of the ethical reason. (4) This study did not show the relationship between the improvement of autonomic imbalance and the change of arterial stiffness directly, because both were not measured simultaneously.
Even there are limitations in this study as written above, our results may propose the following hypothesis, which is expected to be proven by further studies.
In conclusion, both NIF and AML controlled the BP well in hypertensive patients without inducing excessive activation of sympathetic nervous system, and in addition, NIF improved systemic arterial stiffness by correcting the imbalance of autonomic activity. Furthermore, our results suggested that NIF had a superior anti-inflammatory effect and improved vascular endothelial function compared with AML.
Conflict of interest
The authors declare no conflict of interest.
References
La Rovere MT, Specchia G, Mortara A, Schwartz PJ . Baroreflex sensitivity, clinical correlates, and cardiovascular mortality among patients with a first myocardial infarction. A prospective study. Circulation 1988; 78: 816–824.
Farrell TG, Paul V, Cripps TR, Malik M, Bennett ED, Ward D, Camm AJ . Baroreflex sensitivity and electrophysiological correlates in patients after acute myocardial infarction. Circulation 1991; 83: 945–952.
Nakao M, Nomura K, Karita K, Nishikitani M, Yano E . Relationship between brachial-ankle pulse wave velocity and heart rate variability in young Japanese men. Hypertens Res 2004; 27: 925–931.
Safar ME, Levy BI . Strujiker-Boudier: current perspective on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation 2003; 107: 2864–2869.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Yamashita A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y . Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Munakata M, Nunokawa T, Tayama J, Yoshinaga K, Toyota T . Brachial-ankle pulse wave velocity as a novel measure of arterial stiffness: present evidence and perspectives. Curr Hypertens Rev 2005; 12: 223–234.
Widgren BR, Wikstrand J, Berglund G, Andersson OK . Increased response to physical and mental stress in men with hypertensive patients. Hypertension 1992; 20: 606–611.
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Circulation 1996; 93: 1043–1065.
Lubsen J, Wagner G, Kirwan BA, Brouwer S, Poole-Wilson PA . Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with symptomatic stable angina and hypertension: the ACTION trial. J Hyperten 2005; 23: 641–648.
Nissen SE, Tuzcu EM, Libby P, Thompson PD, Ghali M, Garza D, Berman L, Shi H, Buebendorf E, Topol EJ, for the CAMELOT Investigators. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure. The CAMELOT Study: a randomized controlled trial. JAMA 2004; 292: 2217–2226.
Kono I, Kugiyama K . Evaluation on antihypertensive effect of nifedipine coat-core and change in pulse pressure in elderly hypertensive patients refractory to amlodipine therapy. Ther Res 2005; 26: 491–497.
Saito I, Saruta T, ADVANCE-Combi Study Group. Controlled release nifedipine and valsartan combination therapy in patients with essential hypertension: the Adalat CR and Valsartan Cost-Effectiveness Combination (ADVANCE-Combi) Study. Hypertens Res 2006; 29: 789–796.
Shinoda E, Yui Y, Kodama K, Hirayama A, Nonogi H, Haze K, Sumiyoshi T, Hosoda S, Kawai C, Japan Multicenter Investigation for Cardiovascular Diseases-B Study Group. Quantitative coronary angiogram analysis: nifedipine retard versus angiotensin-converting enzyme inhibitors (JMIC-B Side arm study). Hypertension 2005; 45: 1153–1158.
Ishii M, Matsuoka H, Iimura O, Yoshinaga K, Yagi S, Saruta T, Kurokawa K, Takeda T, Ogihara T, Fujishima M, Arakawa K, Fukiyama K, Ohashi Y . Clinical efficacy of BAY a 1040-OD (sustained-release nifedipine) in patients with essential hypertension: multicenter open trials of monotherapy and combined therapy (in Japanese). Jpn Pharmacol Ther 1997; 25: 1839–1868.
Masuyama Y, Arita M, Iimura O, Yoshinaga K, Abe K, Inagaki Y, Ishii T, Kuramoto K, Saruta T, Kajiwara N, Mizuno Y, Kumahara Y, Ito K, Arakawa K . A multicenter trial of amlodipine besilate in patients with essential hypertension (in Japanese). Jpn Pharmacol Ther 1991; 19: 2853–2871.
Bruce RA, Rowell LB, Blackmon JR, Doan A . Cardiovascular function tests. Heart Bull 1965; 14: 9–14.
Hagberg JM, Hickson RC, McLane JA, Ehsani AA, Winder WW . Disappearance of norepinephrine from the circulation following strenuous exercise. J Appl Physiol 1979; 47: 1311–1314.
Todd EP, Vick RL . Kalemotropic effect of epinephrine: analysis with adrenergic agonists and antagonists. Am J Physiol 1971; 220: 1964–1969.
Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS . Heart rate recovery immediately after exercise as a predictor of mortality. N Engl J Med 1999; 341: 1351–1357.
Ohtomo N, Kamo T, Watanabe M, Yoneyama K, Tanaka Y, Hayashi R . Power spectral densities of temporal variations of blood pressures. Jpn J Appl Physiol 1996; 35: 5571–5582.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP . Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990; 322: 1561–1566.
Pearlman A, Gardin J, Martin R, Parisi AF, Popp RL, Quinones MA, Stevenson JG . Guidelines for optimal physician training in echocardiography. Recommendations of the American Society of Echocardiography committee for physician training in echocardiography. Am J Cardiol 1987; 60: 158–163.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial.: major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y . Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Schimmler W, Hooffacker M . Spontaneous changes in blood pressure and aortic pulse wave velocity in normotensive subjects (results of a long-term study in 183 men) [author's transl.]. Basic Res Cardiol 1975; 70: 521–530.
Bercu BB, Haupt R, Johnsonbaugh R, Rodbard D . The pulse wave arrival time (QKd interval) in normal children. J Pediatr 1979; 95: 716–721.
Tomiyama H, Kushiro T, Okazaki R, Yoshida H, Doba N, Yamashina A . Influence of increased oxidative stress on endothelial function, platelet function, and fibrinolysis in hypertension associated with glucose intolerance. Hypertens Res 2003; 26: 295–300.
Khalfen ESh, Temkin BM . Clinical value of the study of cardiac rhythm entropy in patients with myocardial infarction. Kardiologiia 1983; 23: 37–41.
Champlain J, Karas M, Nguyen P, Cartier P, Wistaff R, Toal CB, Nadeau R, Larochelle P . Different effects of nifedipine and amlodipine on circulating catecholamine levels in essential hypertensive patients. J Hypertens 1998; 16: 1357–1369.
Imai K, Sato H, Hori M, Kusuoka H, Ozaki H, Yokoyama H, Takeda H, Inoue M, Kamada T . Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J Am Coll Cardiol 1994; 24: 1529–1535.
Pierpont G, Stolpman D, Gornick C . Heart rate recovery post-exercise as an index of parasympathetic activity. J Auton Nerv Syst 2000; 80: 169–174.
Vivekananthen DP, Blackstone EH, Pothier CE, Lauer MS . Heart rate recovery after exercise in a predictor of mortality, independent of the angiographic severity of coronary disease. Am J Cardiol 2003; 42: 831–838.
Petretta M, Marciano F, Bianchi V, Migaux ML, Valva G, De Luca N, Salemme L, Berardino S, Bonaduce D . Power spectrum analysis of heart period variability in hypertensive patients with left ventricular hypertrophy. AJH 1995; 8: 1206–1213.
Kuwajima I, Suzuki Y, Shimosawa T, Kanemaru A, Hoshino S, Kuramoto K . Diminished nocturnal decline in blood pressure in elderly hypertensive patients with left ventricular hypertrophy. Am Heart J 1992; 123: 1307–1311.
Manson RP, Campbell SF, Wang SD, Herbette LG . Comparison of location and binding for the positively charged 1,4-dihydropyridine calcium channel antagonist amlodipine with uncharged drugs of this class in cardiac membranes. Mol Pharmacol 1989; 36: 634–640.
Testa MA, Turner RR, Simonson DC, Krafcik MB, Calvo C, Luque-Otero M . Quality of life and calcium channel blockade with nifedipine GITS versus amlodipine in hypertensive patients in Spain. J Hypertens 1998; 16: 1839–1847.
Nakamichi N, Yanagida T, Hikima Y, Kobayashi N, Shiga K, Tsuji S, Tanaka T, Tamagawa K, Sekino H . Phase-1 study of nifedipine sustained-released formation (BAY a 1040-OD tablets): single administration study. Jpn Pharmacol Ther 1995; 23: S241–S255 (in Japanese).
Matsumori A, Nunokawa Y, Sasayama S . Nifedipine inhibits activation of transcription factor NF-Kb. Life Sci 2000; 67: 2655–2661.
Fukuo K, Yang J, Yasuda O, Mogi M, Suhara T, Sato N, Suzuki T, Morimoto S, Ogihara T . Nifedipine indirectly upregulates superoxide dismutase expression in endothelial cells via vascular smooth muscle cell-dependent pathways. Circulation 2002; 106: 356–361.
Berkels R, Egink G, Marsen TA, Bartels H, Roesen R, Klaus W . Nifedipine increases endothelial nitric oxide bioavailability by antioxidative mechanisms. Hypertension 2001; 37: 240–245.
The ENCORE Investigators. Effect of nifedipine and cerivastatin on coronary endothelial function in patients with coronary artery disease, The ENCORE I Study (Evaluation of nifedipine and cerivastatin on recovery of coronary endothelial function). Circulation 2003; 107: 422–428.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukuda, M., Masuda, T., Ogura, M. et al. Influence of nifedipine coat-core and amlodipine on systemic arterial stiffness modulated by sympathetic and parasympathetic activity in hypertensive patients. Hypertens Res 32, 392–398 (2009). https://doi.org/10.1038/hr.2009.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.18
Keywords
This article is cited by
-
Comparison of short-acting versus extended-release nifedipine: Effects on hemodynamics and sympathetic activity in patients with stable coronary artery disease
Scientific Reports (2020)
-
Musical auditory stimulus acutely influences heart rate dynamic responses to medication in subjects with well-controlled hypertension
Scientific Reports (2018)