Abstract
Fifty years after the implementation of universal newborn screening programs for phenylketonuria, the first disease identified through newborn screening and considered a success story of newborn screening, a cohort of adults with phenylketonuria treated from birth provides valuable information about effects of long-term treatment for inborn errors of metabolism in general, and phenylketonuria specifically. For phenylketonuria, newborn screening allows early implementation of the phenylalanine-restricted diet, eliminating the severe neurocognitive and neuromotor impairment associated with untreated phenylketonuria. However, executive function impairments and psychiatric problems are frequently reported even for those treated early and continuously with the phenylalanine-restricted diet alone. Moreover, a large percentage of adults with phenylketonuria are reported as lost to follow-up by metabolic clinics. While a group of experts identified by the National Institutes of Health convenes to update treatment guidelines for phenylketonuria, we explore individual patient, social, and economic factors preventing >70% of adult phenylketonuria patients in the United States from accessing treatment. As more conditions are identified through newborn screening, factors affecting access to treatment grow in importance, and we must continue to be vigilant in assessing and addressing factors that affect patient treatment outcomes and not just celebrate amelioration of the most severe manifestations of disease.
Genet Med 2013:15(8):591–599
Similar content being viewed by others
Main
In the 1960s, phenylketonuria (PKU, OMIM no. 261600) became the first disease identifiable through universal newborn screening (NBS) programs.1 PKU was first described in two siblings by Følling in 1934.2 In 1937, Jervis and colleagues described the cause of PKU as deficient phenylalanine hydroxylase activity resulting in the inability to convert phenylalanine (Phe) to tyrosine.3 This results in toxic accumulation of Phe in the brain, causing severe neurocognitive and neuromotor impairment.3
Before NBS programs, PKU was generally diagnosed after parents noted delayed developmental skills, by which time, irreversible brain damage had often occurred.4 In California, before the implementation of universal NBS programs, one to two patients were identified annually, with a mean age at diagnosis of 8 years, 2 months. After universal NBS was initiated in California in 1966, approximately 13 patients were diagnosed annually between 1966 and 1968, with mean age of diagnosis decreasing to 8 months.4 Similarly, in the 18 months after the initiation of universal screening in New York State in January 1965, 77 infants were diagnosed with PKU.5
Newborn diagnosis of PKU is considered the first success story of NBS programs because the identification soon after birth permits early implementation of a Phe-restricted diet. This diet restricts dietary Phe intake and requires supplementation with synthetic amino acid–fortified medical foods to ensure a Phe-free protein source with sufficient vitamins and minerals. This treatment, first described by Bickel and colleagues in 1953, eliminated the most severe manifestations of the disorder;3 however, controversy remained.4 Early fears about the reported potential effects of unnecessary protein restriction, such as anorexia, diarrhea, and anemia,6 prevented some clinicians from implementing the Phe-restricted diet until diagnosis was confirmed with secondary testing.7 Experts also disagreed about the degree of elevation of Phe levels above the 60 µmol/l of unaffected individuals, which would indicate the need for dietary treatment. Without detailed information about the outcomes of elevated Phe levels, many clinicians felt that patients with Phe concentrations <1,200 µmol/l did not require treatment, whereas others treated those individuals with levels >900 µmol/l7,8 or even >720 µmol/l.9
Many practitioners in the early 1970s believed that elevated Phe levels would no longer have negative effects once the brain was fully developed. As such, at that time, the Phe-restricted diet was deemed unnecessary after 6 years of age, when the brain was considered nearly fully developed,7 and therefore many supported early diet discontinuation.10,11 However, other experts recommended continuing dietary treatment beyond 6 years due to the presence of deterioration in performance, hyperactivity, and seizures.12,13Gender was also considered a reason to continue treatment; specifically, the continued treatment of females for prevention of maternal PKU syndrome14, which causes microcephaly, intrauterine growth retardation, congenital heart disease, and neurocognitive impairment in the offspring of women with PKU who have uncontrolled Phe levels during pregnancy.15,16
As early as 1967, it was noted that exposure to elevated blood Phe was associated with declining intelligence quotient.16,17,18,19 Despite this, a 1980 survey of clinicians treating children with PKU indicated that some clinics allowed the diet to be “liberalized” as children aged. Even the two largest clinics in the United States reported discontinuing diet for all patients at 3 and 5–6 years of age without any intention to change their practice.20 During this period, three national collaborative studies were under way to compare the effects of continuing versus discontinuing dietary therapy. Accumulating evidence during this time led many clinicians to continue diet treatment while awaiting the outcome of these larger studies and the emergence of a consensus on the care of these patients. For example, one of the authors (S.C.), who was not part of any formal study, saw his first patient with PKU in 1971 and never recommended discontinuing diet, although a number of his patients elected to stop dietary restriction independent of medical advice.
In 1991, the National PKU Collaborative Study reported on the first cohort of 12-year-old children diagnosed through NBS. Patients randomized to discontinue diet at 6 years of age were found to have reduced cognitive functioning when compared with those who had remained on diet, reinforcing the association between high Phe concentrations and impaired cognitive function.21 In 1998, many patients who participated in this study as children were reassessed as adults to evaluate the long-term effects of dietary discontinuation into adulthood. This study revealed that the adults who did not discontinue diet obtained higher scores on measures of verbal intelligence and full-scale intelligence quotient scores than those who discontinued diet. In addition, those who discontinued diet were found to have high incidence of recurrent headaches (31%), neurological abnormalities (24%), hyperactivity (14%), and lethargy (19%), whereas none of these problems were reported by those who continued diet. Mental problems such as phobias and depression were also more frequently reported in those who discontinued versus those who continued diet.22
In response to the growing data on the effects of dietary discontinuation and lack of consistent management of PKU, the National Institutes of Health (NIH) convened a conference in 2000 to develop the first treatment guidelines for PKU.23 Recommendations included lifetime adherence to the Phe-restricted diet with maintenance of blood Phe levels between 120 and 360 µmol/l from infancy to 12 years of age, between 120 and 600 µmol/l during adolescence, and between 120 and 900 µmol/l into adulthood. The guidelines recommended that any woman planning pregnancy resume treatment before conception to achieve Phe levels of 120–360 µmol/l and maintain these levels throughout pregnancy to reduce the risk of effects of elevated blood Phe levels on the fetus. Monitoring recommendations included measuring blood Phe levels one to two times weekly for the first year of life, twice monthly from 1 to 12 years, monthly after 12 years, and twice weekly during pregnancy.23 These treatment guidelines provided much needed information to improve the standard of care for individuals with PKU. However, at that time, outcome data on adult patients treated from birth, but before the implementation of treatment for life, was not available.
Now, 50 years after the implementation of screening for PKU, a cohort of adults with PKU who were treated from birth provides valuable information about long-term treatment effects for inborn errors of metabolism in general and PKU specifically. We know that individuals with PKU fare best with treatment for life to maintain Phe levels within the recommended range.24 We are also aware that despite this, neurocognitive impairments such as poorer executive function skills and psychiatric problems are frequently reported even in early and continuously treated individuals with PKU.24
With these frequent reports of suboptimal outcomes in the literature,24 and the advent of new treatment options for PKU such as sapropterin dihydrochloride (sapropterin, Kuvan), large neutral amino acid supplementation, and glycomacropeptide foods, the NIH reconvened an expert group in 2012 to assess the current state of PKU treatment. This conference was a forum for review of data recently generated from the Agency for Health Research Quality on the state of PKU treatment in the United States. The report supports lifetime maintenance of blood Phe levels of 120–360 µmol/l and the association between long-term high Phe levels and development of neurocognitive impairment and psychological disturbances.25 The NIH conference also supported the need to update the 2000 NIH PKU treatment recommendations. Questions specifically applicable to PKU but also relevant to the more than 30 disorders detected by NBS arose during the conference: Are individuals with PKU accessing appropriate treatment to manage their PKU? What factors influence the individual with PKU to access treatment?
While a group of members from the American College of Medical Genetics and Genomics and Genetic Metabolic Dietitians International update the NIH treatment guidelines for PKU, we attempt to address these questions from the perspective of the US health-care system, looking specifically at the question of access to the health-care services required throughout life to treat PKU. We explore the long-term access to treatment for this patient population and identify areas that should be strengthened to continue improving treatment of individuals with PKU and provide potential insights into the future management of other diseases now identified through NBS programs.
Methods
To determine whether adults are accessing treatment for their PKU, an estimated number of adults with PKU was calculated for comparison with the number of adults with PKU who are actively followed by metabolic clinics. Data on number of births and those diagnosed by NBS programs with hyperphenylalaninemia (≥120 µmol/l) and classic PKU (>1,200 µmol/l) are available from the National Newborn Screening and Genetics Resource Center. An analysis of the National Newborn Screening and Genetics Resource Center records from 1996 to 2005 was performed to derive a combined composite incidence rate for hyperphenylalaninemia and classic PKU. Because classifications vary by clinic, incidence rates for hyperphenylalaninemia and classic PKU were combined and will be referred to as “PKU” throughout. The number of patients with PKU born each year from 1996 to 2005 was tabulated, and the sum of these figures provided a cumulative incidence rate to be used as a model for estimating the number of patients diagnosed with PKU in the United States. The results obtained using the cumulative incidence model were then compared against those reported in the literature.
The incidence rate of PKU calculated from the National Newborn Screening and Genetics Resource Center records for the decade 1996–2005 was applied to the annual number of births in the United States, as recorded in the National Vital Statistics System of the Centers for Disease Control and Prevention through 2010. Patients born before the initiation of NBS in 1965 in the United States were not included in the analysis. The calculated prevalence was then applied to the US Census Current Population Survey from the calendar year 2010 to estimate the number of individuals with PKU by age cohort.
BioMarin Pharmaceutical has developed and maintained a database of 137 metabolic clinics known to be following patients with PKU throughout the United States. During routine and ongoing visits, BioMarin collected the number of patients actively followed by each metabolic clinic in the database. For this analysis, collected data were distributed by age groups of 0–4 years, 5–12 years, 13–18 years, 19–24 years, 25–45 years and ≥46 years. Data not distributed by patient age in the database were analyzed and allocated into age groups using the aggregate percentages reported by clinics that provided data distributed by age. The number of PKU patients estimated from US birth data was compared with the number of patients with PKU reported by metabolic clinics as being treated in order to estimate the number of individuals with PKU who are not followed by a metabolic program.
Finally, online searches of government and private websites were performed to identify insurance coverage of medical formula and special low-protein foods by state and to assess the impact of insurance coverage on adult patients continuing to seek treatment. Authors also offered input from their experience regarding factors reported by patients and their families as well as issues encountered in the clinic.
Results
Table 1 includes tabulation of the annual number of patients with PKU and the calculated incidence of PKU for the 10-year period 1996–2005. The results of the incidence model are consistent with reported prevalence of PKU, which vary from 1:11,400 live births in the United States26 to 1:15,000.23 Therefore, an average incidence of 1:12,707 was applied to annual births reported to the National Vital Statistics System of the Centers for Disease Control and Prevention, resulting in an estimate of 14,988 individuals with PKU diagnosed from 1965 to 2010. Comparing this analysis with clinic reports, >50% of all individuals with PKU are not being followed by a metabolic clinic. The percentage increases with age, ranging from 19% of individuals in the 0–4 years group to >70% of individuals in the 19–45 years group ( Table 2 ).
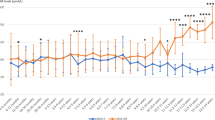
Data collected for state-based insurance coverage and access to care for adults with PKU reveal that eight states (15.4%) have coverage for medical formula only, whereas 18 (34.6%) have no coverage for treatment for adult patients, yielding a total of 50% of states that provide either no coverage of medical formula and modified special low-protein products or only partial coverage of these front-line medical food therapies required for the treatment of adults with PKU ( Table 3 ) The experience of the authors reinforces the difficulties patients experience accessing insurance as well other factors, which are further supported by reports in the literature ( Figure 1 ).
Factors identified as affecting access to treatment for phenylketonuria with applicability to other patients diagnosed through newborn screening.76
Discussion
Given that there are more than 30 metabolic and genetic disorders now diagnosed by NBS programs, we must consider the experience with PKU as an important model to establish the context for long-term treatment from universal NBS programs. Data collected through government statistics and industry suggest that an estimated 71% of adults with PKU between the ages of 19 and 45 years who were diagnosed by NBS are not actively treated by a metabolic clinic ( Table 2 ). Although these data are consistent with those reported in the literature,27 there is the possibility of a sampling error in the number of adults reported as being seen in clinic because data were collected by interview with clinic personnel conducted by representatives of BioMarin, the pharmaceutical company that markets sapropterin. There is also the potential that some adult patients are being treated by physicians not associated with metabolic clinics and therefore not included in this total. Moreover, the estimate that 19% of 0- to 4-year-old children with PKU are not followed by a clinic suggests that some of these patients may have a variant form of hyperphenylalanemia that is not considered to require therapy and, as such, a similar percentage of adults may also not need diet therapy. Regardless, this is a sobering statistic that emphasizes the need to address barriers to access to medical care in an effort to prevent similar issues from arising with other chronic diseases identified through NBS and to improve the outcomes for a greater majority of individuals with PKU.
Despite an increase in health and neuropsychiatric issues affecting adults with poor metabolic control, these concerns are rarely lethal, and those with PKU typically have a normal life span regardless of treatment status. Therefore, disparity between prevalence of PKU based on health statistics and the number of adults reported by metabolic clinics is not primarily due to morbidity in the patient population.28 This disparity may, in part, be due to the dramatic changes in treatment recommendations and clinical guidelines over time. Previous recommendations for early discontinuation of treatment likely resulted in the loss to follow-up of many adults with PKU. Because many metabolic clinics report that they do not see adult patients27,29,30 ( Table 2 ) and some clinics associated with children’s hospitals are not allowed to see adults, the vast majority of adults with PKU are not being followed by a metabolic clinic and encounter difficulties locating clinics able to accept new adult patients with PKU.27 Such was the case in 2008–2009 when the author J.K. helped a veteran find a clinic when he was unable to be treated at Children’s Hospital of Los Angeles because his metabolic physician was not permitted to treat adult patients.
In addition to the inability to access a metabolic clinic, results of the current study clearly identify a lack of or limited insurance coverage for required medical food therapy as a significant and primary barrier for the treatment of adults with PKU31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71 ( Table 3 ). Only 50% of the states in the United States provide coverage of both required medical food and modified special low-protein food products, and almost 35% do not provide any coverage for these therapies for adults with PKU.31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71 Even for those states that do have mandated coverage, barriers to access to medical formula and low-protein special foods may exist for the patient from employer self-insured plans, which do not have to comply with state-imposed mandates. We do not know whether a causal relationship exists between third-party health insurance coverage and access to clinics; however, the contribution of this factor is supported by the literature,27,72,73,74,75 as well as by our own experience.
In far too many states without mandates, private health insurance may cover prescribed pharmaceutical treatments such as sapropterin but not the cost of medical formula and special low-protein foods that are also required to maintain Phe levels within the recommended treatment range, even with sapropterin administration. For those without coverage, the expense associated with medical foods and special low-protein foods27,30 or insurance copayments may be prohibitive for many patients.27,74,75,76 For those with coverage, the deductible is often too high to be met by the patient. Author K.M. reports one patient who benefits from sapropterin treatment and has a small monthly copayment for this medication through his pharmacy benefit. However, as he cannot afford the deductible for the medical food products required to keep blood Phe levels within treatment range, he has access to neither medically necessary treatment for his PKU despite the small monthly copayment for sapropterin.
Ironically, as Medicaid covers the cost of medical foods in all states ( Table 3 ), those individuals with the greatest neurocognitive impairments who are unemployed or underemployed may be better able financially to access treatment compared with employed individuals without the benefits of adequate insurance for the coverage of medical foods. However, individuals with neurocognitive impairments may not be aware of the details of Medicaid coverage or may be unable to independently complete the paperwork required to receive coverage from Medicaid. For those in group homes, care providers assist in completing forms and securing assistance from regional centers. Those who are not referred to social workers must rely on their clinic to assist with paperwork. The time required to complete paperwork, including not only completion of applications but also accessing required documents and supplementary materials, is often prohibitive, and there can be significant lapses for some patients before obtaining treatment for their PKU. This may be the case even for those who are pregnant, when high Phe levels may result in maternal PKU syndrome for the fetus.
A variety of other factors have also been identified as affecting adult patients’ ability to access appropriate treatment for PKU ( Figure 1 ).27,28,29,30,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98 Psychiatric and executive function impairments such as attention and processing-speed deficits,73,77,80 behavioral and emotional problems,81 psychiatric disorders,73,81 and cognitive deficits73,81,82,83 may have an overall negative effect on the individual’s quality of life. If an adult is not followed by a metabolic clinic, he or she may not know that diet treatment is now recommended for life or that new treatment options are available that may make adherence more attainable. The resulting neurocognitive deficits may contribute to unemployment or underemployment, with the subsequent socioeconomic barriers to treatment and difficulty navigating the insurance system to secure access to treatment.84 Even for those adults who continue treatment, there remains a higher risk than the general population for neurocognitive and psychological deficits associated with elevated and/or fluctuating Phe levels.23,24 The less severe neurocognitive issues may still result in patients having difficulties with daily living, such as scheduling and keeping medical appointments.27,72,83 Moreover, because the majority of metabolic clinics have limited access to mental health-care professionals and encounter difficulties obtaining authorization for psychological evaluations, adult patients with neurocognitive and psychological impairment may have limited access to health-care professionals suitably prepared to treat them.
Familial,84,85,88,89,90 social,27,91,92 and health-care provider support systems27,30,85 are important to assist individuals with pursuing treatment for PKU.85,86,87 Distance to the metabolic clinic, lack of transportation, and inability to get time off work have also been cited as reasons for not accessing treatment.27,88 These barriers are not isolated to the American health-care system85,93,94 or unique to PKU.95,96 Similar barriers have been identified in other chronic diseases lacking episodes of acute illness requiring immediate medical attention, such as diabetes, asthma, and other inborn errors of metabolism.95,96
Since the NIH guidelines in 2000 recommended treatment for life,23 transitional care has become an important aspect of managing individuals with PKU and an important concern for many metabolic clinics.76,92,97 Some metabolic clinics have initiated adult-focused clinics to transition patients from pediatric to adult care. However, patient response to transition varies; some patients report feeling uncomfortable at pediatric clinics, whereas others are uncomfortable transitioning from clinics where they have been followed since childhood. Educating caregivers72,84,85 as well as individuals with PKU27 can help prepare them for transition to adult care, an important focus for successful lifelong management of PKU.25,27,72,85,98
Although early treatment of PKU after NBS has been appropriately hailed a success story, it should also be considered a cautionary tale of the success of NBS coupled with the resulting issues of lifelong chronic disease management. While there is a near-universal diagnosis of PKU in the United States, the goal of access to culturally sensitive, age-appropriate treatment programs remains elusive. The majority of adults with PKU are not accessing treatment despite the 2000 NIH recommendation of lifelong diet treatment and the growing evidence of the positive results of resuming treatment for those adults who have not been maintaining metabolic control.27,83
Significant barriers to treatment access are societal, institutional, and multifaceted, starting with the structure of the health-care delivery system and attitudes toward adults with neurocognitive and other disabilities, and ending with logistical, socioeconomic, and insurance coverage issues. Although we cannot with certainty say what has happened to the significant number of PKU patients identified through NBS who are not being followed by a metabolic clinic and are not in contact with patient support organizations, we can say with confidence that outcomes are likely to be significantly poorer for those who are not treated and followed regularly by a metabolic clinic.
Updated treatment recommendations must advise metabolic clinics on how to be prepared for the schism between the treatment needs of adult patients who have been treated early and continuously, and those treated before the “treatment for life” paradigm was implemented. We must also continue to advocate for access to appropriate mental health-care and clinic support for all adult patients with PKU, and not just those who have maintained ongoing contact with pediatric clinics. However, as shown by data from this study, insurance coverage issues persist for many patients, meaning that adults with PKU may go for extended periods of time without access to medical and special low-protein food products. Even for those adults with insurance, one-third of states in the United States (34.6%) may still not have mandated insurance coverage for treatment of adults, and 15.4% of the states may continue to cover only medical formula and not the cost of special low-protein foods ( Table 3 ).
As the NIH, Genetic Metabolic Dietitians International, and the American College of Medical Genetics and Genomics prepare these updated treatment recommendations for PKU, we need to develop the means to implement the recommendations for all patients, not just a few. As a society, it is unethical and ineffective to diagnose a condition and then systematically deny treatment in a variety of ways. We need to improve long-term engagement with chronic-care patients identified through universal NBS programs to ensure optimal lifetime outcomes, and not just celebrate the amelioration of the most severe manifestations of disease.
Disclosure
Elaina Jurecki and Ruth Suter are employees and stockholders of BioMarin Pharmaceutical. The National PKU Alliance has received funding from Abbott Nutrition, Applied Nutrition, BioMarin Pharmaceutical, Cambrooke Foods, Mead Johnson, Nutricia, PKU Perspectives, Solace Nutrition, and Vitaflo. Jean Koch is a stockholder of BioMarin Pharmaceutical. Mitzie Grant has received funding from BioMarin Pharmaceutical for consultant services and clinical research. Judy Wiles has received funding from BioMarin Pharmaceutical for medical writing assistance. Stephen Cederbaum has received funding from BioMarin Pharmaceutical for consultant services.
References
Guthrie R, Susi A . A simple phenylalanine method for detecting phenylketonuria in large populations of newborn infants. Pediatrics 1963;32:338–343.
Folling A . The excretion of phenylpyruvic acid in the urine, an anomaly of metabolism in connection with imbecility. Zeitschrift fur PhysiologischeChemie 1934;227:169–176.
Scriver CR, Levy H, Donlon J . Hyperphenylalaninemia: phenylalanine hydroxylase deficiency. In: Valle D, Beaudet AL, Vogelstein B, Kinzler KW, Antonarakis SE, Ballabio A (eds). The online metabolic and molecular bases of inherited disease. 2008. http://www.ommbid.com.
Koch R, Dobson JC . Hospital screening programs aid identification of PKU. Hosp Top 1968;46:111–113.
Hansen H, Shahidi A, Stein ZA . Screening for phenylketonuria in New York City. Threshold values reconsidered. Public Health Rep 1978;93:246–251.
Hanley WB, Linsao L, Davidson W, Moes CA . Malnutrition with early treatment of phenylketonuria. Pediatr Res 1970;4:318–327.
Blaskovics ME, Nelson TL . Phenylketonuria and its variations. A review of recent developments. Calif Med 1971;115:42–57.
Berman JL, Cunningham GC, Day RW, Ford R, Hsia DY . Causes for high phenylalanine with normal tyrosine in newborn screening programs. Am J Dis Child 1969;117:54–65.
Peterson RM, Koch R, Schaeffler GE, Wohlers A, Acosta PB, Boyle D . Phenylketonuria. Experience at one center in the first year of screening in California. Calif Med 1968;108:350–354.
Fisch RO, Torres F, Gravem HJ, Greenwood CS, Anderson JA . Twelve years of clinical experience with phenylketonuria. A statistical evaluation of symptoms, growth, mental development, electroencephalographic records, serum phenylalanine levels, and results of dietary management. Neurology 1969;19:659–666.
Koff E, Kammerer B, Boyle P, Pueschel SM . Intelligence and phenylketonuria: effects of diet termination. J Pediatr 1979;94:534–537.
Murphy D . Termination of dietary treatment of phenylketonuria. Ir J Med Sci 1969;8:177–183.
Clayton BE, Moncrieff AA, Pampiglione G, Shepherd J . Biochemical and EEG studies in phenylketonuric children during phenylalanine tolerance testc. Arch Dis Child 1966;41:267–272.
McBean MS, Stephenson JB . Treatment of classical phenylketonuria. Arch Dis Child 1968;43:1–7.
Moseley KM, Skrabal J, Yano S, Koch R . Sapropterin dihydrochloride (6R-BH4) and maternal phenylketonuria two case studies. Infan Child Adoles Nutr 2009;5:262–266.
Lenke RR, Levy HL . Maternal phenylketonuria and hyperphenylalaninemia. An international survey of the outcome of untreated and treated pregnancies. N Engl J Med 1980;303:1202–1208.
Dobson J, Koch R, Meyers C, Spector R, Williamson, M . The relationship between cognitive development and dietary treatment in phenylketonuric children. Presented at the Conference of American Association of Mental Deficiency. May 1967.
Cabalska B, Duczynska N, Borzymowska J, Zorska K, Koslacz-Folga A, Bozkowa K . Termination of dietary treatment in phenylketonuria. Eur J Pediatr 1977;126:253–262.
Smith I, Lobascher ME, Stevenson JE, et al. Effect of stopping low-phenylalanine diet on intellectual progress of children with phenylketonuria. Br Med J 1978;2:723–726.
Schuett VE, Gurda RF, Brown ES . Diet discontinuation policies and practices of PKU clinics in the United States. Am J Public Health 1980;70:498–503.
Azen CG, Koch R, Friedman EG, et al. Intellectual development in 12-year-old children treated for phenylketonuria. Am J Dis Child 1991;145:35–39.
Koch R, Burton B, Hoganson G, et al. Phenylketonuria in adulthood: a collaborative study. J Inherit Metab Dis 2002;25:333–346.
National Institutes of Health Consensus Development Panel. National Institutes of Health Consensus Development Conference Statement. Phenylketonuria (PKU): acreening and management, October 16–18, 2000. Pediatr 2001;108:972–982.
Enns GM, Koch R, Brumm V, Blakely E, Suter R, Jurecki E . Suboptimal outcomes in patients with PKU treated early with diet alone: revisiting the evidence. Mol Genet Metab 2010;101:99–109.
Agency for Healthcare Research and Quality (AHRQ). Adjuvant Treatment for Phenylketonuria (PKU). Comparative Effectiveness Review 56. http://effectivehealthcare.ahrq.gov/ehc/products/259/957/executivesummary_CER56_PKU.pdf. Accessed 12 September 2012.
Hertzberg VS, Hinton CF, Therrell BL, Shapira SK . Birth prevalence rates of newborn screening disorders in relation to screening practices in the United States. J Pediatr 2011;159:555–560.
Burton BK, Leviton L . Reaching out to the lost generation of adults with early-treated phenylketonuria (PKU). Mol Genet Metab 2010;101:146–148.
Pitt DB, Danks DM . The natural history of untreated phenylketonuria over 20 years. J Paediatr Child Health 1991;27:189–190.
Bilginsoy C, Waitzman N, Leonard CO, Ernst SL . Living with phenylketonuria: perspectives of patients and their families. J Inherit Metab Dis 2005;28:639–649.
National PKU Alliance. http://www.npkua.org/index.php/clinics. Accessed 7 August 2012.
The Alaska State Legislature. http://w3.legis.state.ak.us/index.php. Accessed 10 February 2012.
onecle. http://law.onecle.com/arizona/insurance/20-2326.html. Accessed 10 February 2012.
Arkansas State Insurance. http://www.insurance.arkansas.gov/PandC/Insurance%20Code%20&%20related%20chapters/Chapter79.htm. Accessed 10 February 2012.
onecle. http://law.onecle.com/california/insurance/10123.89.html. Accessed 10 February 2012.
LexisNexis. http://www.lexisnexis.com/hottopics/Colorado/. Accessed 6 January 2012.
State of Connecticut General Assembly. http://search.cga.state.ct.us/adv/. Accessed 10 February 2012.
Find Law. http://codes.lp.findlaw.com/decode/18/33/3355. Accessed 6 January 2012.
District of Columbia Official Code. http://weblinks.westlaw.com/find/default.wl?cite=N5F33100095-DB11DB9BCF9-DAC28345A2A&sr=TC&pbc=DA010192&rs=WEBL13.01&rp=%2ffind%2fdefault.wl&spa=DCC-1000&fn=_top&findtype=VQ&vr=2.0&db=1000869. Accessed 22 February 2013.
The Florida Senate. http://www.flsenate.gov/Laws/Statutes/2011/627.42395. Accessed 6 January 2012.
Hawaii State Legislature. http://www.capitol.hawaii.gov/hrscurrent/Vol09_Ch0431-0435E/HRS0431/HRS_0431-.htm. 22 February 2013.
IDAPA 16.02.26. Rules Governing the Idaho Children’s Special Health Program.
Leagle. http://www.leagle.com/statutes.aspx?page=5&xmldoc=ILST08292011081.xml&docbase=Statutes&SizeDisp=7. Accessed 6 January 2012.
Indiana State Legislative Agency. http://www.in.gov/legislative/ic/code/title27/ar8/ch24.1.html. Accessed 6 January 2012.
Kansas Statutes. http://kansasstatutes.lesterama.org/Chapter_65/Article_1/65-180.html. Accessed 6 January 2012.
Kentucky Legislature. http://www.lrc.ky.gov/kar/902/004/035.htm. Accessed 6 January 2012.
Louisiana State Legislature. http://legis.la.gov/lss/lss.asp?doc=506420. Accessed 6 January 2012.
Maine Revised Legislature. http://www.mainelegislature.org/legis/statutes/24-a/title24-Asec2745-D.html. Accessed 6 January 2012.
Find Legal Information. http://www.find-laws.com/statutes/maryland/health-general/title-19/subtitle-7/19-705-5. Accessed 6 January 2012.
Commonwealth of Massachusetts. http://www.malegislature.gov/Laws/GeneralLaws/PartI/TitleXXII/Chapter176b/Section4k. Accessed 6 January 2012.
Minnesota Office of the Revisor of Statutes. https://www.revisor.leg.state.mn.us/statutes/?id=256B.0625&year=2011. Accessed 6 January 2012.
Missouri Revised Statutes. http://www.moga.mo.gov/statutes/C300-399/3760001219.HTM. Accessed 6 January 2012.
Montana Code Annotated 2011. http://data.opi.mt.gov/bills/mca/33/22/33-22-131.htm. Accessed 6 January 2012.
Law Server. http://www.lawserver.com/law/state/nebraska/ne-statutes/nebraska_statutes_71-520. Accessed 6 January 2012.
Nevada Legislature. http://www.leg.state.nv.us/nrs/NRS-689A.html#NRS689ASec0423. Accessed 6 January 2012.
Justia US Law. http://law.justia.com/codes/new-hampshire/2010/titlexxxvii/chapter420-a/section420-a-17/. Accessed 6 January 2012.
onecle. http://law.onecle.com/new-jersey/17-corporations-and-institutions-for-finance-and-insurance/48a-7q.htm. Accessed 12 September 2012.
New Mexico Compilation Commission. http://www.nmonesource.com/nmnxtadmin/. Accessed 10 October 2012.
New York Legislator. http://public.leginfo.state.ny.us/menuf.cgi. Accessed 12 September 2012.
onecle. http://law.onecle.com/north-carolina/130a-public-health/130a-125.html. Accessed 6 January 2012.
North Dakota Legislative Branch. http://www.legis.nd.gov/cencode/t25c17.pdf. Accessed 15 October 2012.
State of Oklahoma. http://webserver1.lsb.state.ok.us/2003-04HB/HCR1044_int.rtf. Accessed 15 October 2012.
Oregon Laws. http://www.oregonlaws.org/ors/743A.188. Accessed 6 January 2012.
http://weblinks.westlaw.com/find/default.wl?cite=N901E570034-2611DA8A989-F4EECDB8638&sr=TC&pbc=DA010192&rs=WEBL13.01&rp=%2ffind%2fdefault.wl&spa=PAC-1000&fn=_top&findtype=VQ&vr=2.0&db=1000262. Accessed 22 February 2013.
State of Rhode Island General Assembly. http://webserver.rilin.state.ri.us/Statutes/. Accessed 15 October 2012.
South Dakota Legislature. http://legis.state.sd.us/statutes/DisplayStatute.aspx?Type=Statute&Statute=58-38-23. Accessed 6 January 2012.
Find Legal Information. http://www.find-laws.com/statutes/tennessee/title-56/chapter-7/part-25/56-7-2505. Accessed 6 January 2012.
FindLaw. http://codes.lp.findlaw.com/txstatutes/IN/8/E/1359/1359.003. Accessed 6 January 2012.
Utah State Legislature. http://le.utah.gov/~code/TITLE31A/htm/31A22_062300.htm. Accessed 6 January 2012.
Vermont Statutes Online. http://www.leg.state.vt.us/statutes/fullsection.cfm?Title=08&Chapter=107&Section=04089e. Accessed 6 January 2012.
Washington State Legislature. http://apps.leg.wa.gov/rcw/default.aspx?cite=48.20.520. Accessed 6 January 2012.
State of Wisconsin. http://docs.legis.wisconsin.gov/statutes/statutes/253.pdf. Accessed 15 October 2012.
Koch R, Trefz F, Waisbren S . Psychosocial issues and outcomes in maternal PKU. Mol Genet Metab 2010;99(suppl 1):S68–S74.
Brumm VL, Azen C, Moats RA, et al. Neuropsychological outcome of subjects participating in the PKU adult collaborative study: a preliminary review. J Inherit Metab Dis 2004;27:549–566.
Barron J, Wahl P, Fisher M, Plauschinat C . Effect of prescription copayments on adherence and treatment failure with oral antidiabetic medications. P T 2008;33:532–553.
Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health 2008;11:44–47.
Camp KM, Lloyd-Puryear MA, Huntington KL . Nutritional treatment for inborn errors of metabolism: indications, regulations, and availability of medical foods and dietary supplements using phenylketonuria as an example. Mol Genet Metab 2012;107:3–9.
Albrecht J, Garbade SF, Burgard P . Neuropsychological speed tests and blood phenylalanine levels in patients with phenylketonuria: a meta-analysis. Neurosci Biobehav Rev 2009;33:414–421.
Huijbregts SC, de Sonneville LM, Licht R, van Spronsen FJ, Verkerk PH, Sergeant JA . Sustained attention and inhibition of cognitive interference in treated phenylketonuria: associations with concurrent and lifetime phenylalanine concentrations. Neuropsychologia 2002;40:7–15.
Channon S, Mockler C, Lee P . Executive functioning and speed of processing in phenylketonuria. Neuropsychology 2005;19:679–686.
Christ SE, Steiner RD, Grange DK, Abrams RA, White DA . Inhibitory control in children with phenylketonuria. Dev Neuropsychol 2006;30:845–864.
Brumm VL, Bilder D, Waisbren SE . Psychiatric symptoms and disorders in phenylketonuria. Mol Genet Metab 2010;99(suppl 1):S59–S63.
Waisbren SE, Noel K, Fahrbach K, et al. Phenylalanine blood levels and clinical outcomes in phenylketonuria: a systematic literature review and meta-analysis. Mol Genet Metab 2007;92:63–70.
Vernon HJ, Koerner CB, Johnson MR, Bergner A, Hamosh A . Introduction of sapropterin dihydrochloride as standard of care in patients with phenylketonuria. Mol Genet Metab 2010;100:229–233.
Cotugno G, Nicolò R, Cappelletti S, Goffredo BM, Dionisi Vici C, Di Ciommo V . Adherence to diet and quality of life in patients with phenylketonuria. Acta Paediatr 2011;100:1144–1149.
Stockler S, Moeslinger D, Herle M, Wimmer B, Ipsiroglu OS . Cultural aspects in the management of inborn errors of metabolism. J Inherit Metab Dis 2012. doi:10.1007/s10545-012-9455-4
Feillet F, MacDonald A, Hartung Perron D, Burton B . Outcomes beyond phenylalanine: an international perspective. Mol Genet Metab 2010;99(suppl 1):S79–S85.
World Health Organization (WHO). Adherence to long-term therapies: evidence for action. http://whqlibdoc.who.int/publications/2003/9241545992.pdf. Accessed 12 September 2012.
Imperiale M, Suter R, Jurecki E, Schelling C, Turbeville S . Factors which may lead to inappropriate discontinuation of Kuvan® after at least 3 months of continued therapy. Presented in 2009 at the annual International Congress of Inborn Errors of Metabolism.San Diego, CA, USA, 29 August 2009 – 2 September 2009.
Olsson GM, Montgomery SM, Alm J . Family conditions and dietary control in phenylketonuria. J Inherit Metab Dis 2007;30:708–715.
Fehrenback AM, Peterson J . Parental problem-solving skills, stress, and dietary compliance in phenylketonuria. J Consult Clin Psychol 1989;57:237–241.
Scal P, Evans T, Blozis S, Okinow N, Blum R . Trends in transition from pediatric to adult health care services for young adults with chronic conditions. J Adolesc Health 1999;24:259–264.
Mütze U, Roth A, Weigel JF, et al. Transition of young adults with phenylketonuria from pediatric to adult care. J Inherit Metab Dis 2011;34:701–709.
MacDonald A, Gokmen-Ozel H, van Rijn M, Burgard P . The reality of dietary compliance in the management of phenylketonuria. J Inherit Metab Dis 2010;33:665–670.
Ozel HG, Kucukkasap T, Koksal G, et al. Does maternal knowledge impact blood phenylalanine concentration in Turkish children with phenylketonuria? J Inherit Metab Dis 2008;31(suppl 2):S213–S217.
van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW . Prevalence and characteristics of children with special health care needs. Arch PediatrAdolesc Med 2004;158:884–890.
Kemper AR, Brewer CA, Singh RH . Perspectives on dietary adherence among women with inborn errors of metabolism. J Am Diet Assoc 2010;110:247–252.
American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group; Cooley WC, Sagerman PJ . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatr 2011;128:182–200.
Tiv M, Viel JF, Mauny F, et al. Medication adherence in type 2 diabetes: the ENTRED study 2007, a French Population-Based Study. PLoS ONE 2012;7:e32412.
American College of Medical Genetics as commissioned by the Health Resources and Services Administration (HRSA). Newborn screening: towards a uniform screening panel and system. Genetic Med 2006;8(suppl 5):S12–S252.
Acknowledgements
Beth Rader provided assistance with data collection and analysis. Medical writing, editorial, and layout assistance was supported with funds from BioMarin Pharmaceutical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Berry, S., Brown, C., Grant, M. et al. Newborn screening 50 years later: access issues faced by adults with PKU. Genet Med 15, 591–599 (2013). https://doi.org/10.1038/gim.2013.10
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2013.10
Keywords
This article is cited by
-
Measuring Burden of Illness in Phenylketonuria (PKU): Development of the PKU Symptom Severity and Impacts Scale as a Robust Patient-Reported Outcome
Advances in Therapy (2022)
-
Preventing maternal phenylketonuria (PKU) syndrome: important factors to achieve good metabolic control throughout pregnancy
Orphanet Journal of Rare Diseases (2021)
-
The effect of improved dietary control on cognitive and psychiatric functioning in adults with phenylketonuria: the ReDAPT study
Orphanet Journal of Rare Diseases (2021)
-
Adult cognitive outcomes in phenylketonuria: explaining causes of variability beyond average Phe levels
Orphanet Journal of Rare Diseases (2019)
-
A systematic review of cognitive functioning in early treated adults with phenylketonuria
Orphanet Journal of Rare Diseases (2018)