Abstract
Purpose: Genetic cancer risk assessment is an emerging interdisciplinary practice that requires knowledge of genetics and oncology and specialized patient and family counseling skills. There is a growing need for cancer risk assessment practitioners, but most clinicians have inadequate cross-disciplinary training. An interdisciplinary course was developed to promote practitioner-level competency in cancer risk assessment to community-based clinicians.
Methods: Participants were competitively selected from a pool of board-certified/eligible genetic counseling, masters-trained advanced practice nursing and physician applicants. Preference was given to clinicians with strong institutional backing practicing in underserved regions. The Continuing Medical Education/Continuing Education Unit-accredited course included didactic lectures, workshops, counseling practicum, and case conferences. Pre- and postcourse knowledge tests measured cancer genetics knowledge. Six month and one-year postcourse practice outcome surveys measured the impact of the program on professional self-efficacy and continued professional development.
Results/Conclusions: Forty clinicians completed the course (23 genetic counselors, 14 nurses, and three physicians). There was a significant overall increase of 22.6% in postcourse knowledge scores (P < 0.001). Thirty-five (88%) completed prescribed practice development activities. Of 29 respondents to 1-year postcourse survey, 76% reported increased professional self-efficacy; 66% reported increase in number of patients seen, and virtually all indicated interest in additional training. Outcomes demonstrate the value and efficacy of interdisciplinary training in genetic cancer risk assessment targeted to motivated community-based clinicians. Courses such as this can help address the need for competent cancer risk assessment services in communities outside the academic health center.
Similar content being viewed by others
Main
The rapid pace of genetic discovery continues to drive changes in clinical care, bringing greater understanding of the genetic basis of cancer and more incisive tools for hereditary cancer risk assessment. While only 5% to 10% of cancers are associated with highly penetrant hereditary syndromes, this translates to hundreds of thousands of cancer cases attributable to hereditary predisposition, and the magnitude of risk conferred by these altered genes is dramatic. Identifying those at increased risk allows for more effective application of surveillance or preventive measures and may improve the quality of life for individuals at risk.1–7
There are now more than 50 hereditary cancer-associated syndromes for which the genetic basis is known, and new genes are reported every year. Genetic cancer risk assessment is standard of care for several of these, including familial adenomatous polyposis, multiple endocrine neoplasia Types I and II, Von Hipple Lindau disease, hereditary breast/ovarian cancer syndrome, and hereditary nonpolyposis colorectal cancer syndrome.8–14
The genetic cancer risk assessment process is complex, involving more steps and provider time than most other clinical services, and has emerged as a highly specialized discipline that requires knowledge of genetics, oncology, and individual and family counseling skills.15–19 There is a growing need for clinicians with the cross-training required for efficient identification and management of high-risk individuals.20–27
Genetic counselors have formal education in genetics and are trained to address the complex communications and counseling issues related to prenatal and pediatric genetics, but little or no training in oncology.17 Formal education for genetics nurses has historically been focused on prenatal or pediatric genetics.28 Conversely, advanced practice oncology nurse training is typically centered on the care and supportive management of individuals with active diagnoses of cancer, with little or no formal training in genetics or genetic counseling.29 Medical oncologists are well trained in most aspects of cancer screening, diagnosis, and management of individuals with cancer, but there is inadequate training in genetics in medical school, and medical geneticists generally have minimal training in oncology and the clinical aspects of cancer.30,31
Oncology and genetics professional societies and the National Cancer Institute (NCI) have advocated greater educational opportunities in the emerging discipline of cancer genetics.8,14 (NIH Publication No. 98-4373, pp 31–87) The American Society of Human Genetics (ASHG), National Society of Genetic Counselors (NSGC), American Society of Clinical Oncologists (ASCO), the International Society of Nurses in Genetics (ISONG), and a small number of academic institutions have conducted 1- to 2-day cancer genetics seminars, but there are few formal cancer genetics training opportunities available for clinicians to develop the interdisciplinary skills that contribute to practitioner-level competence. Consequently, most active cancer risk practitioners have developed their clinical expertise primarily through on-the-job experience.32
To address the growing need for interdisciplinary training in cancer risk assessment, the Cancer Genetics Education Program (CGEP) of the Department of Clinical Cancer Genetics (CCG) at the City of Hope Comprehensive Cancer Center developed and delivered an intensive course in clinical cancer genetics, supported by the California Cancer Research Program of the University of California no. 99-86874. The goal of the course was to promote practitioner-level competency in cancer risk assessment for clinicians, focusing on genetic counselors (GCs) and master's level advanced practice nurses (APNs) specializing in oncology or genetics. Although not marketed directly to physicians (MDs), participation was also open to MDs with oncology or genetics training. This article describes the outcomes of the first 3 years of delivery of the course on cancer genetics knowledge and its impact on practice among course participants.
MATERIALS AND METHODS
Curriculum development
The Intensive Course curriculum was developed by a multidisciplinary team composed of Clinical Cancer Genetics (CCG), Nursing Research Education, and other Cancer Center faculty, working from a core curriculum developed by the CCG Cancer Genetics Education Program (CGEP) for primary care and specialty clinicians. The core CGEP curriculum, supported in part by an NCI cancer education research grant (R25 CA75131, J. Weitzel, PI), incorporates key elements of the published ASCO cancer genetics curriculum,33 periodic scientific meeting proceedings, and clinical experience from the City of Hope Cancer Screening and Prevention Program (comprehensive clinical cancer genetics services network). The CGEP conducts grand rounds CME lectures and an annual full-day cancer genetics conference targeted to community physicians and allied health professionals. A description of the CGEP curriculum development and program implementation, and a report describing the effects of the first of the first 5 years of CGEP outreach on clinician knowledge about cancer genetics and referral of high-risk patients have been published.34,35 The CGEP also provides the infrastructure for clinical cancer genetics internships and an NCI-funded career development program in cancer genetics research.
The CGEP director is an MD who is board-certified in both medical oncology and clinical genetics, with 15 years of program leadership experience in clinical and research cancer genetics. The course was codirected by an American Board of Genetic Counseling (ABGC)–certified GC and APN with specialty certification in genetics (APNG),28 both of whom have extensive experience in clinical cancer genetics and cancer genetics education and training.
The overall intensive course objectives are listed in Table 1. The core CGEP curriculum was expanded for the intensive course to include lectures by Cancer Center and extramural faculty with expertise on topics required for cross-disciplinary cancer genetics training (surgical and medical oncology, molecular genetics, cytogenetics, molecular medicine, biostatistics, epidemiology, bioethics, law, and quality-of-life). Cross-disciplinary training among genetic counseling, nursing, and physician participants was fostered through case-based problem solving workshops, mock and practice cancer risk counseling sessions, attendance in established CME-accredited Clinical Cancer Genetics Working Group (multidisciplinary case review conference), Topics in Cancer Genetics (interdisciplinary literature review/journal club) sessions, and a molecular genetics wet lab. Each year an annual CGEP full-day cancer genetics conference for primary care and specialty physicians35 was incorporated into the intensive course curriculum to enhance and broaden course content and to encourage cross-disciplinary interaction during conference workshops and case presentations. Intensive course didactic modules, workshops, special training sessions, and titles of the full-day CGEP conferences included in each year's course are listed in Table 2.
The course was purposefully designed to simultaneously train clinicians from different disciplines (e.g., genetic counselors and oncology nurses) to encourage cross-disciplinary learning. Continuing medical education (CME) accreditation (70 hours) for APNs and MDs was obtained through the Cancer Center ACCME accreditation process; continuing education units (CEU) accreditation (5.6 units) was obtained from the American Counseling Association through the NSGC for GCs. A professional activities plan defining prescribed continued clinical, educational, teaching, and professional affiliation activities was provided to each participant to foster structured postcourse professional development. The postcourse activities included reading and summarizing a total of 15 seminal articles, each on a different topic area related to cancer genetics syndromes and behavioral, ethical, legal, and social issues related to cancer risk assessment; delivering one or more educational talks on cancer risk assessment to medical professionals within their institution or community, and attending one or more professional organizational seminar with content related to cancer genetics (ASHG, ASCO, NSGC, ISONG).
The course curriculum was reviewed by the interdisciplinary CGEP advisory committee, which is composed of professionals in genetics, oncology, social services, bioethics, law, and medical education. Revisions to the curriculum were made after each year's offering to incorporate suggestions and critiques from course participants and faculty.
Curriculum delivery
Lectures were delivered as PowerPoint presentations in 45-minute segments followed by 10- to 15-minute question and answer sessions. Mock counseling sessions were conducted with actual consultants (patients who've gone through the cancer risk assessment process who volunteered to participate in the course) under the supervision of senior cancer genetics counseling faculty. Participants reviewed and discussed actual anonymized clinical cases in the weekly Cancer Genetics Working Group. The Molecular Genetics Wet Lab took participants through a demonstration of molecular genetics sequencing and screening techniques with explanations on how to read results of molecular genetic analyses, followed by a hands-on workshop in DNA extraction and analysis. The weekly Topics in Cancer Genetics journal club allowed participants to experience a critical review of articles from the primary cancer genetics literature.
The course syllabus was composed of printed outlines of presentations and handouts for each didactic module, selected scientific articles, case-based assignments, compiled references and on-line resources, and a genetics and oncology glossary. All participants attended a computer lab for introduction to a computerized pedigree drawing and database program, and were instructed on the use of the Genetics Link, a pilot version of an internet web-based discussion board interface for postcourse practice development and case discussions. Web board features were developed and implemented progressively with each offering of the course, beginning with introduction to the discussion board for postcourse use in year 1, with the completion of pre- and postknowledge tests via the web board added in year 2, and PDF files of assigned journal articles were distributed via the web board in addition to the other activities in year 3.
Participant selection and profiles
The course design and participant evaluation protocol were approved by the City of Hope Institutional Review Board. Participants were competitively selected based on academic merit, demonstrated need for cancer risk assessment services in their community, and institutional support for implementing or expanding a clinical cancer genetics program. The course was primarily targeted and marketed to board-eligible or certified GCs and master's level APNs with oncology or genetics specialties, practicing in underserved geographic areas in California (in part because of the State of California–based funding mechanism), but physicians were also eligible, and enrollment was opened to clinicians practicing in areas outside of California on a space-available basis. California-based clinicians received a travel stipend and subsidized lodging through California Cancer Research Program support (University of California no. 99-86874). A modest fee was assessed for incidental costs. A total of 40 competitively selected clinicians completed the course over three annual offerings from 2001 to 2003; 23 ABGC board-certified or board-eligible GCs, 14 APNs (10 with oncology training and 4 with training in general genetics), and three MDs in clinical genetics practice. The professional profiles of the participants are summarized in Table 3. In addition, three APNs with specialty training in education attended the course to learn about the content and training methods. As their purpose for training was not associated with clinical practice, they did not complete all of the knowledge and practice surveys and they are not included in this analysis.
Instruments
Knowledge test
Knowledge changes were measured by pre- and postcourse tests composed of approximately 40 true/false and multiple choice questions selected from an 88-item test bank covering core concepts in cancer genetics and oncology, cancer syndrome recognition, cancer risk assessment, genetic testing strategy, and ethical, legal, and insurance issues. The questions were created by the course directors, CCG clinical staff, and course faculty. Faculty were not privy to the final 40 items selected for administration to a given class. Psychometric analyses of these questions were performed on the entire 88-question item bank. Initial analysis revealed that overall item difficulty index ranged from 0.07 (very difficult) to 1.0 (very easy). Coefficient alpha, a measure of internal consistency reliability, was 0.70 for a group of common test questions administered to all participants. Five questions that did not discriminate between high and low scorers (item-total correlations < 0.20) were removed from the test item bank. Selected questions were revised in hopes of improving discrimination and difficulty. Forty items representing each of the course topic domains were selected for each course offering and were administered to participants on site on day one of the course to obtain baseline knowledge, and again immediately after course completion.
Professional development report and practice outcomes survey
An activities summary report, consisting of a checklist of prescribed postcourse activities, was administered at the end of each course, with instructions to complete and return six months after course completion. A follow-up clinical practice survey was administered 1-year after the course. The survey requested a tally of patients seen for cancer risk assessment and included open-ended questions eliciting the impact of training on practice skills, interest in continued cancer genetics education, and professional self-efficacy (the participant's belief that he or she is able to take the appropriate actions required to perform a task). Postcourse summaries and surveys were transmitted via e-mail or fax.
Participant satisfaction
Satisfaction with the curriculum and course delivery was elicited through standard CME evaluation of each module during the course and attached to the postcourse test (described earlier). Several items assessed the function and utility of the Genetics Link web board. Given that the functionality and use of the web board evolved over the 3 years, user statistics were not considered a primary endpoint, and responses were used to inform continued development of this pilot tool. Comments and suggestions for improvement in course content and delivery were summarized and served to guide refinements in the course each year.
Data analysis
The pre- and posttest question responses were scored using the test answer key, and the percent correct was calculated. Descriptive statistics were calculated on profession, specialty, and pre- and posttest scores. A paired t test was used to test knowledge gain for the entire group. A knowledge gain score was calculated by subtracting pre from post scores, and an independent t test of knowledge gain by profession was conducted to compare GCs and APNs (there were too few MDs to include in the analysis). Deductive content analysis was performed on open-ended survey responses.
RESULTS
Knowledge outcomes
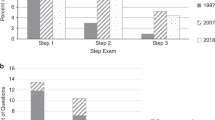
As shown in Table 4, there was a significant increase in cancer genetics knowledge for the entire group (t(39) = 6.67; P < 0.001). The overall pretest score was 65% correct, and the overall posttest score was 80% correct. There was a significant difference in baseline knowledge scores between GCs and APNs (F(1,35) = 22.2; P < 0.001). Although knowledge gain for APNs was 36% and for GCs was only 17%, there was no significant difference in knowledge gain between these two subgroups (t(35) = 1.72, P = 0.094). Comparison of baseline scores and knowledge improvement between the APNs with specialty practices in oncology compared with nurses with specialty practices in genetics showed no significant differences in these measures. Although they demonstrated a gain in knowledge, going from 64% correct on the pretest to 73% correct on the post test (a 16% improvement), because only three physicians participated in the course, we did not compare their performance to the GCs and APNs.
Continued professional development
Thirty-five of 40 total course alumni (88%) fulfilled prescribed postcourse professional development activities and returned a completed activities summary report 6 months after completing the course. All respondents completed the reading assignments; 22 (63%) conducted one, and 13 (37%) reported conducting from two to five presentations (seminars) on cancer risk assessment to medical professionals within their institution or community. Thirty-one of respondents (89%) attended one or more professional organization seminars related to cancer genetics (ASHG, ASCO, NSGC, ISONG).
Several community-based course participants indicated interest in participating in clinical research related to genetics, despite their nonacademic practice setting. Three course alumni sought expanded ties to the Cancer Center Cancer Screening & Prevention Program Network (CSPPN) to obtain ongoing support of practice development and to collaborate in cancer prevention research activities, and two of these three contributed to the course by presenting a workshop on setting up a cancer risk assessment practice based on their own experiences as part of the second and third course offerings.
Practice outcomes
Of 40 total alumni, 35 were actively practicing cancer risk assessment 1 year after completion of the course (two had altered the focus of their practices, two stated that institutional changes had delayed development of their practices, and one was not practicing due to illness). Twenty-nine of forty alumni (73%) responded to the 1-year postcourse survey. Seven respondents had established or were in the process of setting up a new cancer genetics risk assessment practice, and reported an overall total of 38 patients seen in their new practices in 6 months since completing the course. Of the 29 respondents who had previous practice experience, 19 (66%) reported an increase in the number of patients seen for cancer risk assessment. Open-ended questions elicited such statements as, “the number of cancer risk assessment cases assigned to me has increased in number (approximately 2-fold) as a consequence of being identified as ‘the expert’ in our clinical staff after the intensive course,” and “the course helped me streamline the number of patient visits and the intake process.” Four respondents noted that they were receiving more referrals as a direct result of course-prescribed professional and community educational outreach about hereditary cancer and cancer risk assessment.
Professional self-efficacy was measured by content analyzing responses to the open-ended question, “What, if any influence did taking the course have on your practice? Please describe.” Twenty-two (76%) respondents indicated that taking the course increased professional self-efficacy, as determined by such responses as, “my level of confidence was greatly enhanced, allowing me to move forward with the genetics program at my institution,” “the course gave me more confidence in promoting my own cancer genetics practice,” and “I feel more confident about what I know about cancer genetic counseling.” Eighteen (62%) of respondents specified that the course improved their ability and confidence related to skills such as taking a cancer-focused family history, use of probability and risk assessment tools, selecting and interpreting genetic test results, and providing risk-appropriate surveillance and management recommendations.
Participant satisfaction
The majority of alumni reported that taking the course was well worthwhile, and that training with professionals with different backgrounds was an enhancement to the overall learning experience, as participants from different training backgrounds were able to share their experiences and areas of knowledge in an intimate interactive learning environment. Alumni critiques mentioned the difficulty and logistics of on-site attendance for nearly 2 full weeks, and the desire for ongoing distance support for practical integration of the new knowledge into community-based practice.
Most respondents (95%) indicated that they continue to use and benefit from course resources (syllabus, articles, and written materials and referral guidelines). Of these, 30% reported that they use the Genetics Link web board. Some indicated its potential value for continued practice development, as suggested by such statements as, “The availability of the web-board and ‘consultations’ with the CSPPN experts allows me to help more patients in the local region without needing to send them for comprehensive services located 3 1/2 hours away.”
Analysis of usage statistics (web trends) indicated very little use of the web board initially. Several alumni reported that they experienced technical difficulties as a major barrier to using the site, which is restricted to members and password protected. Improvements in the technical interface resulted in a simpler and more reliable gateway and yielded significant increase in transactions on the site from several participants from the last offering of the course. Most of the queries were for advice about challenging cases encountered in practice. Additional feedback from alumni about the function, usability, and content of the web board was used to improve the interface each year of the course as more features were implemented.
DISCUSSION
Once the exclusive domain of academic health centers, clinical cancer genetics services are increasingly being delivered in community settings. The full subscription in this 10-day intensive course by working clinicians demonstrates the need for and motivation to participate in clinical cancer genetics training. It was noteworthy that although the course was exclusively marketed to GCs and APNs, several MDs who learned about the course by word of mouth approached us to participate, and of those, three made the time commitment to participate—a further testament to the interest and motivation for training in this subspecialty.
Interest in cancer genetics training is also reflected in the results of a needs assessment survey we distributed in the fall of 2002 to genetic counselors and oncology nurses during the NSGC annual meeting and to both the ISONG and NSGC listserves. The survey was composed of eight questions related to perceived need for and interest in cancer genetics training. Of 125 respondents (88 genetic counselors, 31 nurses, 6 PhDs), 78% stated they currently provide some level of cancer risk assessment services, and 82% expressed interest in attending a cancer genetics training course (unpublished data, 2004). We currently have a log of 47 genetic counselors, APNs, and MDs or PhDs in clinical practice who have inquired within the last year about the course, based on word-of-mouth among professionals
Recent literature has suggested that although traditional lecture format approaches to CME often do not change physician behavior,36 small group interactive educational formats with case-based learning in the model of the intensive course are more often result in the translation of newly acquired knowledge into practice changes.37,38 The efficacy of intensive interdisciplinary training through this course was demonstrated in part by the significant improvement in cancer genetics knowledge, and by the successful application of attained knowledge and skills by course alumni with different professional backgrounds.
A more subjective measure of the program's success is the professional self-efficacy reported by course alumni. As we were unable to directly monitor the postcourse activities of participants, we measured professional self-efficacy and self-reported improvement in cancer genetics risk assessment skills, which have been found to serve as acceptable surrogates for direct assessment of performance.39,40 Furthermore, the use of broad, open-ended questions allows for spontaneous, uncued responses. Finally, the high level of compliance with recommended postcourse activities suggests that the course design was successful in fostering continued self-education and practice development.
In addition to its highly interdisciplinary curriculum, the greatest novelty of the course was the purposeful admixing of different disciplines among the participants, with MDs, GCs, and APNs training side by side. Considering the experimental nature of this training model, it was instructive to reflect on the very positive interactions of the participants. Informal observations of classroom dynamics indicated smooth, productive interactions between and among participants of different disciplines. Not surprising, the clinical genetics physicians, who are in general accustomed to working closely with interdisciplinary teams that include GCs and nurses, worked well with both groups. Furthermore, despite potential turf issues, the APNS and GCs also worked well together, and all disciplines shared perspectives, knowledge, and resources openly and enthusiastically. These observations were also reflected in postcourse evaluations by the participants, who overall stated that the intermixing of disciplines enhanced their learning experience, and suggest that the course may serve as a model for highly specialized inter- and cross-disciplinary cancer genetics training.
The results of this course suggest that multifaceted, interdisciplinary training in cancer risk assessment promotes competence in clinical cancer genetics for a selected subset of motivated clinicians with previous training in either clinical genetics or clinical oncology and a supportive practice setting. Given the complex nature of the cancer genetics information, these results may not be generalized to health professionals without advanced degrees or similar background training. Consequently, we believe that for the time being, training programs in cancer risk assessment and counseling should continue to target masters or doctoral-level clinicians with either oncology or genetics training, and should strive to address the areas of competency outlined in published professional practice guidelines.8,29,41
Despite the fact that demand for the course exceeded capacity and the participants considered the breadth of content to be valuable to intensive training, feedback from course alumni and from our needs assessment survey indicated that whereas the face-to-face element of the program was essential, a shorter on-campus time commitment would make the course more attractive and more feasible for working practitioners to attend. Therefore, future course offerings should consider mechanisms to abbreviate the on-site training portion of the course without compromising course content. This may be accomplished by using a multimodal approach to curriculum delivery, with a self-directed distance learning component (CD-Rom or web-based) for elements of the core didactic content, combined with shorter on-campus commitment for reinforcement of didactic learning through interactive case-based training, mock risk assessment and counseling sessions, and multidisciplinary workshops.
The demand for clinicians with specialized training in cancer risk assessment is certain to increase as discoveries related to moderate risk genes, gene-gene, and gene-environment interactions moves from bench to bedside, yet the shortage of health care professionals with specialized genetic cancer risk assessment skills remains a barrier to the efficient identification and management of high-risk individuals. Comprehensive interdisciplinary training in cancer risk assessment for clinicians with genetics or oncology practice specialties should improve access to high-quality cancer risk assessment services in the community setting.
References
Burke W, Petersen G, Lynch P, Botkin J, Daly M, Garber J, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. I. Hereditary nonpolyposis colon cancer. Cancer Genetics Studies Consortium. JAMA 1997; 277: 915–919.
Burke W, Daly M, Garber J, Botkin J, Kahn MJ, Lynch P, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer Genetics Studies Consortium. JAMA 1997; 277: 997–1003.
Scheuer L, Kauff N, Robson M, Kelly B, Barakat R, Satagopan J, et al. Outcome of preventive surgery and screening for breast and ovarian cancer in BRCA mutation carriers. J Clin Oncol 2002; 20: 1260–1268.
Hartmann LC, Sellers TA, Schaid DJ, Frank TS, Soderberg CL, Sitta DL, et al. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst 2001; 93: 1633–1637.
Kauff ND, Satagopan JM, Robson ME, Scheuer L, Hensley M, Hudis CA, et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 2002; 346: 1609–1615.
Rebbeck TR, Lynch HT, Neuhausen SL, Narod SA, Van't Veer L, Garber JE, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 2002; 346: 1616–1622.
Lerman C, Hughes C, Lemon SJ, Main D, Snyder C, Durham C, et al. What you don't know can hurt you: adverse psychologic effects in members of BRCA1-linked and BRCA2 linked families who decline genetic testing. J Clin Oncol 1998; 16: 1650–1654.
ASCO American Society of Clinical Oncology Policy Statement Update: Genetic testing for cancer susceptibility. J Clin Oncol 2003; 21: 2397–2406.
Daly MB, Angelos P, Bryant E, Buys S, Eng C, Engstrom PF, et al. NCCN practice guidelines: Genetic/familial high-risk assessment: Breast [Monograph on CDROM]. Available at: http://www.nccn.org. Accessed June 1, 2003, 2003.
Fries MH, Holt C, Carpenter I, Carter CL, Daniels J, Flanagan J, et al. Guidelines for evaluation of patients at risk for inherited breast and ovarian cancer: recommendations of the Department of Defense Familial Breast/Ovarian Cancer Research Project. Mil Med 2002; 167: 93–98.
ACMG Genetic susceptibility to breast and ovarian cancer: assessment, counseling and testing guidelines executive summary. American College of Medical Genetics: New York State Department of Health; 1999; 1–40.
McKinnon WC, Baty BJ, Bennett RL, Magee M, Neufeld-Kaiser WA, Peters KF, et al. Predisposition genetic testing for late-onset disorders in adults. A position paper of the National Society of Genetic Counselors. JAMA 1997; 278: 1217–1220.
Weitzel JN . Genetic counseling for familial cancer risk. Hospital Practice 1996; 31: 57–69.
(ASHG) Statement of The American Society of Human Genetics on genetic testing for breast and ovarian cancer predisposition. Am J Hum Genet 1994; 55: 22–25.
Bennett RL, Hampel HL, Mandell JB, Marks JH . Genetic counselors: translating genomic science into clinical practice. J Clin Invest 2003; 112: 1274–1279.
Reynolds PP, Benkendorf JL . Genes and generalists: why we need professionals with added competencies. West J Med 1999; 171: 375–379.
Stopfer JE . Genetic counseling and clinical cancer genetics services. Semin Surg Oncol 2000; 18: 347–357.
Peters JA, Stopfer JE . Role of the genetic counselor in familial cancer. Oncol 1996; 10: 159–182.
ASHG/ACMG The American Society of Human Genetics Social Issues Committee and The American College of Medical Genetics Social EaLIC ASHG/ACMG Statement. Genetic testing in adoption. Am J Hum Genet 2000; 66: 761–767.
Koil CE, Everett JN, Hoechstetter L, Ricer RE, Huelsman KM . Differences in physician referral practices and attitudes regarding hereditary breast cancer by clinical practice location. Genet Med 2003; 5: 364–369.
Wideroff L, Freedman AN, Olson L, Klabunde CN, Davis W, Srinath KP, et al. Physician use of genetic testing for cancer susceptibility: results of a national survey. Cancer Epidemiol Biomarkers Prev 2003; 12: 295–303.
Cho M, Sankar P, Wolpe P, Godmilow L . Commercialization of BRCA1/2 testing: practitioner awareness and use of a new genetic test. Am J Med Genet 1999; 83: 157–163.
Myers MF, Doksum T, Holtzman NA . Genetic services for common complex disorders: surveys of health maintenance organizations and academic genetic centers. Genet Med 1999; 1: 272–285.
Menasha JD, Schechter C, Willner J . Genetic testing: a physician's perspective. Mt Sinai J Med 2000; 67: 144–151.
Acton RT, Burst NM, Casebeer L, Ferguson SM, Greene P, Laird BL, et al. Knowledge, attitudes, and behaviors of Alabama's primary care physicians regarding cancer genetics. Acad Med 2000; 75: 850–852.
Wilkins-Haug L, Erickson K, Hill L, Power M, Holzman GB, Schulkin J . Obstetrician-gynecologists' opinions and attitudes on the role of genetics in women's health. J Womens Health Gend Based Med 2000; 9: 873–879.
Hayflick SJ, Eiff MP, Carpenter L, Steinberger J . Primary care physicians' utilization and perceptions of genetics services. Genet Med 1998; 1: 13–21.
Greco KE, Mahon SM . Genetics nursing practice enters a new era with credentialing. The Internet Journal of Advanced Nursing Practice 2003; 5.
Calzone KA, Jenkins J, Masny A . Core competencies in cancer genetics for advanced practice oncology nurses. Oncol Nurs Forum 2002; 29: 1327–1333.
(ASCO) Training resource document for curriculum development in medical oncology. J Clin Oncol 1998; 16: 372–379.
ASHG Report. Report from the ASHG Information and Education Committee: medical school core curriculum in genetics. ASHG Information and Education Committee. Am J Hum Genet 1995; 56: 535–537.
Weitzel JN . Genetic cancer risk assessment: Putting it all together. Cancer 1999; 86: 2483–2492.
ASCO Cancer Genetics & Cancer Predisposition Testing. ASCO Curriculum. Vol 1 & 2. Alexandria, Va: American Society of Clinical Oncology; 1998.
Blazer KR, Grant M, Sand SR, MacDonald DJ, Choi JJ, Nedelcu RA, et al. Development of a cancer genetics education program for clinicians. J Cancer Educ 2002; 17: 69–73.
Blazer KR, Grant M, Sand SR, MacDonald DJ, Uman GC, Weitzel JN . Effects of a cancer genetics education programme on clinicians knowledge and practice. J Med Genet 2004; 41: 518–522.
Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A . Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?. JAMA 1999; 282: 867–874.
Slotnick HB . How doctors learn: the role of clinical problems across the medical school-to-practice continuum. Acad Med 1996; 71: 28–34.
Dixon J . Evaluation criteria in studies of continuing education in the health professions: a critical review and a suggested strategy. Eval Health Prof 1978; 1: 47–65.
Velde B, Lust C . Using a learning community to enhance course integration in a school of allied health. J Allied Health 2004; 33: 55–61.
Maibach E, Murphy DA . Self-efficacy in health promotion research and practice: conceptualization and measurement. Health Educ Res Theory Pract 1995; 10: 37–50.
Trepanier A, Ahrens M, McKinnon W, Peters J, Stopfer J, Grumet S, et al. Genetic Cancer Risk Assessment and Counseling: Recommendations of the National Society of Genetic Counselors. J Genet Counsel 2004; 13: 81–111.
Acknowledgements
The City of Hope Intensive Course in Clinical Cancer Genetics was developed through COH Center for Cancer Genetics Technology Transfer Research (CCGTTR) project, supported by the California Cancer Research Program of the University of California no. 99-86874. Curriculum development was supported in part by R25CA no. 75131 from the NCI. The authors wish to acknowledge Padma Mantha, BSC, Raluca Nedelcu, MS, CGC, Alejandra Wright, Bernadette Pabillare, Veronica Lagos and Alexandra Arad for assistance with program coordination, data collection, and manuscript preparation.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Blazer, K., MacDonald, D., Ricker, C. et al. Outcomes from intensive training in genetic cancer risk counseling for clinicians. Genet Med 7, 40–47 (2005). https://doi.org/10.1097/01.GIM.0000151154.27612.49
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/01.GIM.0000151154.27612.49
Keywords
This article is cited by
-
Clinical interpretation of pathogenic ATM and CHEK2 variants on multigene panel tests: navigating moderate risk
Familial Cancer (2018)
-
Impact of Web-Based Case Conferencing on Cancer Genetics Training Outcomes for Community-Based Clinicians
Journal of Cancer Education (2012)
-
Genetic educational needs and the role of genetics in primary care: a focus group study with multiple perspectives
BMC Family Practice (2011)
-
Mentoring Nurses in Familial Cancer Risk Assessment and Counseling: Lessons Learned From a Formative Evaluation
Journal of Genetic Counseling (2008)
-
Anticipating dissemination of cancer genomics in public health: A theoretical approach to psychosocial and behavioral challenges
Annals of Behavioral Medicine (2007)