Abstract
Purpose
Increased implementation of complex genetic technologies in clinical practice emphasizes the urgency of genomic literacy and proficiency for medical professionals. We evaluated our genomic education model.
Methods
We assessed the 5-day, extended format program, encompassing lectures, videos, interactive tests, practice cases, and clinical exercises. Pre- and post questionnaires assessed knowledge change, using t-tests to compare groups. Satisfaction on program completion and after 3 years were evaluated. Implementation in other centers determined acceptability.
Results
During 2012–2018, 774 clinicians from multiple disciplines and career stages attended 35 programs; 334 (43%) attended the 5-day extended format. Evaluations showed significant improvement of genomic literacy (mean 15.05/100 points, p < 0.001). Residents initially had higher scores than specialists (pre: 66.3 ± 17.3 vs. 58.7 ± 16.6, respectively, p = 0.002); both significantly improved, with specialists “catching up” (post: 79.1 ± 17.2 vs. 75.7 ± 15.9, nonsignificant (NS)); there was a similar trend between fellows and subspecialists (pre: 70 ± 18 vs. 59.4 ± 16.4, respectively, p = 0.007; post: 78.6 ± 16.4 vs. 73.2 ± 17.7, respectively, NS). Younger specialists (≤10 years residency) had significantly higher pre- and post scores. Absolute improvement in scores did not depend on medical specialties.
Conclusion
Our program is effective in improving genomics literacy for clinicians, irrespective of career length or expertise, and could be a model for improving skills in practical genomics for all medical professionals.
Similar content being viewed by others
INTRODUCTION
Over the past decade, there has been a dramatic rise in the use of genetic counseling and testing in clinical practice. This is probably due to a combination of factors, such as the inclusion of new genomic technologies in national health insurance programs, and a growing number of physicians subspecializing in medical genetics.
In Israel, we witnessed this rise as well. In 2013, chromosomal microarray (CMA) was included in the national health basket, followed by single-gene sequencing (Sanger) in 2015, next-generation sequencing (NGS) sequencing in 2017, exome “trios” in 2018, and recently NGS panels in 2019. The number of newly board-certified specialists in medical geneticists has increased nearly fourfold during since 2013.
In accordance with Israel regulations, referrals to genetic testing must be carried out by medical geneticists or specialists in their respective fields (for example, referral to prenatal genetic testing by obstetricians). Due to the shortage of genetic professionals, proficiency of physicians in genetic testing is of utmost importance, as it is for physicians practicing in the United States and most centers in Europe.
New genomic technologies are constantly emerging. In current medicine, knowledge of genetics and genomics is imperative for medical professionals.
The need for providing nurses with genomic education for managing their patients was previously described.1 A recent study2 demonstrates the need for continuing education for genetic counselors due to the continuous rapid expansion of genetic technologies. The authors conclude that “indeed fundamental changes may be warranted” regarding genetic counselors’ knowledge, skills, and attitudes.
With the increasing implementation of genomic technologies into the clinic, physicians are also expected to be proficient in this field. A systematic literature review on primary care providers’ barriers against provision of genetic testing found that knowledge about genomics was one of the most common.3
A recent survey assessing the need for genomic education and training in England’s National Health Service (NHS) emphasized the importance of ongoing awareness about genomics, as some health-care professionals are unaware how genomics can be applied to health care. The conclusion was that general information should be targeted to professional groups, in addition to cross-professional resources in specific clinical areas.4
Genetic training of physicians is offered in various programs across Europe and the United States. Despite evidence of progress in training nongenetic health professionals in genetics, there is a need for a standardized model and effective programs for practicing physicians. Such a model would potentially enable high quality training of a growing number of health-care providers.
A recent systematic review summarized different aspects of programs described in the literature.5 Although 44 articles about genetic training programs were included, most studies had few participants (less than 100). In addition, less than half were based on theoretical frameworks, or included information about participants’ years of practice.
A 2015–2018 review of genomic medicine education and training articles describes various genomic education initiatives. The authors conclude these programs should be assessed systematically to create an optimal evidence-based program, and that utilizing genetics specialists to teach physicians is an effective approach that enables interdisciplinary collaboration.6
Our mission is to teach physicians principles of genomic medicine, and proficiency in various aspects of genetic testing such as indications, advantages, test results interpretation along with their clinical implications, and limitations of various novel technologies. This would enable clinicians to guide their patients through the genetic evaluation process, to the benefit of all parties.
We present our genomic medicine education program and analyze its quality with regard to knowledge change, teaching techniques, participants’ satisfaction, and acceptability.
The study objective was to evaluate the strength of our genomic education model in improving genomic knowledge among practicing physicians.
MATERIALS AND METHODS
Program description
In 2012, we established a genomic medical education program for physicians at the Recanati Genetic Institute, Rabin Medical Center, in Israel.
Participants
The program was designed for practicing physicians in multiple disciplines of medicine, working in hospitals or outpatient clinics. The courses were offered to physicians from all stages of training/practice, from residency to retired physicians. To ensure effective learning, we required participants be completely engaged in the course, and dedicate their undivided attention to learning.
Lecturers and teaching
The course director was present at all lectures. The 23 lecturers were highly motivated and scientifically updated certified medical geneticists. They were encouraged to attend their colleagues’ lectures to develop continuity between lectures and avoid gaps in the learning process. Participants evaluated the lecturers at the end of each course to guide improvements in subsequent courses. We used social media (e.g., email or WhatsApp groups) for effective communication between participants and lecturers (questions and answers, referrals to recommended reading materials, etc.).
Topics
The opening lectures were dedicated to basic knowledge in genetics and terminology and principal genomic tests used in medicine and research to provide the fundamental tools that would serve participants from varied backgrounds. These were followed by various topics in clinical genetics such as oncogenetics, reproductive genetics, and pediatric genetics. Application of different genomic technologies was presented in each field, using actual cases that had presented at our clinic. State of the art topics such as epigenetics and genetic treatments were addressed, as well as lectures on complexities, ethics, and legal regulations related to genetic counseling and testing. The courses included guided visits to the medical genetic laboratories.
Format and learning tools
The workshop schedule varied among the program’s formats, from one day (8 hours) to the most extended format consisting of 5 consecutive 8-hour days. The workshops combined frontal lectures, interactive multiple-choice tests (smart phone based), exercises involving clinical cases (interpreting pedigrees and laboratory results), as well as other methods. Participants received preparatory learning materials ahead of the course, including printed booklets with lectures slides, as well as computer access to all course files. Teaching videos were sent as an additional learning tool, to further strengthen skills acquired during lectures. Participants were allowed time for questions at the beginning and end of each day. In the extended format, the participants received daily homework assignments consisting of 10 multiple-choice questions, which were reviewed in the following class.
Following the courses, we maintained contact with our graduates and continuously updated them with key articles in the field and invitations to genomic conferences. We encouraged communications through social media, to facilitate consultation and cooperation for both clinical and research purposes.
To enable more participants to attend our courses, we created four additional program formats. These included weekly afternoon classes, courses designed for physicians in specific subspecialties, bioinformatics for geneticists, and continued education courses for graduates. Several participants attended more than one course, sometimes in different formats. The different course formats are detailed in Table 1.
Program evaluation
We used several methods to analyze the quality of our program:
-
1.
Effectiveness: improvement of test scores between the first and last day of the course (post-test minus pretest).
-
2.
Satisfaction of participants: questionnaires were filled out immediately upon course completion and at follow-up 3 years later.
-
3.
Uptake: implementation of course programs in other centers in Israel and abroad.
Statistical analysis
Analyses were performed with SAS version 9.4 software package (SAS, Cary, NC, USA), and t tests were used to compare pre- and post-test scores overall, and between different groups of participants (according to medical discipline and years of medical practice). Wilcoxon nonparametric tests yielded the same results, and normal distribution was also demonstrated visually. Comparison of score improvement between various medical fields was performed by Tukey–Kramer post hoc analysis.
RESULTS
Description of courses
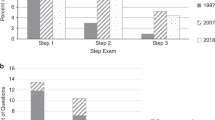
During our 7-year educational experience, we held 35 courses overall; 19 were 5-day courses and 16 had other formats. Growth in education volume is presented in Fig. 1, both by number of participants and hours of education. Table 2 summarizes the days and hours of all courses provided.
Description of participants
The 774 medical personnel (691 physicians; 83 genetic counselors and laboratory workers) who participated in the programs included mostly clinicians from various disciplines and career stages, but also researchers, lab personnel, and health-care managers from different positions in hospitals, health maintenance organizations (HMOs), and the Ministry of Health (e.g., clinic directors, department chairs).
As presented in Table 2, among the physicians participating, 137/691 (20%) were residents and 554/691 (80%) board-certified specialists, among whom 123/554 (22%) were department chairs. Most worked in 1 of 24 different tertiary medical centers throughout Israel, 8% (46) in outpatient centers, and a few were lab workers.
The physicians were from 33 different medical disciplines (see Fig. 2). Of those with known fields of practice, 332 (52%) were from internal medicine, 200 (31%) pediatricians, and 112 (17%) from surgical fields (including gynecologists).
Five percent of participants were classified as other. *Other internal includes pulmonology, psychiatry, radiology, anesthesiology, immunology, rheumatology. **Other pediatrics includes pediatric pulmonology, pediatric gastroenterology, pediatric cardiology, pediatric hematology, pediatric rheumatology. ***Other surgery includes orthopedics, plastic, ENT, urology.
Program evaluation
Score improvement
Pretest and post-test results are reported in Table 3. Test scores improved significantly for all groups (mean 15.05, p < 0.001). Residents initially had higher scores than specialists (pretest score 66.3 ± 17.3 vs. 58.7 ± 16.6, respectively, p = 0.002). Scores of both groups improved significantly, by similar magnitude, with specialists “catching up” (post-test 79.1 ± 17.2 vs. 75.7 ± 15.9, nonsignificant (NS)). The trend was similar when comparing physicians training in a subspecialty (fellows) and physicians who had completed their subspecialty (pretest 70 ± 18 vs. 59.4 ± 16.4, p = 0.007, post-test 78.6 ± 16.4 vs. 73.2 ± 17.7, NS). Specialists who had completed medical training within the past 10 years had significantly higher scores than those practicing >10 years, both before and after the program, but all participants improved dramatically. Scores did not depend on the specialty field, and degree of improvement in knowledge due to the course was equivalent, regardless of practice years. However, in post hoc analysis of specialty fields adjusted for years of practice, there was a tendency toward greater improvement for surgeons (mostly obstetricians) compared with pediatricians (delta 17.4 points vs. 11.7 points, respectively, p = 0.09 (NS).
Satisfaction of participants
Participants were extremely satisfied with the program in general, and particularly with the clinical approach. They reported satisfaction on all levels, including content, lecturers, organization, exercises, and learning tools, and supported the 5-day intensive learning format without interruptions, due to demanding work schedules that would not have enabled learning in parallel. Most physicians had finished their medical training at least 10 years before the course, therefore were impressed by the great advancements in the field. They expressed their satisfaction with a course that covered a huge gap in their knowledge, which would not have been covered otherwise. Some compared this new genomic language with “learning any other language” or “learning how to swim.” They enjoyed the use of example clinical cases from their practices rather than textbook cases, which naturally included cases with mistakes and negative results. Actual laboratory results from their own patients were presented and helped them better appreciate the clinical context, rather than hypothetical results from literature. Availability of the lecturers for questions contributed to their satisfaction, as well as the variety of fields among the participants, which enabled case examples from multiple disciplines of medicine.
Participants remembered the course fondly after 3 years and had made good use of skills acquired during the workshops. Perhaps the best indicator of satisfaction was that many expressed interests in attending additional courses to refresh their memory and learning new updates on genetic technologies.
Uptake and acceptability
This parameter was more difficult to quantify than knowledge, quality, and satisfaction. However, five other medical centers throughout Israel have adopted our teaching format, and the extended format course was held a couple of times for participants overseas (Moscow and Yekaterinburg, Russia).
In addition, in recent years we have seen a rise in the number of referrals for genetic testing, and more willingness of HMO regulators in Israel to accept these referrals, despite high costs. We believe that the increase in genetic testing may be partially due to changes in attitude of many physicians after participating in our workshop. Therefore, they are more comfortable incorporating genetics into their practices. We expect this trend to continue as more physicians learn about genomics.
DISCUSSION
We describe our program that encompassed nearly 800 participants in a 7-year period (2012–2018). Analysis demonstrated effectiveness in improving genetics knowledge among all physicians, from all backgrounds, years of practice, medicine disciplines, and positions. Although we observed similar improvements in score, the younger physicians scored higher than their senior colleagues, both in pretests and post-tests. Residents and fellows had higher pretest scores than specialists and subspecialists, respectively, but post-test scores were not significantly different.
Our findings are in line with previous reports from the literature, which show that knowledge in genetics is linked to a younger age, since recently graduated clinicians are better trained in this field.7,8,9
The more senior physicians, many of whom are chairmen, department heads, regulators, etc., showed less knowledge at both stages. This may be because the junior physicians completed their medical training more recently, and have more baseline knowledge in genetics, compared with their older colleagues who attended medical school prior to the era of genomic medicine. Medical training in later years may also have provided more “genomic familiarity” and facilitated acquirement of genomic approach and knowledge. One must also take into consideration that younger age is an advantage for learning new fields both in general, and specifically in terms of ability to dedicate time to learning, as more senior physicians usually have more work commitments.
Based on our experience, physicians at any level of practice would likely benefit from the workshop. However, the optimal timing for genomic training is probably shortly after completing residency programs, as this is the point in the physician’s career with the greatest potential for utilization of genetic tests. However, it may be important to include department heads in genomic courses to facilitate implementation of new genetic tests into the health-care system. We did not evaluate optimal timing for training, and plan to do so in future studies.
We have observed a dramatic increase in genomic testing in all fields of medicine over recent years, for many reasons, including their inclusion in Israel’s health basket of services. It is possible that improvement in physicians’ attitudes, skills, and confidence in their own abilities after obtaining knowledge in genetics has also contributed to this process. Examining the association between participation in genomic workshops and increased use of genomic testing is another goal for future studies.
Since we only had 1–3 courses in other formats, these were not assessed formally. However, from our experience, afternoon classes were less successful than the 5-day course, probably due to long intervals between lectures (2 weeks), which disrupted continuity. Long intervals are detrimental to the learning process, especially when new and technically difficult materials are being presented. In addition, afternoon courses involved less commitment of the participants in attendance and assignment completion. The extended courses enabled physicians to completely focus on and be devoted to the course, as they freed their schedules from work routines and clinical commitments.
Workshops catering to physicians according to subspecialties had excellent results, both in improvement in knowledge and skills, and participant satisfaction. This may largely be explained by participants’ similar baseline level of knowledge with more targeted teaching to the participants’ knowledge, topics of interest, and expected goals. Due the high success rate, this may be the most beneficial format, which we plan to repeat in future courses.
A recent review that summarized different aspects of training programs described in the literature5 had significantly fewer participants (less than 100) compared with our study, and most lacked information about participants’ years of practices or were based on theoretical frameworks. Another paper6 on genomic medicine education and training that reviewed articles published in 2015–2017 concluded these programs should be assessed systematically. Our study systematically evaluated a curriculum-based program that, thus far, has included almost 800 participants, with data regarding their medical disciplines and years of practice.
Further research is needed to validate results of our program on a larger scale and in other centers. We aim to continue our educational program in its current formats. and our future direction will also involve online courses (e-learning tool). We plan to continue to evaluate our program using the methods described here as well as others.
To conclude, in the genomic era, physicians need to be knowledgeable in genetics. Training physicians from all fields will potentially increase the use of clinical genetic testing.3 We described an example of a program that may be beneficial for improving the genomic skills and competence of health providers in additional centers.
References
Calzone KA, Cashion A, Feetham S, et al. Nurses transforming health care using genetics and genomics. Nurs Outlook. 2010;58:26–35.
Farwell Hagman KD, Lamb Thrush D, Freeze S, Dorsainville DL, Eichmeyer J, Banks KC. Genomic Technologies Special Interest Group of the National Society of Genetic Counselors. Facing the challenge of genetic counselors’ need for rapid continuing education about genomic technologies. J Genet Couns. 2020 Jan 9; https://doi.org/10.1002/jgc4.1213 [Epub ahead of print].
Mikat-Stevens NA, Larson IA, Tarini BA. Primary-care providers’ perceived barriers to integration of genetics services: a systematic review of the literature. Genet Med. 2015;17:169–176.
Simpson S, Seller A, Bishop M. Using the findings of a national survey to inform the work of England’s Genomics Education Programme. Front Genet. 2019;10:1265.
Talwar D, Tseng TS, Foster M, Xu L, Chen LS. Genetics/genomics education for nongenetic health professionals: a systematic literature review. Genet Med. 2017;19:725–732.
Rubanovich CK, Cheung C, Mandel J, Bloss CS. Physician preparedness for big genomic data: a review of genomic medicine education initiatives in the United States. Hum Mol Genet. 2018;27:R250–R258.
Selkirk CG, Weissman SM, Anderson A, Hulick PJ. Physicians’ preparedness for integration of genomic and pharmacogenetic testing into practice within a major healthcare system. Genet Test Mol Biomarkers. 2013;17:219–225.
Wilkins-Haug L, Hill LD, Power ML, Holzman GB, Schulkin J. Gynecologists’ training, knowledge, and experiences in genetics: a survey. Obstet Gynecol. 2000;95:421–424.
Baars MJH, Henneman L, Ten Kate LP. Deficiency of knowledge of genetics and genetic tests among general practitioners, gynecologists, and pediatricians: a global problem. Genet Med. 2005;7:605–610.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Michaelson-Cohen, R., Salzer-Sheelo, L., Sukenik-Halevy, R. et al. Teaching clinicians practical genomic medicine: 7 years’ experience in a tertiary care center. Genet Med 22, 1703–1709 (2020). https://doi.org/10.1038/s41436-020-0868-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-020-0868-4
Key words
This article is cited by
-
Ordering genetic testing by neurologists: points to consider
Journal of Neurology (2023)
-
Unearthing the Learning of Genomic Medicine in the Workplace: a Qualitative Study
Vocations and Learning (2022)