Abstract
Purpose
We present a novel variation of the traction test of the inferior oblique (IO) muscle. We demonstrate the correlation between the traction test and clinically graded IO overaction and describe the utility of this test to confirm IO weakening.
Methods
We performed a retrospective chart review on all patients who underwent IO surgery and intraoperative intorsion traction tests by a single surgeon over a 10-year period. We compared the traction test results, in ‘clock hours’ of freedom, before and after IO surgery. We correlated the torsion test at start of surgery with clinical observed IO overaction (scale 0 to +4) in 67 IO operations (56 myectomies, 6 anterior transpositions, 4 myotomies, and 1 recession) and compared to a control group of 23 eyes with minimal or no IO overaction.
Results
The mean intorsion freedom in the eyes undergoing IO surgery was less than in control eyes (1.63 vs 1.89 clock hour; P<0.00005). There was a significant inverse relationship between grading of clinical IO action and the intorsion test result (Pearson rank coefficient, (r=−0.45; P<0.00001)). Myectomy produced the greatest change in torsion freedom (mean 1.32 clock hour), with all myectomies showing at least 1 clock hour extra freedom after the surgery.
Conclusions
The intorsion traction test confirmed that the IO stiffness correlated with pre-operative IO overaction grade. While it can be helpful in confirming that the entire IO muscle was weakened, it does not substitute for the careful inspection at the end of surgery to ensure there are no remaining IO fibers.
Similar content being viewed by others
Introduction
Surgery on the inferior oblique (IO) muscle is commonly performed for primary and secondary IO over-actions, dissociated vertical deviations (DVD), and ‘V’ pattern strabismus. There are many different surgical approaches to weaken the IO muscle1, 2 but persistent overaction is a well-recognized complication. Splitting of the IO muscle fibers during hooking or failure to recognize that the IO can have multiple muscle bellies are causes of failure of IO surgery, as portions of the muscle may be left untreated.3, 4
Various authors have described oblique muscle traction tests, or torsional forced duction tests, in order to diagnose disorders of these muscles, both pre-operatively and at the time of surgery.5, 6, 7, 8, 9, 10, 11, 12 Their use intra-operatively has also been touted as a valuable tool to identify and limit the possibility of incomplete weakening of an oblique muscle.6, 7, 8, 12 Traction testing of the rectus muscles is easy to perform and interpret, but traction testing of the obliques is more challenging. The most widely used technique for gauging IO tightness, described by Guyton,6 involves retropulsion, adduction, and depression before a temporal movement is used to assess IO tightness. The test can be difficult to perform for an inexperienced observer, and the assigned grading is subjective in nature.7, 12, 13 More recently, Jung and Holmes12 described a quantitative torsional traction test using a Mendez ring to quantitate the degrees of available rotational movement of the globe.
To our knowledge, there has not been any statistical study of a correlation of a torsional traction test at surgery with clinically graded inferior oblique overaction. Guyton6 showed that there seemed to be a correlation of tightness grading using his technique and pre-operative overaction, but he did not analyze this relationship statistically. In addition, the prior reports of torsion traction tests have not studied its utility as a test to confirm complete IO weakening. Coats and Payssee10 used Guyton’s method in 10 cases of inferior oblique myotomy, and found that 8 of 10 IO muscles showed no change in subjective tightness until the myotomy was complete. Jung and Holmes12 showed 30 degrees’ increase in intorsion movement after IO disinsertion compared to the reading at the start of surgery, but their data was from only 2 eyes.
We describe a simple intorsional traction test for the IO muscle that is easy to perform, grade and interpret, and allows a more objective assessment of IO tightness. In this study we had several objectives. First, we statistically analyzed the correlation of the intorsion traction test at surgery with pre-operative clinical grading of IO oblique overaction. Second, we recorded the intorsion traction test result at the start of IO surgery and after the completion of the procedure on the muscle, to determine the change of torsion improvement, or increased ‘freedom’ of movement, created by the surgery. Third, we compared the results of the traction test in the various causes of IO overaction and also a control group with no IO overaction. Finally, we compared the change in torsion test ‘freedom’ after IO surgery in eyes that underwent IO myectomies, myotomies, anterior transpositions, and recessions.
Materials and methods
We performed a retrospective chart review on all patients who had undergone IO surgery and who had quantitative intorsional traction testing at the time of surgery by a single surgeon (SPK) over a 10-year period. Research ethics board approval was granted for this retrospective chart review by the host institution (Hospital for Sick Children, Toronto).
The surgical techniques employed by the surgeon in this case series included myectomies, involving 10 mm resections of muscle at the insertion,1 2-snip marginal myotomies at the insertion,1 anterior transpositions whereby the IO was inserted in a bunched-up fashion lateral to and collinear with the inferior rectus insertion,2 and recessions of 10 mm.1 All IO surgeries were performed via a fornix approach.
For each of the eyes having IO surgery we documented the diagnosis, pre-operative primary position vertical deviation and clinical grading of the IO overaction (scale of 0 to +4).2 We recorded the intorsion traction test result performed under general anesthesia, without depolarizing agents, at the beginning of surgery and after completion of the procedure on the IO. Post operatively we recorded the primary position vertical deviation and inferior oblique action grading. Finally, in order to assemble a control group, we performed the intorsion traction test on 23 consecutive eyes undergoing primary rectus muscle surgery that showed no or very minimal pre-operative IO overaction (<+1).
The intorsion traction test
The traction test was carried out under anesthesia immediately prior to IO surgery. Figure 1 shows the steps carried out in the traction test. The perilimbal conjunctiva is grasped with toothed forceps at the 3 and 9 o’clock positions and the globe retropulsed into the maximal posterior position allowed by orbital contents. The globe is then intorted until maximal intorsion is reached. The grading is then recorded as the maximal number of ‘clock hours’ of intorsion that can be generated before inferior oblique reaches maximum tension and the forced duction cannot tort the eye further. Each clock hour of intorsion is the equivalent of 30 degrees, and the reading is taken to the nearest 0.5 clock hour. The test is performed again immediately after IO weakening. The difference in reading compared to the pre-surgical result represents the increase in clock hours of freedom of movement of the globe.
Each reading on each eye was performed by the senior author and repeated by an experienced pediatric ophthalmology fellow. The traction test was repeated by both surgeons until they agreed on the result to the nearest 0.5 clock hour (15 degrees). If a rectus muscle procedure was performed on the same eye at the same time as the IO surgery, the torsion result was recorded after the IO surgery was completed and before any rectus muscle was approached.
Data analysis
We analyzed the correlation between pre-operative IO overaction grading and intorsion test result at the start of surgery using the Pearson rank coefficient (performed with SPSS Statistics for Windows, Version 22.0, 2013, IBM Corp, Armonk, NY, USA). We compared the mean traction test for eyes undergoing IO surgery to the test results for the control eyes using unpaired t-test. We also calculated the changes in freedom of torsion before and after IO weakening for each of the different weakening procedures: myectomies, marginal myotomies, anterior transpositions, and recessions.
Results
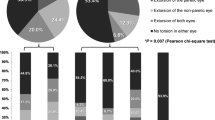
Sixty seven IO-weakening operations were performed on 48 patients. There were 23 eyes in the control group among 15 patients. The distribution of pre-operative diagnoses for all of the study and control patients are listed in Table 1, along with the pre-operative IO overaction grading for all eyes, the surgery performed, vertical misalignment (hypertropia and hypotropia, and DVD), and the traction tests done at the start of surgery. Patients were categorized into the single most appropriate diagnostic group on the basis of why IO surgery was being undertaken, despite in many cases, more than 1 diagnostic criteria being applicable (ie, when IO overaction and DVD coexisted).
Among all of the eyes, the range of intorsion traction at the start of surgery ranged from 1.0 to 2.5 clock hours of freedom. Two eyes with unilateral fourth nerve palsies had myectomy procedures for residual IO overaction following prior recessions. One patient had an anterior transposition surgery, in whom the torsional traction test was performed before and after IO disinsertion but not after reattachment to the globe, and the traction test result for this eye were treated as a myectomy procedure.
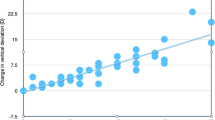
Figure 2 illustrates the correlation between pre-operative IO action and the intorsion traction result at the start of surgery, with the standard deviations for each IO grade. The data presented included both the 23 control eyes and 67 study eyes. Note that 3 control eyes had mild underaction of the IO (graded as −0.5) so it allowed us to plot the data starting from −0.5 underaction to the maximum IO in this series of +3.5. The plot shows a significant inverse relationship between IO action and IO intorsion traction (r=−0.45; P<0.00001). This suggests that the IO has progressively greater ‘stiffness’ the more the pre-operative overaction.
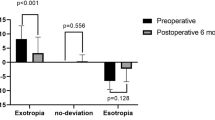
Figure 3 shows the mean intorsion generated for each of the different diagnoses, along with standard deviations. The overall mean traction test result for the 67 eyes undergoing surgery for IO overaction was 1.63 clock hours compared to 1.89 clock hours for the 23 control eyes (unpaired t-test P<0.00005). This confirms that overacting IO muscles are stiffer than non-overacting or minimally-overacting IO muscles.
Figure 4 shows the intorsion traction test result for each of the four IO procedures under anesthesia, prior to and after the IO surgery. The myectomies freed up the traction by an average of 1.32 clock hours, while the myotomies lead to a mean change of 0.90 clock hour. For the anterior transpositions and the recession, the torsion results plotted were at the start of surgery and after reattachment of the IO to the globe. For these 7 eyes the torsion test was not recorded at the time of detachment of the IO and prior to reinsertion of the muscle. The 6 transposition procedures freed up the intorsion by an average of 0.5 clock hour, indicating some relaxing effect of the procedure in addition to its anti-elevation effect. The recession freed up the torsion by 1 full clock hour, indicating a marked relaxing of the muscle when inserted into its recessed position.
Discussion
Traction testing, or forced duction testing, of the globe is an important component in the examination of the strabismus patient. It can help differentiate mechanical from innervational causes of a misalignment, and in turn aids surgical decision-making. When used intra-operatively, this test can confirm that a particular muscle has been weakened or tightened appropriately. In the case of surgery on the IO muscle, the surgeon has to perform an intorsional traction maneuver to assess the tightness of the muscle. There are several methods that have been described to gauge the IO tightness, both qualitatively6, 7, 9 and quantitatively.12
Our results show, for the first time, that there is a statistically significant correlation between a traction test and the clinically graded IO overaction. This trend was suggested by Guyton’s work6 although there was no statistical confirmation of this trend and the method of testing was different. Our results confirm that the torsional traction test is indeed assessing the tautness of the IO itself, as opposed to the muscles and soft tissues that could limit a torsional movement. While the trend was statistically significant, the differences among the grouped data in Figure 1 was small. The presence of 1.5 or 2 clock hours of intorsion freedom on traction testing at the start of surgery does not discriminate between control eyes and those with IO overaction. However, no control group eye had less than 1.5 clock hours of freedom at start of surgery. This suggests that, in an individual eye, a traction test result of less than 1.5 clock hours should be taken as indication of an abnormally taut IO.
There was also a statistically significant difference on the traction test result in those undergoing IO surgery for IO overaction and controls. Again, the differences between groups were small with overlapping results. We have not attempted to reanalyze the data controlling for IO overaction but we suspect that much of the differences between controls and people undergoing IO surgery could be explained by the differences in IO overaction.
It is reasonable to propose the intorsion traction test as an intraoperative aid to determine whether all of the IO has been identified and weakened. At time of primary surgery, patients undergoing myectomy had an increased freedom of average 1.3 clock hours (range 1 to 1.5 hours) after the myectomy, with at least 2.5 clock hours of intorsion evident after IO weakening. Until now, only Jung and Holmes12 published data quantitating the change in freedom after an IO weakening, and they used a Mendez ring to yield exact rotational readings. However, they reported their change in only 2 cases of IO disinsertion, both of whom showed 30 degrees (=one clock hour) of increased freedom. Based on our data and their 2 cases, we feel that the surgeon should anticipate an increase of at least 1 clock hour of freedom after myectomy or disinsertion of an IO muscle, and that this is highly suggestive that all of the IO muscle has been captured and weakened. Any traction tests that show less change in torsion should prompt further exploration of the surgical field for any previously unidentified muscle fibers. This test can be used in all myectomy patients, but it is also applicable in recession and anterior transposition procedures before the muscle is reattached to the globe.
Persistent IO overaction can be caused by a variety of mechanisms including reattachment of the muscle end to the insertion, globe or periocular tissues, or failure to identify a second or third muscle belly.3, 4, 14, 15, 16 In one case of persistent IO overaction after myectomy in this study, we found the IO muscle reattached to the globe in the infero-temporal quadrant away from the site of the original muscle insertion. At the time of the original surgery, the IO traction was freed from 1.5 to 3.0 clock hours. At reoperation, the traction test at the start of surgery showed 1.5 clock hours of torsion freedom, suggesting that the inferior oblique had reattached to the globe.
In a second case of persistent inferior oblique overaction a second operation revealed what appeared to be an unidentified muscle belly was not weakened at the time of the original surgery. At the original surgery, the change in traction test freedom went from 1.5 clock hours to 3 clock hours. At the time of the second surgery the traction test at the start of surgery again measured 1.5 clock hours, suggesting that this muscle may have developed secondary contracture after the initial surgery. After we completed the data collection for this study, we had a different experience in 2 cases of eyes with double-bellied IO muscles. In both cases, the myectomy of the first belly improved the freedom of intorsion by 1.0 clock hours from the initial reading at surgery, and the severing of the second belly led to a further freeing of 0.5 clock hour of intorsion, leading to a total change of 1.5 clock hours of intorsion freedom.
The experience of these 3 cases with multiple bellied IO muscles suggests that the torsion can be freed by at least 1 clock hour even if only one of 2 bellies is weakened. Coats and Paysee,7 using the subjective scale of 0 to 4 tightness as described by Guyton,6 reported a small series of 10 IO myotomies. They found 2 eyes out of 10 in which only partial myotomies (50 and 90%) lead to complete reduction of tightness to zero on their subjective scale. These cases underscore the fact that, irrespective of whether one uses a qualitative or quantitative assessment in the intorsion test, that one still need to be aware of the occurrence of the multibellied inferior oblique muscle.14, 15, 16
All of the patients in this study had the tests performed under general anaesthesia without the use of muscle relaxant drugs and it possible that use of muscle relaxants may change the IO tone and traction test result. Given that the end point of the test is at maximal IO stretch it is our feeling that use of muscle relaxant drugs or depth of anesthesia would produce little if any change to the traction test.
Among the variations of intorsion testing published thus far, the method of Jung and Holmes12 was the first to quantitate the rotational freedom in degrees. Overall, when converting their degrees with the Mendez ring to clock hours, they found less degrees of intorsion than we described in our study. However, our technique differed from theirs in that we retropulsed the globe to bring the inferior oblique into a more coronal plane, allowing relaxation of the other muscles, which may limit torsion, and isolating the inferior oblique. Jung and Holmes did not retropulse the globe to perform their measurements. The retropulsion maneuver is similar to the first steps of the method of Guyton6 and Coats,7 but we have found that the rest of their process is more difficult to grade and is highly subjective. We feel that our method is easy to perform and is reproducible among surgeons. Another advantage of our method is that it is easy to gauge the resistance to further torsional movement. Whilst there is still a degree of subjectivity this reproducible end point does limit inter-observer variation. In the method we suggest in this paper we quantified our results to the nearest 0.5 clock hour (15 degrees) but perhaps greater degree accuracy could be achieved with the addition of a Mendez ring or other protractor as used by Jung and Holmes. Nevertheless, both our method and that of Jung and Holmes provide more objective measurements of the IO intorsion traction test than those of prior authors.
In summary, we describe a variation of the IO intorsion traction test that is quantitative, easy to perform and interpret, and which is reproducible among surgeons. It utilizes a system of clock hours of freedom of torsion. The presence of <1.5 clock hours of torsion on traction testing is indicative of a taut inferior oblique. Myectomy increases the torsion freedom by at least 1 clock hour from the reading at the start of surgery, and any change of less than 1 clock hour should alert the surgeon to check for residual muscle fibers or multiple bellies of the inferior oblique.

References
Parks MM . The weakening surgical procedures for eliminating overaction of the inferior oblique muscle. Am J Ophthalmol 1972; 73: 107–122.
Wright KW, Strube YNJ . Inferior oblique muscle weakening procedures. In: Wright KW, Strube YNJ (eds). Color Atlas Of Strabismus Surgery. Springer: Berlin, 2015; 135–146.
DeAngelis D, Makar I, Kraft SP . Anatomic variations of the inferior oblique muscle: a potential cause of failed inferior oblique weakening surgery. Am J Ophthalmol 1999; 128: 485–488.
DeAngelis DD, Kraft SP . The double-bellied inferior oblique muscle: clinical correlates. J AAPOS 2001; 5: 76–81.
Toosi SH, Von Noorden GK . Effect of isolated inferior oblique myectomy in the management of superior oblique muscle palsy. Am J Ophthalmol 1979; 88: 602–608.
Guyton DL . Exaggerated traction test for the oblique muscles. Ophthalmology 1981; 88: 1035–1039.
Coats DK, Paysse EA . Intraoperative traction testing to detect incomplete inferior oblique myotomy/myectomy. J AAPOS 1997; 1: 197–200.
Plager DA . Traction testing in superior oblique oblique palsy. J Pediatr Ophthalmol Strabismus 1990; 27: 136–140.
Ludwig IH, Clark RA, Stager DR Sr . New strabismus surgical techniques. J AAPOS 2013; 17: 79–88.
Kushner BJ . Superior oblique incarceration syndrome. Arch Ophthalmol 2007; 125: 1070–1076.
Holmes JM, Hatt SR, Leske DA . Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS 2012; 16: 136–140.
Jung JH, Holmes JM . Quantitative intraoperative torsional forced duction test. Ophthalmology 2015; 122: 1932–1938.
Rosenbaum AL . Discussion of Guyton DL: exaggerated traction test for the oblique muscles. Ophthalmology 1981; 88: 1039–1040.
Yalçin B, Ozan H . Insertional pattern of the inferior oblique muscle. Am J Ophthalmol 2005; 139: 504–508.
Emmel DK, Apt L, Foos R . Anatomical variation of the insertion of the inferior oblique muscle. In: Reinecke RD (ed.) Strabismus II: Proceedings of the fourth meeting of the International Strabismological Association. Grune and Stratton: New York, 1984; 669–673.
Paik D-J, Shin SY . An anatomical study of the inferior oblique muscle: the embalmed cadaver vs the fresh cadaver. Am J Ophthalmol 2009; 147: 544–549.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Connor, A., Kraft, S. Intraoperative intorsional traction test of the inferior oblique. Eye 32, 384–390 (2018). https://doi.org/10.1038/eye.2017.200
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.200