Abstract
Background/aims
To identify the factors affecting postoperative horizontal deviation following isolated inferior oblique (IO) weakening surgery.
Methods
The medical records of patients who had undergone isolated IO weakening surgery between February 2010 and September 2021, with a minimum follow-up period of 6 months, were retrospectively reviewed. Patients were divided into two groups, eso-shift, and non-eso-shift, based on the change in horizontal deviation at postoperative 6 months. Eso-shift or exo-shift was defined as a change of 2Δ or more.
Results
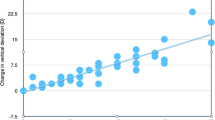
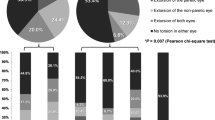
A total of 77 patients were included. Among them, 49 patients (63.6%) showed changes in horizontal deviation: 37 (48.0%) eso-shift, 12 (15.6%) exo-shift. Twenty-eight patients (36.4%) showed no change in alignment. The eso-shift group showed the following characteristics compared to the non-eso-shift group: older age (P < 0.001), higher proportion of patients with preoperative exo-deviation (P < 0.001), and greater preoperative hypertropia in primary gaze (P < 0.001), down gaze (P = 0.031), ipsilateral gaze (P < 0.001), and ipsilateral head tilt (P = 0.002). Regarding the postoperative changes in horizontal deviation based on prior horizontal strabismus, patients with preoperative exo-deviation showed a statistically significant eso-shift. The patients with prior eso-deviation tended toward exo-shift, while those without prior horizontal deviation rarely changed.
Conclusion
Changes in postoperative horizontal deviation are associated with preoperative horizontal and vertical deviation, which might result from changes in the rectus muscle due to oblique muscle dysfunction. Also, this study suggests that isolated IO weakening surgery could effectively correct small-angle horizontal deviation in patients with inferior oblique overaction (IOOA) and horizontal strabismus.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ozsoy E, Gunduz A, Ozturk E. Inferior oblique muscle overaction: clinical features and surgical management. J Ophthalmol 2019;2019:9713189.
Stager DR, Parks MM. Inferior oblique weakening procedures. Effect on primary position horizontal alignment. Arch Ophthalmol 1973;90:15–6.
Rajavi Z, Norouzi S, Sabbaghi H, Yaseri M, Abdi S, Faghihi M. The effect of inferior oblique muscle weakening on horizontal alignment. J Curr Ophthalmol 2019;31:298–304.
Shin JH, Paik HJ. Effect of inferior oblique weakening procedures combined with surgery for intermittent exotropia. J Korean Ophthalmol Soc 2015;56:249–53.
Urist MJ. Surgical treatment of esotropia with bilateral elevation in adduction. AMA Arch Ophthalmol 1952;47:220–47.
Taylan Sekeroglu H, Dikmetas O, Sanac AS, Sener EC, Arslan U. Inferior oblique muscle weakening: is it possible to quantify its effects on horizontal deviations? J Ophthalmol 2012;2012:813085.
Tommila V, Valle O. Effect of inferior oblique muscle recession on horizontal deviation. Acta Ophthalmol (Copenh) 1968;46:779–84.
Bae SH, Kim J, Kim AY, Lee JY, Choi MY, Lim KH, et al. Effect of combining inferior oblique muscle weakening procedures with exotropia surgery on the surgical correction of exotropia. PLoS One 2018;13:e0198002.
Scelfo C, Elhusseiny AM, Alkharashi M. Effect of inferior oblique myectomy on primary position when combined with lateral rectus recession for intermittent exotropia. Eur J Ophthalmol 2022;32:559–62.
Jampel RS. The fundamental principle of the action of the oblique ocular muscles. Am J Ophthalmol 1970;69:623–38.
Von Noorden GK. Binocular vision and ocular motility. Theory and management of strabismus. (1996).
Diamond GR, Parks MM. The effect of superior oblique weakening procedures on primary position horizontal alignment. J Pediatr Ophthalmol Strabismus 1981;18:35–8.
Rajavi Z, Molazadeh A, Ramezani A, Yaseri M. A randomized clinical trial comparing myectomy and recession in the management of inferior oblique muscle overaction. J Pediatr Ophthalmol Strabismus 2011;48:375–80.
Minguini N, Dantas FJ, Monteiro de Carvalho KM, Moreira-Filho DC. A study to determine: should conventional amounts of eye muscle surgery for horizontal binocular deviations be changed when oblique muscle weakening procedures are simultaneously performed? Binocul Vis Strabismus Q 2005;20:21–5.
Kim JM, Kim US. Horizontal effects of 10-mm inferior oblique recession versus 14-mm inferior oblique recession. Korean J Ophthalmol 2018;32:478–82.
Yang HK, Kim JH, Hwang JM. Congenital superior oblique palsy and trochlear nerve absence: a clinical and radiological study. Ophthalmology 2012;119:170–7.
Molinari A, Ugrin MC. Frequency of the superior rectus muscle overaction/contracture syndrome in unilateral fourth nerve palsy. J aapos 2009;13:571–4.
Khawam E, Ghazi N, Salti H. “Jampolsky Syndrome”: superior rectus overaction-contracture syndrome: prevalence, characteristics, etiology and management. Binocul Vis Strabismus Q 2000;15:331–42.
Costenbader FD. The Role of the Oblique Muscles In the ‘A’ and ‘V’ Syndromes*. J Pediatr Ophthalmol Strabismus 1965;2:25–30.
Wang X, Zhang W, Liu L. Effect of isolated oblique muscle weakening procedures on horizontal deviation in A- and V-pattern exotropia. Curr Eye Res 2020;45:211–4.
Funding
This work is supported by grant No.0420200400 from the Seoul National University Hospital (SNUH) Research Fund.
Author information
Authors and Affiliations
Contributions
Conceptualization: S-JK. Study design: S-JK, YG. Data collection: YG. Data and statistical analyses: YG. Drafting the manuscript: YG. Critical revision and final approval of the article: S-JK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gim, Y., Kim, SJ. Factors associated with changes in horizontal deviation after inferior oblique weakening surgery. Eye 38, 600–605 (2024). https://doi.org/10.1038/s41433-023-02741-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02741-3