Abstract
Purpose
To describe a technique which exploits the transparency and toughness of the pre-Descemets layer (Dua’s layer) to safely perform deep anterior lamellar keratoplasty (DALK) and phacoemulsification at the same time.
Methods
Three DALK procedures combined with phacoemulsification were performed by the same surgeon using the big-bubble (BB) technique at the Research Institute of Ophthalmology, Cairo, Egypt. In two cases a type-1 BB, baring Dua’s layer, was achieved and in one case a type-2 BB, baring the Descemet’s membrane (DM), was achieved. The surgeries were video recorded and photo slit-lamp images were taken in the follow-up visits.
Results
DALK with phacoemulsification and lens implant was carried out in both patients where a type-1 BB was achieved. At a follow up of 18 months (first case) and 6 months (second case), the best corrected vision was 6/12 for each. In the case where a type-2 BB was achieved, the DM ruptured during injection of viscoelastic prior to capsulorhexis. The procedure was converted to a penetrating keratoplasty without phacoemulsification.
Conclusion
When a type-1 BB is achieved simultaneous DALK and phacoemulsification can be safely accomplished. Dua’s layer allows a clear view for performing phacoemulsification with the added benefit of its toughness, which can maintain a stable anterior chamber for cataract surgery. This should not be attempted when a type-2 BB is achieved.
Similar content being viewed by others
Introduction
Patients with combined corneal stromal scarring and cataract pose a surgical challenge. Poor visibility through the scarred cornea precludes cataract surgery from being undertaken prior to corneal transplantation. The standard approach is the triple procedure wherein a full thickness corneal transplant is combined with an open-sky extracapsular extraction with lens implant. With the advent of deep anterior lamellar keratoplasty (DALK) and its distinct advantages, there is now a tendency to deal with this situation in a staged approach, the DALK procedure being followed at a later date with phacoemulsification and implant. Both options present risks and have drawbacks.1 The triple procedure has an increased risk of extension of capsulorhexis, posterior capsular tear and vitreous loss.1, 2 The sequential approach subjects the patient to multiple operations and anaesthesia with delayed rehabilitation.1, 2
DALK is the gold standard approach for anterior corneal pathology in eyes with a healthy endothelium as it eliminates the possibility of endothelial rejection and consequent graft failure.3 It is essentially an extraocular procedure which allows for faster rehabilitation and a stronger eye.4 However, when a cataract is also present, cataract surgery has to be deferred to a later date. Attempts to combine phacoemulsification and DALK have been made to maximise the advantage of both procedures in a single sitting. These include lamellar stromal dissection, cataract extraction and completion of stromal dissection3 or Descemet’s membrane (DM) baring and cataract extraction followed by sewing on the donor button.2, 4
Dua et al5 recently demonstrated a pre-Descemet’s layer (Dua’s layer (DL)) which was described by the authors to be much tougher and resilient than DM and could withstand a pressure of around 700 mm of Hg. In this report we describe a technique and clinical application that exploits the knowledge of DL and enabled us to perform successful DALK combined with phacoemulsification and implant (DALK triple) by baring DL prior to lens extraction. We also attempted to simulate the procedure of phacoemulsification after baring DM as reported by others2, 4 with the complication of DM rupture.
Materials and methods
Three combined DALK with lens extraction and implant procedures were attempted. All surgeries were done under general anaesthesia by the same surgeon (AAZ) at the Research Institute of Ophthalmology, Cairo, Egypt. One was in the right eye of a 52-year old male with the best corrected visual acuity (BCVA) of 2/60 due to dense corneal scarring secondary to infectious keratitis and dense cataract. Another was in the left eye of a 20-year old male with central-anterior stromal scarring due to keratoconus and a posterior-polar cataract reducing his BCVA to 2/60. The third case was in the left eye of a 55-year old male with post-herpetic stromal scarring, cataract and a BCVA of 3/60.
Surgical technique
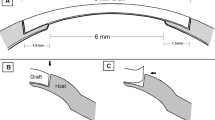
Big bubble (BB)-DALK procedure was performed with a central trephination to a depth of approximately 300 microns with an 8.00 mm vacuum corneal trephine and intrastromal injection of air. A type-1 BB (Pre-DL bubble, central bubble with a white ring)5 was achieved in the first two cases. Two thirds of the corneal stroma constituting the anterior wall of the BB was removed, the central part of the remaining stroma was punctured to deflate the bubble, a spatula was inserted between the stroma and DL and the stroma was divided along the spatula into four quadrants by a cruciate incision, followed by excision of the quadrants.
A sclerocorneal tunnel was performed, a cohesive viscoelastic (healon) was injected in the anterior chamber (AC) followed by a continuous anterior capsulorhexis, hydro-dissection and phacoemulsification of the nucleus by the stop and chop technique. The appropriate lens implant was inserted. An 8.25 mm diameter corneal button from which the DM and endothelium were removed, was sutured in place with 16 interrupted 10/0 nylon sutures.
In the first case, after aspiration of the cortex, posterior capsular rupture and vitreous loss occurred. Anterior vitrectomy clearance was carried out and a PMMA IOL was implanted in the sulcus (Supplementary video 1). The second surgery was uneventful and a folding acrylic lens was implanted in the bag. The cataract wound was closed with 10/0 nylon sutures in both cases.
In the third case, a type-2 BB5 (pre-Descemetic) was achieved. The BB extended to the periphery in one quadrant. The DM was bared and a sclerocorneal tunnel with side ports was fashioned. When viscoelastic was injected into the AC prior to capsulorhexis, the DM disinserted from its peripheral attachment and the AC collapsed (Supplementary video 2). Cataract surgery was abandoned and the corneal transplantation was completed as a penetrating graft.
All patients received routine postoperative management in the form of topical moxifloxacin six times a day and dexamethasone six times a day. The antibiotic medication was discontinued after 6 weeks and the steroid medication tapered to four times a day after 3 months, to twice a day after 6 months and discontinued after 1 year.
Results
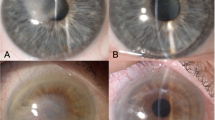
At the last follow up at 18 months, the first case of successful DALK-triple had a clear graft with BCVA of 6/12 and a residual astigmatism of two dioptres following the sequential removal of five sutures to treat astigmatism (Figure 1). The second case of successful DALK-triple, at the last follow up at 6 months had a clear graft with a BCVA of 6/12 (Figure 2). The third patient that was converted to a penetrating graft maintained a clear graft at the last follow up of 8 months, with a BCVA of 6/9 (Figure 3). No postoperative complications were noted. IOP was normal through the follow up period.
Discussion
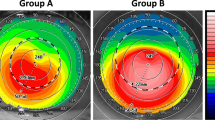
The pre-Descemet’s layer/DL that forms the posterior wall of the type-1 BB has certain distinct characteristics which set it apart from the rest of the posterior corneal stroma. Its thickness ranges from 6 to 15 microns; it is made up of 5–8 lamellae of collagen fibres; it is devoid of keratocytes and is impervious to air. In donor eyes from eye banks the bubble can be inflated to a pressure of around 700 mm Hg before it ruptures.5 Recent observations have demonstrated that it is also present in children (unpublished observations). Our observations from our studies and from a review of the literature5, 6, 7 indicate that keratocytes are not normally present in contact with the anterior surface of the DM. There is always an acellular zone between the anterior surface of the DM and the most posterior row of keratocytes. This is the zone that separates as DL when the stroma is inflated with air. Its strength accounts for the strength of eyes that have undergone DALK compared to PK and it also allows the surgeon to perform phacoemulsification, anterior vitrectomy and lens implant, without rupture. Though previous reports2, 4 have described a very similar procedure, they claim that they have bared DM by manual dissection or use of viscoelastic. We submit that they had actually performed the procedure with DL in situ. When we attempted to perform DALK under DM, confirmed by the formation of a type-2 BB, it did not withstand the pressure induced by injection of viscoelastic. We therefore recommend that phacoemulsification should be attempted with extreme caution or not at all with a type-2 BB but can be performed reasonably safely if DL is retained (type-1 BB).
The origin of the bubble at the centre and its centrifugal spread, the surrounding white ring, its diameter extending to no more than 8.5–9 mm and surface ‘roughness’ related to broken strands of collagen extending between DL and deep stroma, are signs of a type-1 BB.5 With a type-1 BB a gentle attempt at insertion of a blunt spatula directed radially towards the limbus, between the surface of DL and the deep stroma along the circumference of the trephine cut will be met with resistance but not so with a type-2 BB where the plane extends further towards or up to the limbus. However this manoeuvre is risky and should be attempted with caution. A type-2 BB expands very rapidly, starts at the periphery and spreads centrally covering an area much larger than the trephine mark, often to the periphery of the cornea as stated above. It has a very smooth surface with no ‘roughness’ as seen with a type-1 BB. These clues can help the surgeon to decide which type of BB has been achieved. We also recommend repeated paracentesis during DALK (with or without phacoemulsification), to reduce intraocular pressure and stress on the DM, especially with a type-2 BB. This will help to reduce risk of DM rupture and make the procedure safer. Furthermore, as has been demonstrated previously, the type-2 BB extends outwards to the periphery of the cornea.5, 8 The tip of the paracentesis needle or knife can easily rupture the bubble if it makes contact with the bubble wall. This can be avoided by making a very peripheral paracentesis with a type-2 BB prior to puncturing the roof of the bubble. Thereafter, once the air has escaped and the bubble has deflated, the paracentesis can be extended.
Another important observation is that even with dense corneal scars, DL remains transparent allowing good visibility through it. The lack or paucity of keratocytes and consequent lack of keratocyte activation and scar tissue formation may be an explanation for this. Retention of transparency in the presence of extensive stromal scarring is yet another feature of DL.
The disadvantage of this approach is that it is difficult to predict which type of BB will be achieved though some measures such as placing the needle/canula tip in deep stroma in the centre of the cornea help in achieving a type-1 BB. This approach also shares the inherent disadvantage of any one-stage procedure with regard to predictability of biometry. Inaccurate keratometry related to corneal changes pre-operatively or post-graft astigmatism can be avoided when the cataract surgery is performed after corneal transplantation and removal of all sutures. In our postoperative protocol, suture management of astigmatism (removal of sutures in the steep (semi) meridian) is carried out until a residual astigmatism of 2.5 D or less is obtained. Remaining sutures are not routinely removed to avoid risk of worsening astigmatism.

References
Greene JB, Mian SI . Cataract surgery in patients with corneal disease. Curr Opin Ophthalmol 2013; 24: 9–14.
Panda A, Sethi HS, Jain M, Nindra Krishna S, Gupta AK . Deep anterior lamellar keratoplasty with phacoemulsification. J Cataract Refract Surg 2011; 37: 122–126.
Senoo T . Combined surgery with deep lamellar keratoplasty. Semin Ophthalmol 2001; 16: 126–136.
Muraine MC, Collet A, Brasseur G . Deep lamellar keratoplasty combined with cataract surgery. Arch Ophthalmol 2002; 120: 812–815.
Dua HS, Faraj LA, Said DG, Gray T, Lowe J . Human corneal anatomy redefined: a novel pre-Descemet's layer (Dua's layer). Ophthalmology 2013; 120: 1778–1785.
Marshall J, Grindle CF . Fine structure of the cornea and its development. Trans Ophthalmol Soc UK 1978; 98: 320–328.
Dua HS, Faraj LA, Said DG, Gray T, Lowe J . “Dua’s Layer is not just residual Stroma” Author reply. Ophthalmology 2014; 121 (5): e25–e26.
Dua HS, Faraj LA, Said DG . Dua’s layer: its discovery, characteristics and clinical applications. Biomechanica y arquitetura corneal (corneal architecture and biomechanics). eds. Ángeles del Buey Sayas MA, Cristina Peris Martínez CP. Elsevier, 2014 Chapter 4 pp 35–47.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented 15th January 2014 in VIII Research Institute of Ophthalmology Silver Jubilee International Meeting, Cairo, Egypt.
Supplementary Information accompanies this paper on Eye website
Rights and permissions
About this article
Cite this article
Zaki, A., Elalfy, M., Said, D. et al. Deep anterior lamellar keratoplasty—triple procedure: a useful clinical application of the pre-Descemet’s layer (Dua’s layer). Eye 29, 323–326 (2015). https://doi.org/10.1038/eye.2014.273
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.273
This article is cited by
-
Refractive surgery after deep anterior lamellar keratoplasty: a review of the literature
International Ophthalmology (2022)
-
In vitro reconstructed 3D corneal tissue models for ocular toxicology and ophthalmic drug development
In Vitro Cellular & Developmental Biology - Animal (2021)