Abstract
Objectives
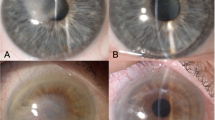
Visual and topographic outcomes of large (9.0 mm) versus conventional (8.0 mm) deep anterior lamellar keratoplasty (DALK) for the treatment of keratoconus (KC) were compared in relation to the different localization of the corneal ectasia (within or beyond the central 8.0 mm).
Methods
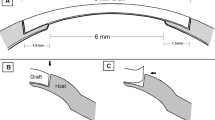
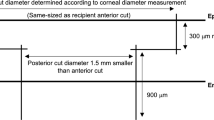
This is a retrospective, comparative case series. Preoperatively, the topographic extension of the conus was calculated by measuring the distance from the geometric center of the cornea and the outermost point of the corneal ectasia (ectasia <8.0 mm, group A; ectasia ≥8.0 mm, group B). DALK was performed using both small grafts (8.0 mm, group 1) and large grafts (9.0 mm, group 2). Best-corrected visual acuity and topographic astigmatism were evaluated preoperatively (T0) and postoperatively after complete suture removal (1 year, T1).
Results
Data from 224 eyes of 196 patients (mean age 37.6 ± 15.1 years) were evaluated. Topographic astigmatism improved from T0 to T1 (4.94 ± 2.92 diopters (D) [95% CI, 4.56–5.33] vs 4.19 ± 2.45 D [95% CI, 3.87–4.51], p = 0.001). There was no significant difference in postoperative topographic cylinder between group 1 and group 2 when considering eyes with corneal ectasia <8.0 mm (group 1 A, 4.15 ± 2.19 D [95% CI, 3.64–4.66] vs group 2 A, 3.65 ± 2.13 D [95% CI, 2.92–4.38], p = 0.14); conversely, the difference was significant considering eyes with corneal ectasia ≥8.0 mm (group 1B, 4.74 ± 2.90 D [95% CI, 4.09-5.38] vs group 2B, 3.68 ± 1.94 D [95% CI, 3.10–4.26], p = 0.02).
Conclusions
Large 9.0-mm DALK provided better anatomical outcomes compared to conventional 8.0-mm DALK, particularly in eyes with corneal ectasia extending beyond the central 8.0 mm.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data are available upon reasonable request.
References
Eye Bank Association of America. 2019 Eye Banking Statistical Report; 2020. Accessed 8 Dec 2022.
Arundhati A, Chew MC, Lim L, Mehta JS, Lang SS, Htoon HM, et al. Comparative study of long-term graft survival between penetrating keratoplasty and deep anterior lamellar keratoplasty. Am J Ophthalmol. 2021;224:207–16.
Henein C, Nanavaty MA. Systematic review comparing penetrating keratoplasty and deep anterior lamellar keratoplasty for management of keratoconus. Cont Lens Anterior Eye. 2017;40:3–14.
Chen G, Tzekov R, Li W, Jiang F, Mao S, Tong Y. Deep anterior lamellar keratoplasty versus penetrating keratoplasty: a meta-analysis of randomized controlled trials. Cornea. 2016;35:169–74.
Shams M, Sharifi A, Akbari Z, Maghsoudlou A, Tajali MR. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for keratoconus: a systematic review and meta-analysis. J Ophthalmic Vis Res. 2022;17:89–107.
Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty: a report by the American academy of ophthalmology. Ophthalmology. 2011;118:209–18.
Yu AC, Mattioli L, Busin M. Optimizing outcomes for keratoplasty in ectatic corneal disease. Curr Opin Ophthalmol. 2020;31:268–75.
Thanitcul C, Mathews P, Woreta FA, Akpek EK, Varadaraj V, Srikumaran D. Surgeon preference for keratoplasty techniques and barriers to performing deep anterior lamellar keratoplasty. Cornea. 2021;40:1406–12.
Anwar M, Teichmann KD. Big-bubble technique to bare Descemet’s membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28:398–403.
Knutsson KA, Rama P, Paganoni G. Modified big-bubble technique compared to manual dissection deep anterior lamellar keratoplasty in the treatment of keratoconus. Acta Ophthalmol. 2015;93:431–8.
Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol. 2007;143:117–24.e2.
Busin M, Leon P, Nahum Y, Scorcia V. Large (9 mm) deep anterior lamellar keratoplasty with clearance of a 6-mm optical zone optimizes outcomes of keratoconus surgery. Ophthalmology. 2017;124:1072–80.
Huang T, Hu Y, Gui M, Zhang H, Wang Y, Hou C. Large-diameter deep anterior lamellar keratoplasty for keratoconus: visual and refractive outcomes. Br J Ophthalmol. 2015;99:1196–200.
Lucisano A, Lionetti G, Yu AC, Giannaccare G, D’Angelo S, Busin M, et al. Outcomes of conventional 8.0-mm versus large 9.0-mm diameter deep anterior lamellar keratoplasty for keratoconus. Cornea. 2022. https://doi.org/10.1097/ICO.0000000000003082.
Bergmanson JPG, Goosey JD, Patel CK, Mathew JH. Recurrence or re-emergence of keratoconus-what is the evidence telling us? Literature review and two case reports. Ocul Surf. 2014;12:267–72.
Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre-descemet’s layer (Dua’s Layer). Ophthalmology. 2013;120:1778–85.
Goweida MBB. Intraoperative review of different bubble types formed during pneumodissection (Big-Bubble) deep anterior lamellar keratoplasty. Cornea. 2015;34:621–4.
Dua HS, Katamish T, Said DG, Faraj LA. Differentiating type 1 from type 2 big bubbles in deep anterior lamellar keratoplasty. Clin Ophthalmol. 2015;9:1155.
Seitz B, Langenbucher A, Küchle M, Naumann GOH. Impact of graft diameter on corneal power and the regularity of postkeratoplasty astigmatism before and after suture removal. Ophthalmology. 2003;110:2162–7.
Giannaccare G, Weiss JS, Sapigni L, Bovone C, Mattioli L, Campos EC, et al. Immunologic stromal rejection after deep anterior lamellar keratoplasty with grafts of a larger size (9 mm) for various stromal diseases. Cornea. 2018;37:967–72.
Scorcia V, Giannaccare G, Lucisano A, Soda M, Scalzo GC, Myerscough J, et al. Predictors of bubble formation and type obtained with pneumatic dissection during deep anterior lamellar keratoplasty in keratoconus. Am J Ophthalmol. 2020;212:127–33.
Author information
Authors and Affiliations
Contributions
Conceptualization, GG, AL, VS; Methodology, GG and AT; Validation, GG, VS and AL; Formal analysis, AL, AT, RG, CR; Investigation, GG, VS, AL, CR, RG and AT; Data curation, AT, RG and CR; Writing – original draft preparation, AT, RG, CR and GG; Writing – review & editing, AT, GG, AL, and VS; Visualization, AL, AT, VS, G.G., RG, CR; Supervision, GG, VS and AL; Project Administration, VS and GG All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
This study followed the tenets of the 2013 Declaration of Helsinki. The study was approved by the local ethics committee (Comitato Etico Area Centro, Regione Calabria - Protocol No. 150/22).
Informed consent statement
Written informed consent was obtained by all patients undergoing surgery.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lucisano, A., Scorcia, V., Taloni, A. et al. Impact of topographic localization of corneal ectasia on the outcomes of deep anterior lamellar keratoplasty employing large (9 mm) versus conventional diameter (8 mm) grafts. Eye 37, 3477–3483 (2023). https://doi.org/10.1038/s41433-023-02536-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02536-6