Abstract
Fuchs endothelial corneal dystrophy (FECD) is a well recognized corneal disorder characterized by the presence of collagenous warts extending from Descemet membrane (guttae) and endothelial cellular dysfunction due to cell loss and/or degeneration. Because of the characteristic abnormal cell morphology as seen with specular microscopy as well as the limited regenerative capacity in vivo, the endothelial cells were considered to be ‘dystrophic’. Hence, FECD is commonly managed by replacement of the endothelium with donor tissue by means of a penetrating or endothelial keratoplasty. The latter procedure has now been refined to the isolated transplantation of a donor Descemet membrane and its endothelium, referred to as Descemet membrane endothelial keratoplasty (DMEK). Unexpectedly, clinical observation made after DMEK seemed to challenge the current concept of the state of the endothelium in FECD; we actually observed an important role for the ‘dystrophic’ host endothelium in re-endothelialization of the denuded DM, and subsequent corneal clearance. In addition, recent studies regarding the pathophysiology of FECD made us realize that the endothelial cells are not ‘dystrophic’ per se, but in the course of time may have acquired a dysfunction instead. This paper describes the rationale behind this new concept and based on this, discusses the possibilities for future, less invasive treatment modalities for FECD.
Similar content being viewed by others
Introduction
Fuchs endothelial corneal dystrophy (FECD) is an endothelial cellular dysfunction due to cell loss and/or degeneration.1, 2 The disorder has four distinctive stages. In the early stages, visual acuity is reduced by ‘guttae’, that is, collagenous warts extending from the Descemet membrane that compromise the optical performance of the cornea.1, 2 In the advanced stages, the cornea shows edema as a result of reduced endothelial pump function.2, 3, 4, 5, 6 This entity was first recognized by Dr Ernst Fuchs in the early 1900s, with the sole availability of a candle light illuminated slit-lamp. The function of the endothelium was not yet known, and as the condition seemed irreversible, the cornea was considered to be ‘dystrophic.’ The condition was first described to be an ‘epithelial dystrophy’, and the term later evolved to a ‘combined dystrophy’ and ‘endothelial dystrophy’. The overall clinical picture seemed to fit into the definition of the term ‘corneal dystrophy’, first used to refer to ‘a group of inherited corneal diseases that are typical bilateral, symmetric, slowly progressive, and without relationship to environmental or systemic factors’.7
However, we would like to challenge this concept; in our opinion, the endothelial cells are not ‘dystrophic’ per se, but in most cases may have acquired a dysfunction instead. This idea is based on recent clinical observations showing the important role of the ‘dystrophic’ host endothelium in corneal clearance after endothelial keratoplasty,8, 9, 10 and current knowledge regarding the pathophysiology of FECD.11, 12 More detailed knowledge of FECD etiology might even open the door to the development of new, less invasive treatment modalities, and have far reaching consequences for patients, corneal surgeons, and eye banks.
Methodology: PubMed and Google Scholar were used to search the literature. The main search terms used were: ‘Corneal dystrophy’, ‘Fuchs endothelial dystrophy’, ‘Pathophysiology AND Fuchs endothelial dystrophy’, ‘Gene AND Fuchs endothelial dystrophy’, ‘Oxidative stress AND Fuchs endothelial dystrophy’, ‘Keratoplasty’, ‘Endothelial keratoplasty’, ‘Descemet Membrane Endothelial Keratoplasty’, ‘Wound healing AND corneal endothelium’, ‘Regeneration AND corneal endothelium’, ‘Migration AND corneal endothelium’, ‘Culture AND corneal endothelium’, Stem cells AND corneal endothelium’, ‘Spontaneous clearance AND keratoplasty’, ‘Donor endothelial cells AND keratoplasty’, ‘Recipient AND Host AND endothelial cells AND keratoplasty’.
Clinical observations after Descemet membrane endothelial keratoplasty suggesting a role for the ‘dystrophic’ recipient endothelium in corneal clearance
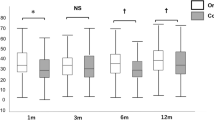
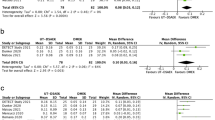
Corneal endothelial cells are considered to be ‘dystrophic’ and have limited to no regenerative capacity in vivo.3, 6, 13 Therefore, replacing the diseased endothelium with healthy donor tissue through a penetrating or endothelial keratoplasty is generally accepted as the only effective treatment option for FECD.14 With the evolution of endothelial keratoplasty, the procedure has been refined to isolated transplantation of a donor Descemet membrane and its endothelium. This procedure is known as ‘Descemet membrane endothelial keratoplasty’ (DMEK).14, 15, 16 Clinical observations made after DMEK8, 9, 10 quite unexpectedly led us to reconsider the presumption that FECD is an irreversible pathological condition owing to ‘dystrophic’ endothelial cells. In DMEK eyes, a more rapid clearance was seen in the corneal periphery than in the central cornea overlying the transplant.9 Also, in DMEK eyes with an eccentrically positioned or a partially detached transplant, the area between the edge of the descemetorhexis and the edge of the transplant often showed faster clearance than the area over the transplant. This observation held true even if the transplant edge showed an outward roll, potentially ‘blocking’ donor endothelial cell migration toward the peripheral host cornea.8, 9 The most striking observation was seen in DMEK eyes complicated by complete detachment of the donor Descemet graft, where the cornea still cleared in the majority of cases.9 In other words, the recipient bare posterior stroma (denuded after descemetorhexis) was somehow re-endothelialized.10
This ‘spontaneous clearance’ of the host cornea was observed only when the indication for surgery was FECD, whereas no improvement was seen in eyes operated on for bullous keratopathy.10 This suggests that corneal clearance depended on the underlying pathogenesis responsible for the endothelial dysfunction, which may be explained by the host peripheral endothelium having a significant role in the early repopulation of the denuded recipient posterior stroma. However, the presence of a donor graft may be mandatory for the migration of a recipient peripheral endothelium over denuded posterior stroma, as it appeared to be completely absent in a patient in whom a DMEK procedure was interrupted after making the descemetorhexis (ie, without graft implantation),9 and only partly successful in a nonrandomized, prospective clinical study, where patients underwent a descemetorhexis without endothelial keratoplasty.17 These data suggest that the term ‘dystrophy’ may in fact be misleading, because it defines an irreversible cellular pathology, whereas the clinically observed endothelial wound healing patterns seems to prove the opposite; this is a reversible condition, where the host corneal endothelium is capable of restoring its normal mosaic on the bare stroma after removal of the pathologically altered Descemet membrane.
How can these findings be explained? To answer this question we need to look into what is currently known about the pathophysiology of FECD and wound healing patterns of the normal and FECD corneal endothelium (Figure 1).
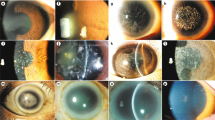
Wound healing response and regenerative potential of recipient endothelial cells of normal and FECD corneas. Here, ultraviolet (UV) radiation is taken as an example to demonstrate the wound healing response of normal and FECD corneal endothelium to oxidative stress-induced damage and apoptosis. As the central cornea is thinner in comparison with the peripheral cornea, it is suggested that UV radiation has its most damaging effects (in the form of oxidative stress) on the central endothelial cells, whereas the peripheral endothelial cells are protected from oxidative stress-induced damage (a, d). Although cells have several defense mechanisms against short-time exposure to oxidative stress, during prolonged exposure, the damage which cannot be repaired will accumulate, and consequently, the cell dies by apoptosis. In the case of corneal endothelium, this leaves a gap between the rest of the endothelial cells, which might compromise the endothelial pump and cause stromal swelling. In the normal cornea (b, c), this defect is supposedly covered by the centripetal migration of stem-like cells in the periphery (arrows in b) which, during migration to the center of the cornea, become mature endothelial cells, dedicated to keep the cornea thin and transparent. However, in FECD corneas (e), the central endothelial cells are even more susceptible to UV-induced damage, resulting in a higher number of apoptotic cells and more gaps between cells. Here, the defect cannot be covered by the peripheral stem-like cells because of the physical barrier in the form of guttae (black structures). Therefore, the adjacent endothelial cells need to stretch to cover the gap the lost cell has created. Eventually, as the guttae progress and coalesce, these cells are also lost, and the cornea decompensates and requires a keratoplasty procedure to restore normal vision (f). When DMEK is performed, the barrier in the form of guttae is removed by the descemetorhexis, and when the graft (green) is implanted, the peripheral stem-like cells are again able to migrate to the center (arrows) (g). In the end, the endothelial pump is restored and the cornea becomes thin and transparent again. In due time, as the centripetal migration of recipient stem-like cells continues, they may mix among the donor cells (green) (h).
Pathophysiology of FECD
Although not much is known about the pathological mechanism behind FECD, it is suspected that genetic mutations and environmental factors, and possibly their interactions,11, 12 lie at the root of the disease. When we take a look at what is currently known about the genetic background of FECD, mutated genes have only been found in inherited cases and some sporadic cases. For instance, FECD has been associated with rare mutations in SLC4A11 (solute carrier family 4, sodium borate transporter, member 11),18, 19 TCF4 (transcription factor 4),20, 21, 22, 23, 24, 25 TCF8 (transcription factor 8),26, 27 CLU (clusterin),24 and LOXHD1 (lipoxygenase homology domains 1).28 These mutations, however, are not identified in every cohort of FECD patients.29, 30 In addition to mutations in known genes, linkage studies have identified mutations in chromosomal loci such as in chromosome 5 (FCD3),31 9 (FCD4),27 13 (FCD1),32 18 (FCD 2),33 and potential linkages at chromosome 1, 7, 15, 17, and X,20 of which the specific mutated genes have not been identified yet. Some of these mutations have also been identified in other types of endothelial dystrophy; the SLC4A11 mutation has also been identified in congenital hereditary endothelial dystrophy34, 35 and perceptive deafness (Harboyan syndrome),36 and mutations in TCF8 have also been identified in posterior polymorphous corneal dystrophy.37, 38 This suggests that corneal endothelial dystrophies may not be separate diseases, but may represent a phenotypic continuum with a significant genetic overlap, despite discrete clinical manifestations.27
However, in most cases, FECD is not associated with a specific genetic mutation, but may rather be due to an impaired defense to environmental factors, such as oxidative stress.39 The major inducers of oxidative stress in the cornea are ultraviolet radiation, temperature changes, and aqueous humor soluble factors (Figure 1).40, 41, 42 Corneal endothelial cells are thought to be especially vulnerable to oxidative stress-induced damage because they do not proliferate and have a high level of metabolic activity owing to their pump function.39, 43 Fortunately, these cells have several defense mechanisms against the detrimental effects of oxidative stress,44, 45 thereby reducing damage and promoting cell survival. However, if oxidative stress persists, the defense mechanisms fail, thereby allowing the cell to accumulate damage. As a preventive measure, the cell becomes senescent or, in cases of severe damage, dies by apoptosis.44 Interestingly, several authors have found evidence of increased apoptosis having a role in endothelial cell loss, as observed in FECD.46, 47 Furthermore, it was shown that the defense mechanism of FECD endothelium against oxidative stress-induced damage is impaired when compared with normal cells,39, 45, 48, 49 which is supported by the observed significant higher levels of (baseline) oxidative stress-induced damage,43, 45, 48 and changes in endothelial cell morphology characteristic for oxidative stress.50 These data suggest that chronic oxidative stress contributes to the pathophysiology of FECD, and that the decreased defense system renders FECD endothelial cells even more susceptible to oxidative stress-induced damage than normal cells already are. It is to be noted that the corneal center is the site where oxidative stress is probably most prominent.40 This might explain why FECD initiates in the corneal center, as endothelial cells in this area are exposed to the highest levels of oxidative stress-induced damage. Whether or not oxidative stress is also responsible for the early induction of guttae remains to be determined. However, this theory would agree with aberrant protein expression, which is one of the consequences of oxidative stress-induced damage.51
Wound healing patterns of the normal and FECD corneal endothelium
Until recently it was thought (as endothelial cells were believed to have no regenerative potential) that when a corneal cell is ‘lost’, it induces a wound healing response where the defect of the lost cell is covered by an adjacent endothelial cell through migration and elongation.13 However, a recent study by He et al,40 suggested that the corneal periphery contains a reservoir of stem-like cells that replace damaged or dead endothelium by continuous centripetal migration patterns (Figures 1b and c). These stem-like cells are supposedly shielded from oxidative stress-induced damage because of their specific location at the very edge of the posterior cornea.40 However, upon migration to the center of the cornea, the stem-like cells are exposed to oxidative stress, which induces their maturation to end-stage corneal endothelial cells, dedicated to keep the cornea in a deturgescent state.40 This wound healing mechanism could be impaired in FECD due to the presence of guttae, which act as a physical barrier to the centripetal migration of these peripheral stem-like cells (Figure 1e). Consequently, as in FECD the central cornea is depleted of endothelial cells due to an accumulation of oxidative stress-induced damage, the only wound healing response comes from the adjacent endothelial cells, which have to stretch and elongate to cover the defect and maintain the endothelial pump. As guttae develop, these attempts at wound healing are even further impaired. This may lead to a vicious cycle, where the cells covering the bare area are also damaged and lost. Eventually, too few cells are left to maintain the endothelial pump. This results in corneal decompensation and requires a keratoplasty procedure to restore normal vision (Figure 1f).
Possible mechanisms behind corneal clearance after DMEK
How does the above explain the before-mentioned clinical observations that suggest recipient endothelial migration after DMEK? Given the above, removing the physical barrier (guttae) by means of a penetrating or endothelial keratoplasty may enable the peripheral stem-like cells to freely migrate again and to mix among the donor cells (Figures 1g and h).52, 53, 54 This might also explain the longer survival of corneal grafts in patients with high ECD in the corneal periphery,55, 56 the more rapid clearance in the corneal periphery than in the central cornea after DMEK,9 and the faster clearance over the gap between the edge of the descemetorhexis and the edge of the transplant than over the transplant itself.8, 9 In case of ‘spontaneous clearance’, a similar mechanism might have taken place where by removing the barrier (guttae), the peripheral stem-like cells are once again able to cover the denuded stroma by migrating to the corneal center (Figures 2a–c). Thus, the above mentioned studies indicate that in FECD, the endothelial cells are not necessarily ‘dystrophic’. This is further substantiated by a recent publication showing that among the ‘dysfunctional’ FECD endothelial cells, endothelial cells with regenerative potential exist.57
Mechanisms behind spontaneous clearance and a sole descemetorhexis in the management of FECD. In the case of spontaneous clearance, it is thought that the donor graft somehow induces recipient endothelial migration. By removing the guttae that act as barriers to the migration of peripheral stem-like cells (a) and inserting a free-floating donor tissue (green) (only attached to the incision for stable positioning), clinical observations indicate that migration of the recipient stem-like cells is induced (b). Consequently, the bare stroma is covered by recipient endothelial cells (c), the endothelial pump is restored, and the cornea is returned to its deturgescent state. Alternatively, in some cases, a descemetorhexis, without the concomitant transplantation of donor tissue, might be sufficient to induce recipient endothelial migration (d–f). One of the prerequisites for success is the early detection of the disease, when the guttae have not progressed to the far periphery yet, and sufficient peripheral stem-like cells remain to cover the bare stroma (d). After removal of the physical barrier by means of the descemetorhexis, proliferation and migration of the peripheral stem-like cells may be initiated (e), resulting in a restoration of the normal endothelial mosaic and pump function, thus a thin and transparent cornea.
Future perspectives
If this proves correct, it may open the door to also reconsider the current keratoplasty management of FECD, which is the same for all variants. In the future, tailored treatment options may be developed based on the different variants of FECD. However, before we enter this exciting era, a lot of questions need to be answered. First and foremost, the different disorders now all recognized as FECD need to be identified individually, and it should be assessed to what extent genetic mutations and environmental factors are involved in disease onset, severity, and progression. For instance, although the prevalence of the TCF4 mutation is low, it is associated with a very high risk of developing FECD. Other examples include loss-of-function mutations in TCF8, that can interact with FCD4 to modulate FECD severity,27 and FCD3 mutations presenting clinically with milder phenotypes than FCD1 and FCD2.31 This implies that genetic mutations, whether alone or in concert with other factors, may be used to identify risk of developing disease or act as prognostic factors to determine disease severity and progression.58
Another important question is whether in the different FECD variants, all endothelial cells are affected by the disorder or whether in some a mosaic of non-affected and affected cells exists? Furthermore, the question arises whether a keratoplasty procedure, as it is currently performed, will still be required to restore vision in all of these different variants? Perhaps in some cases, where endothelial cell loss is mainly due to apoptosis, drugs that inhibit apoptosis may be able to delay or even halt FECD progression.46 One of the biggest challenges in this approach is identifying the disease in a sufficiently early stage, where the intervention still has an effect.
In addition, it needs to be determined what potential contribution the recipient endothelium has in restoring the cellular monolayer across the cornea, and whether the presence of donor tissue is really mandatory for the migration of recipient endothelial cells. If the recipient endothelial cells are able to repair the defect independently of donor tissue, the surgical treatment may be directed toward removing the Descemet membrane and its guttae rather than transplanting donor endothelium (Figures 2d–f). Apparently, just the removal of Descemet membrane could already be effective to obtain corneal clearance in some cases, however, these results may not be consistent.9, 17
If, on the other hand, recipient peripheral endothelial cells do need to be stimulated toward migratory and/or regenerative activity by the donor tissue, a central descemetorhexis in combination with free-floating donor tissue, also known as ‘Descemet membrane endothelial transfer’ (DMET),10 might be effective in restoring vision (Figures 2a–c). Alternatively, the transplantation of cultured donor-derived corneal endothelial cells or differentiated stem cells59 may be future options. These cells could be attached to a Descemet membrane-like biomatrix59 or injected as single cells into the anterior chamber together with an adjuvant, inducing their attachment to the bare stroma.60, 61, 62 The latter strategies could also significantly reduce the need for donor tissue, allowing an even larger group of patients to be treated.
Concluding remarks
Minimizing surgical intervention to treat FECD would greatly benefit patients, corneal surgeons, and eye banks. For patients, the visual prognosis would probably be better, as physiological repopulation and near-perfect anatomical restoration by host cells may prove superior to any currently available keratoplasty procedure. For corneal surgeons, the entire management of corneal endothelial disorders would become less challenging with a reduced risk of graft detachments and other complications. For eye banks, the requests for tissue could shift toward isolated donor Descemet implants and/or cell culture, allowing a far more efficient use of donor tissue. In the end, we may even come to understand that conventional and/or endothelial keratoplasty were just scientific side-steps in the management of FECD. The regenerative capacities of our tissues may yet prove to be the most forgiving compared with all current surgical approaches. In the end, it may be Mother Nature, not the corneal surgeon that does a better repair job.
References
Fuchs E . Dystrophia epithelialis corneae. Graefes Arch Ophthalmol 1910; 76: 478–508.
Wilson SE, Bourne WM . Fuchs’ dystrophy. Cornea 1988; 7: 2–18.
Bergmanson JP, Sheldon TM, Goosey JD . Fuchs’ endothelial dystrophy: a fresh look at an aging disease. Ophthalmic Physiol Opt 1999; 19: 210–222.
Adamis AP, Filatov V, Tripathi BJ, Tripathi RC . Fuchs’ endothelial dystrophy of the cornea. Surv Ophthalmol 1993; 38: 149–168.
Borboli S, Colby K . Mechanisms of disease: Fuchs’ endothelial dystrophy. Ophthalmol Clin North Am 2002; 15: 17–25.
Ing JJ, Ing HH, Nelson LR, Hodge DO, Bourne WM . Ten-year postoperative results of penetrating keratoplasty. Ophthalmology 1998; 105: 1855–1865.
Weiss JS, Møller HU, Lisch W, Kinoshita S, Aldave AJ, Belin MW et al. The IC3D classification of the corneal dystrophies. Cornea 2008; 27: S1–S83.
Balachandran C, Ham L, Verschoor CA, Ong TS, van der Wees J, Melles GRJ . Spontaneous corneal clearance despite graft detachment in Descemet membrane endothelial keratoplasty (DMEK). Am J Ophthalmol 2009; 148: 227–234.
Dirisamer M, Dapena I, Ham L, van Dijk K, Oganes O, Frank LE et al. Patterns of endothelialization and corneal clearance after Descemet membrane endothelial keratoplasty for Fuchs endothelial dystrophy. Am J Ophthalmol 2011; 152: 543–555.
Dirisamer M, Yeh RY, van Dijk K, Ham L, Dapena I, Melles GRJ . Recipient endothelium may relate to corneal clearance in Descemet membrane endothelial transfer. Am J Ophthalmol 2012; 154: 290–296.
Schmedt T, Silva MM, Ziaei A, Jurkunas U . Molecular bases of corneal endothelial dystrophies. Exp Eye Res 2012; 95: 24–34.
Elhalis H, Azizi B, Jurkunas UV . Fuchs endothelial corneal dystrophy. Ocul Surf 2010; 8: 173–184.
Olsen EG, Davanger M . The healing of human corneal endothelium. An in-vitro study. Acta Ophthalmol (Copenh) 1984; 62: 885–892.
Melles GRJ . Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea 2006; 25: 879–881.
Guerra FP, Anshu A, Price MO, Giebel AW, Price FW . Descemet’s membrane endothelial keratoplasty prospective study of a 1-year visual outcomes, graft survival, and endothelial cell loss. Ophthalmology 2011; 118: 2368–2373.
Dirisamer M, Ham L, Dapena I, Moutsouris K, Droutsas K, van Dijk K et al. Efficacy of Descemet membrane endothelial keratoplasty—Clinical outcome of 200 consecutive cases after a learning curve of 25 cases. Arch Ophthalmol 2011; 129: 1435–1443.
Bleyen I, Saelens IE, van Dooren BT, van Rij G . Spontaneous corneal clearing after Descemet’s stripping. Ophthalmology 2013; 120: 215.
Vithana EN, Morgan PE, Ramprasad V, Tan DT, Yong VH, Venkataraman D et al. SLC4A11 mutations in Fuchs endothelial corneal dystrophy. Hum Mol Genet 2008; 17: 656–666.
Riazuddin SA, Vithana EN, Seet LF, Liu Y, Al-Saif A, Koh LW et al. Missense mutations in the sodium borate cotransporter SLC4A11 cause late-onset Fuchs corneal dystrophy. Hum Mutat 2010; 31: 1261–1268.
Baratz KH, Tosakulwong N, Ryu E, Brown WL, Branham K, Chen W et al. E2-2 protein and Fuchs’s corneal dystrophy. N Engl J Med 2010; 363: 1016–1024.
Li YJ, Minear MA, Rimmler J, Zhao B, Balajonda E, Hauser MA et al. Replication of TCF4 through association and linkage studies in late-onset Fuchs endothelial corneal dystrophy. PLoS One 2011; 6: e18044.
Thalamuthu A, Khor CC, Venkataraman D, Koh LW, Tan DT, Aung T et al. Association of TCF4 gene polymorphisms with Fuchs’ corneal dystrophy in the Chinese. Invest Ophthalmol Vis Sci 2011; 52: 5573–5578.
Stamler JF, Roos BR, Wagoner MD, Goins KM, Kitzmann AS, Riley JB et al. Confirmation of the association between the TCF4 risk allele and Fuchs endothelial corneal dystrophy in patients from the Midwestern United States. Ophthalmic Genet 2013; 34: 32–34.
Kuot A, Hewitt AW, Griggs K, Klebe S, Mills R, Jhanji V et al. Association of TCF4 and CLU polymorphisms with Fuchs’ endothelial dystrophy and implication of CLU and TGFBI proteins in the disease process. Eur J Hum Genet 2012; 20: 632–638.
Wieben ED, Aleff RA, Tosakulwong N, Butz ML, Highsmith WE, Edwards AO et al. A common trinucleotide repeat expansion within the transcription factor 4 (TCF4, E2-2) gene predicts Fuchs corneal dystrophy. PLoS One 2012; 7: e49083.
Mehta JS, Vithana EN, Tan DT, Yong VH, Yam GH, Law RW et al. Analysis of the posterior polymorphous corneal dystrophy 3 gene, TCF8, in late-onset Fuchs endothelial corneal dystrophy. Invest Ophthalmol Vis Sci 2008; 49: 184–188.
Riazuddin SA, Zaghloul NA, Al-Saif A, Davey L, Diplas BH, Meadows DN et al. Missense mutations in TCF8 cause late-onset Fuchs corneal dystrophy and interact with FCD4 on chromosome 9p. Am J Hum Genet 2010; 86: 45–53.
Riazuddin SA, Parker DS, McGlumphy EJ, Oh EC, Iliff BW, Schmedt T et al. Mutations in LOXHD1, a recessive-deafness locus, cause dominant late-onset Fuchs corneal dystrophy. Am J Hum Genet 2012; 90: 533–539.
Hemadevi B, Srinivasan M, Arunkumar J, Prajna NV, Sundaresan P . Genetic analysis of patients with Fuchs endothelial corneal dystrophy in India. BMC Ophthalmol 2010; 10: 3.
Riazuddin SA, McGlumphy EJ, Yeo WS, Wang J, Katsanis N, Gottsch JD . Replication of the TCF4 intronic variant in late-onset Fuchs corneal dystrophy and evidence of independence from the FCD2 locus. Invest Ophthalmol Vis Sci 2011; 52: 2825–2859.
Riazuddin SA, Eghrari AO, Al-Saif A, Davey L, Meadows DN, Katsanis N et al. Linkage of a mild late-onset phenotype of Fuchs corneal dystrophy to a novel locus at 5q33.1-q35.2. Invest Ophthalmol Vis Sci 2009; 50: 5667–5671.
Sundin OH, Jun AS, Broman KW, Liu SH, Sheehan SE, Vito EC et al. Linkage of late-onset Fuchs corneal dystrophy to a novel locus at 13pTel-13q12.13. Invest Ophthalmol Vis Sci 2006; 47: 140–145.
Sundin OH, Broman KW, Chang HH, Vito EC, Stark WJ, Gottsch JD . A common locus for late-onset Fuchs corneal dystrophy maps to 18q21.2-q21.32. Invest Ophthalmol Vis Sci 2006; 47: 3919–3926.
Vithana EN, Morgan P, Sundaresan P, Ebenezer ND, Tan DT, Mohamed MD et al. Mutations in sodium-borate cotransporter SLC4A11 cause recessive congenital hereditary endothelial dystrophy (CHED2). Nat Genet 2006; 38: 755–757.
Paliwal P, Sharma A, Tandon R, Sharma N, Titiyal JS, Sen S et al. Congenital hereditary endothelial dystrophy—mutation analysis of SLC4A11 and genotype-phenotype correlation in a North Indian patient cohort. Mol Vis 2010; 16: 2955–2963.
Desir J, Moya G, Reish O, Van Regemorter N, Deconinck H, David KL et al. Borate transporter SLC4A11 mutations cause both Harboyan syndrome and non-syndromic corneal endothelial dystrophy. J Med Genet 2007; 44: 322–326.
Krafchak CM, Pawar H, Moroi SE, Sugar A, Lichter PR, Mackey DA et al. Mutations in TCF8 cause posterior polymorphous corneal dystrophy and ectopic expression of COL4A3 by corneal endothelial cells. Am J Hum Genet 2005; 77: 694–708.
Aldave AJ, Yellore VS, Yu F, Bourla N, Sonmez B, Salem AK et al. Posterior polymorphous corneal dystrophy is associated with TCF8 gene mutations and abdominal hernia. Am J Med Genet A 2007; 143A: 2549–2556.
Buddi R, Lin B, Atilano SR, Zorapapel NC, Kenney MC, Brown DJ . Evidence of oxidative stress in human corneal diseases. J Histochem Cytochem 2002; 50: 341–351.
He Z, Campolmi N, Gain P, Ha Thi BM, Dumollard JM, Duband S et al. Revisited microanatomy of the corneal endothelial periphery: new evidence for continuous centripetal migration of endothelial cells in humans. Stem Cells 2012; 30: 2523–2534.
Joyce NC, Zhu CC, Harris DL . Relationship among oxidative stress, DNA damage, and proliferative capacity in human corneal endothelium. Invest Ophthalmol Vis Sci 2009; 50: 2116–2122.
Zhu C, Rawe I, Joyce NC . Differential protein expression in human corneal endothelial cells cultured from young and older donors. Mol Vis 2008; 14: 1805–1814.
Czarny P, Kasprzak E, Wielgorski M, Udziela M, Markiewicz B, Blasiak J et al. DNA damage and repair in Fuchs endothelial corneal dystrophy. Mol Biol Rep 2013; 40: 2977–2983.
Fridman JS, Lowe SW . Control of apoptosis by p53. Oncogene 2003; 22: 9030–9040.
Jurkunas UV, Bitar MS, Funaki T, Azizi B . Evidence of oxidative stress in the pathogenesis of fuchs endothelial corneal dystrophy. Am J Pathol 2010; 177: 2278–2289.
Borderie VM, Baudrimont M, Vallée A, Ereau TL, Gray F, Laroche L . Corneal endothelial cell apoptosis in patients with Fuchs’ dystrophy. Invest Ophthalmol Vis Sci 2000; 41: 2501–2505.
Li QJ, Ashraf MF, Shen DF, Green WR, Stark WJ, Chan CC et al. The role of apoptosis in the pathogenesis of Fuchs endothelial dystrophy of the cornea. Arch Ophthalmol 2001; 119: 1597–1604.
Azizi B, Ziaei A, Fuchsluger T, Schmedt T, Chen Y, Jurkunas UV . p53-regulated increase in oxidative-stress-induced apoptosis in Fuchs endothelial corneal dystrophy: a native tissue model. Invest Ophthalmol Vis Sci 2011; 52: 9291–9297.
Bitar MS, Liu C, Ziaei A, Chen Y, Schmedt T, Jurkunas UV . Decline in DJ-1 and decreased nuclear translocation of Nrf2 in Fuchs endothelial corneal dystrophy. Invest Ophthalmol Vis Sci 2012; 53: 5806–5813.
Wang Z, Handa JT, Green WR, Stark WJ, Weinberg RS, Jun AS . Advanced glycation end products and receptors in Fuchs’ dystrophy corneas undergoing Descemet’s stripping with endothelial keratoplasty. Ophthalmology 2007; 114: 1453–1460.
Engler C, Kelliher C, Spitze AR, Speck CL, Eberhart CG, Jun AS . Unfolded protein response in fuchs endothelial corneal dystrophy: a unifying pathogenic pathway? Am J Ophthalmol 2010; 149: 194–202.
Wollensak G, Green WR . Analysis of sex-mismatched human corneal transplants by fluorescence in situ hybridization of the sex-chromosomes. Exp Eye Res 1999; 68: 341–346.
Lagali N, Stenevi U, Claesson M, Fagerholm P, Hanson C, Weijdegård B et al. Survival of donor-derived cells in human corneal transplants. Invest Ophthalmol Vis Sci 2009; 50: 2673–2678.
Lagali N, Stenevi U, Claesson M, Fagerholm P, Hanson C, Weijdegård B et al. Donor and recipient endothelial cell population of the transplanted human cornea: a two-dimensional imaging study. Invest Ophthalmol Vis Sci 2010; 5: 1898–1904.
Thompson RW Jr, Price MO, Bowers PJ, Price FW Jr . Long-term graft survival after penetrating keratoplasty. Ophthalmology 2003; 110: 1396–1402.
Williams KA, Coster DJ . The immunobiology of corneal transplantation. Transplantation 2007; 84: 806–813.
Zaniolo K, Bostan C, Rochette Drouin O, Deschambeault A, Perron MC, Brunette I et al. Culture of human corneal endothelial cells isolated from corneas with Fuchs endothelial corneal dystrophy. Exp Eye Res 2012; 94: 22–31.
Igo RP Jr, Kopplin LJ, Joseph P, Truitt B, Fondran J, Bardenstein D et al. Differing roles for TCF4 and COL8A2 in central corneal thickness and fuchs endothelial corneal dystrophy. PLoS One 2012; 7: e46742.
Zavala J, López Jaime GR, Rodríguez Barrientos CA, Valdez-Garcia J . Corneal endothelium: developmental strategies for regeneration. Eye (Lond) 2013; 27: 579–588.
Okumura N, Koizumi N, Ueno M, Sakamoto Y, Takahashi H, Hirata K et al. Enhancement of corneal endothelium wound healing by Rho-associated kinase (ROCK) inhibitor eye drops. Br J Ophthalmol 2011; 95: 1006–1009.
Okumura N, Koizumi N, Ueno M, Sakamoto Y, Takahashi H, Tsuchiya H et al. ROCK inhibitor converts corneal endothelial cells into a phenotype capable of regenerating in vivo endothelial tissue. Am J Pathol 2012; 181: 268–277.
Okumura N, Koizumi N, Kay EP, Ueno M, Sakamoto Y, Nakamura S et al. The ROCK inhibitor eye drop accelerates corneal endothelium wound healing. Invest Ophthalmol Vis Sci 2013; 54: 2493–2502.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
GRJ Melles is a consultant for DORC International BV/Dutch Ophthalmic USA. M Bruinsma and CM Tong declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bruinsma, M., Tong, C. & Melles, G. What does the future hold for the treatment of Fuchs endothelial dystrophy; will ‘keratoplasty’ still be a valid procedure?. Eye 27, 1115–1122 (2013). https://doi.org/10.1038/eye.2013.153
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.153