Abstract
Purpose
Corneal graft rejection is the most common reason for the failure of an allograft corneal transplant. We undertook this study to identify and compare risk factors and treatment outcomes for early and late corneal graft rejections after optical penetrating keratoplasty.
Methods
A retrospective case file analysis of 880 primary penetrating keratoplasties was performed at a tertiary ophthalmic care centre. Patients were divided into early rejectors (rejection episode within 6 months postoperatively) and late rejectors (rejection episode after 6 months postoperatively). Main parameters evaluated were demographics, preoperative diagnosis and clinical signs, donor tissue details, surgical technique, details of rejection episode, treatment, and outcome information.
Results
A total of 156 patients with rejection episodes were identified. Of these, 42 (26.9%) patients experienced early rejection episodes and 114 (73.1%) patients experienced late rejection episodes. Preoperative donor and recipient characteristics, surgical technique, and clinical presentation of graft rejection were found to be similar between both groups after a Bonferroni correction was applied (P>0.005). Treatment outcomes of graft rejections were not significantly different (P=0.46) between early and late rejectors, with 83% of patients responding to rejection treatment (80% early rejectors; 85% late rejectors).
Conclusion
Patients with early and late graft rejection have similar characteristics and both groups respond to treatment equally.
Similar content being viewed by others
Introduction
Graft rejection is the most common cause of corneal graft failure in which the host's immune system actively destroys the donor tissue.1, 2, 3 Several studies have identified risk factors for rejection, such as corneal neovascularisation, presence of herpetic eye disease, and repeat corneal grafting.1, 2, 4, 5, 6, 7, 8, 9, 10 Whilst there is extensive literature identifying risk factors for corneal graft rejection, there is limited data looking at the timing of these rejection episodes. It is currently not known whether the risks for corneal graft rejection in the early postoperative period are different compared with late rejection. If a patient could be identified as at increased risk for graft rejection at a particular point in time, then postoperative care could be modified to increase the chance of graft survival.
The aim of this study was therefore to identify and compare risk factors and treatment outcomes associated with early and late corneal graft rejections.
Materials and methods
A retrospective file review of hospital medical records identified all patients who underwent a penetrating keratoplasty between 1991 and 2006 at the Royal Victorian Eye and Ear Hospital, Melbourne. Operations were performed by various corneal surgeons of differing experience throughout the investigative period. The files were perused for evidence of corneal graft rejection and cases of optical PK involving corneal graft rejection were analysed. Patients were divided into early rejectors (rejection episode within 6 months postoperatively) and late rejectors (rejection episode after 6 months postoperatively). Only data from the first rejection episode in either eye was used in the analysis, so as to reduce bias from patients with multiple rejection episodes.
The exclusion criteria were patients <18 years of age (at the time of surgery), those with non-penetrating forms of keratoplasty, therapeutic or tectonic keratoplasty, patients with a second or subsequent keratoplasty, patients with incomplete scheduled follow-ups, and those who were not followed up at the same centre. Also, we chose to exclude hot grafts where the risk of rejection is inherently high, such as active, chemical injuries and corneal perforations. Graft rejection was defined as any episode involving the presence of combination of any of the following: (a) oedema in a previously clear graft, (b) presence of keratic precipitates (KP), (c) presence of an epithelial or endothelial rejection line, and (d) presence of cells and flare in the anterior chamber (AC); a definition, which is consistent with current literature.3 Patients with corneal oedema alone in the absence of other inflammatory signs were excluded to avoid potential cases of graft failure. Treatment of a graft rejection episode was considered successful if there was a decrease in steroid medication, combined with decline in (a) corneal oedema, (b) AC activity, and (c) epithelial or endothelial lines, for two or more consecutive follow-up appointments. Demographics, preoperative clinical profile, donor tissue details, surgical details of PK, details of rejection episode, treatment, and outcome of rejection episode were extracted from patients’ files. Ethical approval was obtained from the Human Research and Ethics Committee at the Royal Victorian Eye and Ear Hospital for this retrospective review, which was conducted in accordance with the Declaration of Helsinki.
Statistical analyses
Patients were categorised as early rejector or late rejector to identify differences between the two groups. Early rejectors were those who presented with corneal graft rejection episode within first 6 months postoperatively, and late rejectors were those who presented with graft rejection episode later than 6 months after surgery. Descriptive analyses were performed to characterise the participants’ socio-demographic and clinical data. These included gender, age, indication for keratoplasty, past ocular history, presence or absence of crystalline lens, intraocular pressure (IOP), and presence or absence of other ocular features such as, corneal oedema and neovascularisation. Variables associated with the donor material used in our analyses included age, gender, cause of death, preservative used, storage times, and endothelial cell count. Surgical details analysed included donor and recipient cut size, suture type, associated surgeries, and surgical complications. Details of rejection episode were documented, including timing of episode, presence or absence of endothelial line, AC cells or flare, KP, and presence of any residual sutures. Treatment of the rejection episode was analysed next, followed by outcome in terms of success or failure of treatment of rejection episode.
Univariate analyses using χ2-statistic and Fisher's exact test for categorical, and Student's t-test or one-way ANOVA for continuous data were performed to identify factors that differed early and late rejectors. Binary logistic regression analyses for predictors of early rejectors were performed for variables, which were statistically significant in the univariate analyses. Data were analysed using the SPSS statistical software (Version 16, SPSS Science, Chicago, IL, USA).
Owing to the large number of statistical tests we are running on our sample, we chose to use a Bonferroni correction, and designated a P-value of 0.005 to indicate statistical significance.
Results
A total of 880 cases of PK, performed between 1991 and 2006, were identified. Of these, 229 cases of optical PK with subsequent corneal graft rejection were identified. After applying exclusion criteria, 156 files were available for review in the final analysis.
Clinical background of participants
The preoperative clinical characteristics of all patients with a graft rejection are shown in Table 1. Both groups were well matched for age and sex, with no significant differences between the two groups (P>0.005). Pseudophakic bullous keratopathy (PBK) was the most common indication for corneal transplant (37%), followed by keratoconus (21%). About 24% of PKP were performed for other varied reasons such as corneal stromal dystrophies, corneal decompensation secondary to other surgery, and traumatic scars, all of which were similarly distributed between early and late rejectors. Glaucoma was the most common comorbidity (21%), and prior retinal surgery was uncommon (4%). In all, 66% of patients had signs of corneal oedema at the time of grafting, and 14% of patients had at least one quadrant of corneal vascularisation. IOP was generally well controlled preoperatively, with an average ± SD pressure of 16±5 mm Hg. Overall, there were no statistically significant differences between the two groups (P>0.005).
Graft donors
There were no statistically significant differences between the donor characteristics in both groups. Mean age of the donors was 60±18 years (58±21 in early rejectors, 61±18 in late rejectors; P=0.34). The cause of donor's death was evenly distributed among different body systems in both groups. Optisol was the preferred preservative (72%), with McCarey Kaufman as the only other preservative used. Donor material was stored in the storage medium for a mean of 74±44 h (80±53 in early rejectors, 71±40 in late rejectors; P=0.30) with enucleation occurring 6±4.3 h (5±4 in early rejectors, 6±4.4 in late rejectors; P=0.29) after death in an average case. Donor material had a mean±SD endothelial cell count of 2543±329 cells/mm2 (2562±356 in early rejectors, 2536±321 in late rejectors; P=0.67). There were no significant differences between the early and late rejection patients on any of the donor factors (P>0.005).
Surgical technique
There were no statistically significant differences between the surgical techniques employed in both groups. Few patients had donor or recipient trephination sizes >9.0 mm in both groups (5% and 3%, respectively), with the majority of donor and recipient trephined sizes being 8.0–8.9 mm (71% and 72%, respectively). Interrupted sutures were most commonly used during the operation (72%). Cataract extraction was the most frequent surgery performed in conjunction with the PK (19%). Wound leak requiring resuturing was the only complication of note, with 14% of cases requiring this postoperatively. The differences between the early and late rejectors on any of these surgical factors were not statistically significant (P>0.005). Postoperative medications routinely consisted of antibiotic and corticosteroid eye drops, most commonly chloramphenicol 0.5% four times daily and prednisolone acetate 1% six times daily. In most patients, the corticosteroid eye drops were tapered by one drop every month, beginning at the third postoperative month. All patients were followed up in the corneal clinic at 1, 3, and 6 weeks, and 3 and 6 months postoperatively. Thereafter, the minimum follow-up visit schedule included a visit between months 6 and 12, and then annual visits through 5 years.
Diagnosis and presentation of graft rejection episode
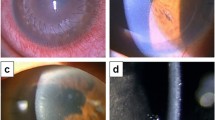
The clinical diagnosis of all patients with suspected corneal graft rejection was confirmed by a corneal specialist. For all graft recipients, the mean time±SD to rejection was 17±19 months, with 80% of rejections occurring within the first 24 months after surgery (Table 2). Overall, 42 (27%) patients experienced rejection episodes within 6 months after surgery whereas 114 (73%) patients experienced late rejection episodes, later than 6 months after surgery. At the time of presentation, AC inflammatory signs were noted in the form of KP (71%), AC cells (80%), and flare (55%). Endothelial rejection lines were uncommon (8%). Mean IOP at the time of presentation was 15.0±4.9 mm Hg. There were no statistically significant differences between the two groups’ characteristics at the presentation of the rejection episode (P>0.005; Table 2). There were 10 cases in which the diagnosis of graft rejection was based on the presence of corneal oedema only. These were excluded from the initial analysis.
Treatment and outcome of rejection episode
Prednisolone acetate 1% eye drops were the most frequently prescribed topical agent (55%) (Table 3). Topical dexamethasone was rarely used, but exclusively amongst early rejectors (14%, P<0.001). Twenty-seven percent of patients were not prescribed hourly topical steroids, as per the standard treatment regime. Systemic treatment was rarely used (3%). Rejection episodes responded well to treatment, with most (83%) being successfully managed. No other differences were found between the early and late rejection groups on the other treatment and outcomes variables (P>0.005; Table 3).
Further statistical analyses
We also analysed our results after inclusion of cases where corneal graft oedema was the only clinical sign of rejection (n=10). This did not significantly alter the results. On further analysis of data at 3 months, and 12-month cut-off time, our findings were mostly similar to those using a 6-month limit. These data were therefore not presented as well.
Multivariate analysis
Multivariate analyses were performed to ascertain whether any factors were independently associated with early rejection. We found that there were no preoperative characteristics, donor factors, surgical factors, clinical characteristics at presentation of rejection episode, or treatment factors, which independently predicted an early graft rejection (P>0.005).
Discussion
Attempts to identify and modify risk factors associated with corneal graft rejection are well reported in the literature.1, 4, 7, 9 However, there is no study that has comparatively evaluated the characteristics and treatment outcome of corneal graft rejection at different time points after penetrating keratoplasty. We undertook the present study in order to determine whether there were different risk factors and treatment outcomes in early and late rejectors. Only elective optical penetrating grafts were included for analysis in order to control the number of variables to be analysed. A Bonferroni correction was applied to our results to address the problem of multiple comparisons. We chose 6 months as the cut-off time for early and late rejectors on the basis of the evidence provided by the Cornea Transplant Follow-up Study conducted across the United Kingdom and Ireland in which the risk of graft rejection was found to be the highest during first 150 days postoperatively.2
Overall, in our cohort, 42 (27%) patients had early rejection episodes whereas 114 (73%) patients experienced late rejection episodes. Our results showed that none of the characteristics in preoperative clinical profile of patients differed between the two groups. This contrasts with the study done by Vail et al4 who found that preoperative age, diagnosis, and glaucoma impacted time to rejection, though they did not specify the details of this association. Overall, the effects of age and glaucoma on graft rejection have been the subject of much conjecture in the literature,4, 10, 11, 12, 13, 14, 15 and we believe our findings support the hypothesis that neither of these factors impacts on graft rejection. Donor tissue factors and surgical techniques did not have an impact upon the timing of rejection episode in our study, which is consistent with the current opinion that donor factors and surgical technique have a little impact upon corneal graft survival.16 Recently compiled data from the Cornea Donor Study has also shown that donor characteristics, such as donor age, ABO compatibility, method of tissue retrieval, processing factors, and timing of use of the cornea, are unrelated to the risk of graft failure.17, 18, 19
The Cornea Transplant Follow-up Study reported that use of mixed suturing, larger grafts, and grafts with poor matching at HLA class I antigens were associated with an increased risk of rejection. Risk of rejection reduced with increasing recipient age, increased for those with glaucoma or with diagnoses of secondary endothelial failure and inflammation, regrafts, and large grafts. This study had confounding variables, most importantly the inclusion of non-optical and therapeutic corneal grafts in the analyses. Furthermore, there was no information regarding the timing of graft rejection after corneal transplantation. None of these factors were found to be associated with the timing of occurrence of corneal graft rejection in our study.
Treatment prescribed for corneal graft rejection in our study is consistent with other studies, with prednisolone acetate being the most commonly prescribed topical steroid.20 Treatment in both the group was similar with the exception of dexamethasone, which was used more commonly amongst early rather than late rejectors. Dexamethasone has been used as a standard therapy for treatment of graft rejection in an earlier study with a high rate of reversal of graft rejection episodes.21 Though this is an interesting finding in the present study, further work is needed to confirm this result as patient numbers using dexamethasone were small resulting in a study power of 4%, which is insensitive to detect a risk reduction at α level of 0.05.
Overall, outcomes of early and late episodes of graft rejection were found to be quite similar, with 83% of patients having their rejection episode successfully reversed with medical treatment, with both early and late rejectors reaching an end point in similar time frames. However, no statistically significant difference was found in the preoperative and intraoperative characteristics in both groups. We also looked at a 3-month and 12-month cut-off time, and our findings were mostly similar to those using a 6-month limit. These data were therefore not presented.
We recognise that there are limitations to this study, especially because of the retrospective nature of the study design. The quality of data is dependent upon documentation provided within the patient files. In order to lessen recall bias, all cases of PK were reviewed for evidence of graft rejection rather than rely on medical record coding of rejection episodes. Reviewer bias was minimised through use of strict guidelines to accurately identify events, such as rejection episodes, and outcomes, and where notes were unclear, a second reviewer was consulted. Owing to the extended time course of this review, various surgeons were involved in the care of this patient group; however, we did find that a similar surgical technique was used between both groups (P>0.005). Furthermore, whilst there were a variety of surgeons involved, all cases of PK were managed and followed up at a single centre, where a standard practice for management of PK patients is followed. We also believe that there are limitations regarding the definitions of corneal allograft rejection that are being used for such studies. Although standard criteria were employed for the diagnosis of allograft rejection in the present study, there may be potential for over as well as under diagnosis.
We did not study HLA/ABO matching as these factors have not conclusively altered the outcome of corneal transplant rejections, and have been shown to not impact upon transplant failure either.9, 16, 17
In conclusion, our study indicates that the timing of corneal graft rejection cannot be predicted on the characteristics analysed herein. Our study also shows that both early and late rejectors respond equally to treatment for corneal allograft rejection.

References
Williams KA, Hornsby N, Bartlett C, Holland H, Esterman A, Coster D . The Australian Corneal Graft Registry 2004 Annual Report. Flinders University Press: Adelaide, 2004.
Wilson SE, Kaufman HE . Graft failure after penetrating keratoplasty. Surv Ophthalmol 1990; 34 (5): 325–356.
Rahman I, Huang MC, Carley F, Hillarby MC, Vasileiadis GT, Tullo A . The influence of donor and recipient factors in allograft rejection of the human cornea. Eye (Lond) 2010; 24 (2): 334–339.
Vail A, Gore SM, Bradley BA, Easty DL, Rogers CA, Armitage WJ . Conclusions of the corneal transplant follow up study. Collaborating Surgeons. Br J Ophthalmol 1997; 81 (8): 631–636.
Williams KA, Lowe MT, Bartlett CM, Kelly L, Coster DJ . The Australian Corneal Graft Registry 2007 Report. Flinders University Press: Adelaide, 2007.
Streilein JW . Anterior chamber associated immune deviation: the privilege of immunity in the eye. Surv Ophthalmol 1990; 35 (1): 67–73.
Maguire MG, Stark WJ, Gottsch JD, Stulting RD, Sugar A, Fink NE et al. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Ophthalmology 1994; 101 (9): 1536–1547.
Volker-Dieben HJ, D’Amaro J, Kok-van Alphen CC . Hierarchy of prognostic factors for corneal allograft survival. Aust N Z J Ophthalmol 1987; 15 (1): 11–18.
Volker-Dieben HJ, Claas FH, Schreuder GM, Schipper RF, Pels E, Persijn GG et al. Beneficial effect of HLA-DR matching on the survival of corneal allografts. Transplantation 2000; 70 (4): 640–648.
Williams KA, Esterman AJ, Bartlett C, Holland H, Hornsby NB, Coster DJ . How effective is penetrating corneal transplantation? Factors influencing long-term outcome in multivariate analysis. Transplantation 2006; 81 (6): 896–901.
Reinhard T, Kallmann C, Cepin A, Godehardt E, Sundmacher R . The influence of glaucoma history on graft survival after penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol 1997; 235 (9): 553–557.
Boisjoly HM, Bernard PM, Dube I, Laughrea PA, Bazin R, Bernier J . Effect of factors unrelated to tissue matching on corneal transplant endothelial rejection. Am J Ophthalmol 1989; 107 (6): 647–654.
Sit M, Weisbrod DJ, Naor J, Slomovic AR . Corneal graft outcome study. Cornea 2001; 20 (2): 129–133.
Williams KA, Muehlberg SM, Lewis RF, Coster DJ . Influence of advanced recipient and donor age on the outcome of corneal transplantation. Australian Corneal Graft Registry. Br J Ophthalmol 1997; 81 (10): 835–839.
Kuchle M, Cursiefen C, Nguyen NX, Langenbucher A, Seitz B, Wenkel H et al. Risk factors for corneal allograft rejection: intermediate results of a prospective normal-risk keratoplasty study. Graefes Arch Clin Exp Ophthalmol 2002; 240 (7): 580–584.
Vail A, Gore SM, Bradley BA, Easty DL, Rogers CA, Armitage WJ . Influence of donor and histocompatibility factors on corneal graft outcome. Transplantation 1994; 58 (11): 1210–1216.
Dunn SP, Stark WJ, Stulting RD, Lass JH, Sugar A, Pavilack MA et al. The effect of ABO blood incompatibility on corneal transplant failure in conditions with low-risk of graft rejection. Am J Ophthalmol 2009; 147 (3): 432.e3–438.e3.
Sugar J, Montoya M, Dontchev M, Tanner JP, Beck R, Gal R et al. Donor risk factors for graft failure in the cornea donor study. Cornea 2009; 28 (9): 981–985.
gal RL, Dontchev M, Beck RW, Mannis MJ, Holland EJ, Kollman C et al. The effect of donor age on corneal transplantation outcome results of the cornea donor study. Ophthalmology 2008; 115 (4): 620–626.e6.
Barker NH, Henderson TR, Ross CA, Coster DJ, Williams KA . Current Australian practice in the prevention and management of corneal allograft rejection. Clin Experiment Ophthalmol 2000; 28 (5): 357–360.
Hudde T, Minassian DC, Larkin DF . Randomised controlled trial of corticosteroid regimens in endothelial corneal allograft rejection. Br J Ophthalmol 1999; 83: 1348–1352.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Perera, C., Jhanji, V., Lamoureux, E. et al. Clinical presentation, risk factors and treatment outcomes of first allograft rejection after penetrating keratoplasty in early and late postoperative period. Eye 26, 711–717 (2012). https://doi.org/10.1038/eye.2012.14
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.14