Abstract
Purpose
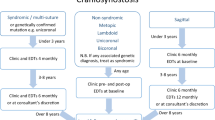
Adults with facial nerve paresis (FNP) generally develop ectropion, but a recent report of children with syndromatic FNPs implies that entropion may be more common in this setting than ectropion. This study evaluates eyelid position and other periorbital changes in children with isolated, non-syndromatic FNP.
Methods
Charts were reviewed of 10 sequential children who presented to a major national eye referral centre with isolated FNP of variable aetiology. Severity of FNP was assessed according to the House-Brackmann scale.
Results
All 10 patients (4 males and 6 females; mean age at presentation, 4 years) had unilateral, isolated FNP. Mild lower-eyelid entropion was present in four patients, and severe lower-eyelid entropion required surgical correction in three patients. All patients had lower eyelid retraction (mean 2.3 mm) and lagophthalmos (mean 2.9 mm). None had enophthalmos, lower eyelid ectropion, or brow ptosis.
Conclusion
Unlike adults, children with isolated FNP seem prone to develop entropion rather than ectropion. Entropion reported previously in five syndromic children with FNP seems more likely related to patients’ age than to their congenital syndromes.
Similar content being viewed by others
Introduction
Ectropion is common in adults with facial nerve paresis (FNP),1, 2 but a recent report described entropions in a small group of children with syndromic FNP.3 Eyelid position has not yet been carefully evaluated in children with isolated FNP,2, 4, 5, 6, 7, 8, 9, 10 so this study reports eyelid and periorbital changes in 10 consecutive children presenting with isolated FNP.
Methods
Medical records were reviewed of 10 consecutive children who were presented to King Abdulaziz University Hospital, Riyadh, Saudi Arabia, with isolated lower motor neuron FNP between January 2007 and January 2011. Patients who had undergone previous ophthalmic surgery and patients with obvious craniofacial disorders were excluded. The information that was recorded included the cause of FNP, the complete ophthalmologic clinical examination, and ophthalmologic surgical procedures needed to manage the consequences of FNP.
Results
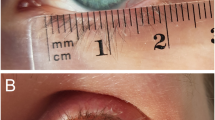
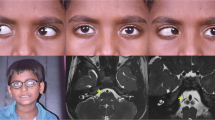
Table 1 summarizes the aetiology of FNP, age at onset and presentation, lower eyelid observations, and surgeries performed. All 10 patients (4 males and 6 females; mean age 4 years at presentation) had unilateral FNP with House-Brackmann grade III or IV at presentation.11 Severe lower eyelid entropion with trichiasis was present in three patients (Figures 1a and b), while mild lower eyelid entropion without trichiasis was seen in four patients when initially evaluated (Figures 2a and b). None of the patients had enophthalmos, lower eyelid ectropion, or a significant abnormality of the eyelid skin, tarsus, or conjunctiva. All patients had lower eyelid retraction (mean 2.3 mm; range 1–3 mm) and lagophthalmos (mean 2.9 mm; range 1–4 mm) (Figure 2c), and three patients had 1 mm of upper eyelid retraction on the affected side.
(a) A 4-year-old girl with left-sided facial paralysis secondary to middle ear infection presented with severe lower eyelid entropion causing marked ocular irritation due to trichiasis. (b) The same patient 6 months after entropion repair by reinsertion of the lower eyelid retractors into the lower anterior part of the tarsus. Entropion was improved, but she continued to have the same degree of lower eyelid retraction postoperatively.
All patients had moderate to severe decrease in frontalis function on the affected side, but none had eyebrow ptosis. Also, none of the patients had clinically evident aberrant regeneration of the facial nerve, but five patients had mild atrophy of the mid-face on the affected side. All patients had normal ocular motility and otherwise grossly normal neurologic and general medical examinations; none had major general medical problems. The five patients with congenital onset did not have a family history of FNP.
In three patients, lower eyelid retractors were reinserted into the lower anterior part of the tarsus through a subciliary incision to correct severe lower eyelid entropion (Figures 1a and b).
Discussion
We report 10 children who presented sequentially to a national ophthalmology centre between the ages of 2 and 8 years with congenital or acquired, isolated, unilateral lower motor neuron facial nerve palsies. Four had some degree of entropion, and three had severe entropion with trichiasis requiring surgical correction. These patients had no other obvious visual, neurologic, or general medical problems. Age at onset and presentation, etiology and severity of FNP, and duration of symptomatology were not consistently associated with severity of entropion. The three operated patients were relatively young (ages 2, 3, and 5 years at the time of surgery), but their lid problems may have brought them to medical attention relatively early.
Lower eyelid entropion has been described previously in a small group of children with FNP and craniofacial abnormalities.3 Our report shows that entropion is also a frequent observation in children with diverse causes of isolated, unilateral FNP without craniofacial syndromes. The mechanism of lower eyelid changes observed in this study was not clear, although the presence of tight medial and lateral canthal tendons in children might combine with a loss in the balance between the orbicularis oculi and lower eyelid retractors in patients with FNP to contribute to the development of lower eyelid entropion and lid retraction.3, 12 Alternatively, maldevelopment or repair of the peripheral facial nerve injury might lead to subclinical hyperactivity of previously paralyzed periocular muscles.
A few additional observations are probably valuable regarding the facial appearance of these children. These children did not have eyebrow ptosis even after substantial loss of frontalis function, while adults with FNP generally exhibit clinical brow ptosis.2 This may be due to a laxity of the forehead and eyebrows that develops with age.12 Impairment of facial nerve innervation of the cheek muscles almost certainly contributed to the mild cheek atrophy observed in five of the patients.
There are a few limitations to this study. The patient group is relatively small and was studied retrospectively. Patients were seen at a national ophthalmology centre, which may reflect a referral bias for somewhat worse symptomatology than the typical child with isolated FNP. Finally, neuroimaging and electrodiagnostic studies were not performed on these patients because these were not necessary for the clinical care provided. The observations reported here should be confirmed with a larger group of patients from multiple ethnicities in the future.

References
Bashour M, Harvey J . Causes of involutional ectropion and entropion—age-related tarsal changes are the key. Ophthal Plast Reconstr Surg 2000; 16 (2): 131–141.
Rahman I, Sadiq SA . Ophthalmic management of facial nerve palsy: a review. Surv Ophthalmol 2007; 52 (2): 121–144.
Pasco NY, Kikkawa DO, Korn BS, Punja KG, Jones MC . Facial nerve paralysis: an unrecognized cause of lower eyelid entropion in the pediatric population. Ophthal Plast Reconstr Surg 2007; 23 (2): 126–129.
Evans AK, Licameli G, Brietzke S, Whittemore K, Kenna M . Pediatric facial nerve paralysis: patients, management and outcomes. Int J Pediatr Otorhinolaryngol 2005; 69 (11): 1521–1528.
Falco NA, Eriksson E . Facial nerve palsy in the newborn: incidence and outcome. Plast Reconstr Surg 1990; 85 (1): 1–4.
Grundfast KM, Guarisco JL, Thomsen JR, Koch B . Diverse etiologies of facial paralysis in children. Int J Pediatr Otorhinolaryngol 1990; 19 (3): 223–239.
Manning JJ, Adour KK . Facial paralysis in children. Pediatrics 1972; 49 (1): 102–109.
May M, Fria TJ, Blumenthal F, Curtin H . Facial paralysis in children: differential diagnosis. Otolaryngol Head Neck Surg 1981; 89 (5): 841–848.
Melvin TA, Limb CJ . Overview of facial paralysis: current concepts. Facial Plast Surg 2008; 24 (2): 155–163.
Toelle SP, Boltshauser E . Long-term outcome in children with congenital unilateral facial nerve palsy. Neuropediatrics 2001; 32 (3): 130–135.
House JW, Brackmann DE . Facial nerve grading system. Otolaryngol Head Neck Surg 1985; 93 (2): 146–147.
van den Bosch WA, Leenders I, Mulder P . Topographic anatomy of the eyelids, and the effects of sex and age. Br J Ophthalmol 1999; 83 (3): 347–352.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Alsuhaibani, A., Bosley, T., Goldberg, R. et al. Entropion in children with isolated peripheral facial nerve paresis. Eye 26, 1095–1098 (2012). https://doi.org/10.1038/eye.2012.102
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.102