Abstract
Background/Objectives
To determine whether horizontal lower eyelid margin length shortens following facial nerve palsy (FNP).
Subjects/Methods
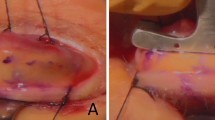
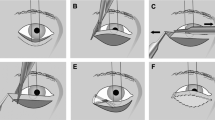
A single-centre retrospective audit of lower eyelid margin horizontal length, measuring from the lower lacrimal punctum to lateral canthal angle with a straight plastic ruler, with the eyelid on gentle stretch (‘punctum-to-canthus (PC) distance’), recorded in all FNP patients reviewed in July–September 2021. Affected and fellow eyes were compared using parametric testing.
Results
Forty-one patients were reviewed. Seventeen were excluded due to previous surgery that would lengthen (e.g., periosteal flap) or shorten (e.g., lateral tarsal strip) the lower eyelid margin. Of the remaining 24, mean age was 52.5 years (range, 27–79) and 54% were female. Mean PC distance was significantly shorter in affected eyes (26.0 mm, range: 22–34 mm) compared to fellow eyes (27.5 mm, 24–35 mm) (paired t-test, T(23) = 6.06, p < 0.00001). Mean difference between both eyes’ PC distance was 1.5 mm (0–4 mm). Only three patients were still in the ‘paralytic phase’ (i.e., <1 year since FNP onset), and difference in PC distance was 0 mm in all three. A reduction in lower eyelid PC distance was weakly associated with a reduction in upper eyelid lid-margin-to-brow distance (R = 0.4775, p = 0.0286).
Conclusions
The lower eyelid margin appears to shorten horizontally following FNP. This study provides proof-of-concept for the use of measuring PC distance in patients with FNP as an additional tool for the overall assessment of soft tissue contraction following FNP. It may help identify patients in whom further lower eyelid margin shortening should be avoided and in whom eyelid lengthening may be required.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ziahosseini K, Venables V, Neville C, Nduka C, Patel B, Malhotra R. Occurrence and severity of upper eyelid skin contracture in facial nerve palsy. Eye. 2016;30:713–7.
Aramideh M, Koelman JHTM, Devriese PP, Speelman JD, Ongerboer de Visser BW. Thixotropy of levator palpebrae as the cause of lagophthalmos after peripheral facial nerve palsy. J Neurol Neurosurg Psychiatry. 2002;72:665–7.
Maqsood SE, Cascone N, Grixti A, Kannan R, Nduka C, Malhotra R. Functional and aesthetic outcomes of eyelid skin grafting in facial nerve palsy. Br J Ophthalmol. 2019;103:686–91.
Trettin H. Neurological principles of edema in inactivity. Z Lymphol. 1992;16:14–16.
Siah WF, Litwin AS, Nduka C, Malhotra R. Periorbital autologous fat grafting in facial nerve palsy. Ophthalmic Plast Reconstr Surg. 2017;33:202–8.
Jamison A, Patel BCK, Malhotra R. Lower eyelid lengthening in facial nerve palsy: when is a periosteal flap required? Presented at the 14th International Facial Nerve Symposium, Seoul, Korea, May 2022. https://www.ifns2022.org/.
Funding
The study was supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology & Visual Sciences, University of Utah.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and/or design of the work, and to the acquisition, analysis, and/or interpretation of data for the work. AJ drafted the work and all authors revised it critically for important intellectual content. All authors gave final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jamison, A., Patel, B.C.K. & Malhotra, R. Horizontal shortening of the lower eyelid margin in facial nerve palsy. Eye 38, 205–209 (2024). https://doi.org/10.1038/s41433-023-02661-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02661-2