Abstract
The approach of all ophthalmologists, diabetologists and general practitioners seeing patients with diabetic retinopathy should be that good control of blood glucose, blood pressure and plasma lipids are all essential components of modern medical management. The more recent data on the use of fenofibrate in the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) and The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye studies is reviewed. In FIELD, fenofibrate (200 mg/day) reduced the requirements for laser therapy and prevented disease progression in patients with pre-existing diabetic retinopathy. In ACCORD Eye, fenofibrate (160 mg daily) with simvastatin resulted in a 40% reduction in the odds of retinopathy progressing over 4 years, compared with simvastatin alone. This occurred with an increase in HDL-cholesterol and a decrease in the serum triglyceride level in the fenofibrate group, as compared with the placebo group, and was independent of glycaemic control. We believe fenofibrate is effective in preventing progression of established diabetic retinopathy in type 2 diabetes and should be considered for patients with pre-proliferative diabetic retinopathy and/or diabetic maculopathy, particularly in those with macular oedema requiring laser.
Similar content being viewed by others
Introduction
Diabetic eye disease affects up to 50 million people worldwide, and its prevalence is projected to double by 2025 in the absence of better therapeutic preventive strategies. In developed countries, diabetic retinopathy (DR) is the leading cause of vision loss in adults of working age (20–65 years),1 and substantially impacts on the patient quality of life.2 In the United Kingdom, retinopathy affects about 40% of people with diabetes and nearly 20% have retinopathy at the time of diagnosis of type 2 diabetes.3 Prevalence and severity of diabetic retinopathy seem to be higher in some ethnic groups, specifically in those of Hispanic, Afro Caribbean,4, 5, 6 or Indo-Asian origin.7 These data suggest that the burden of diabetic eye disease may be even greater in rapidly developing regions.
Pathogenesis of diabetic eye disease
Microangiopathy and capillary occlusion underlie the pathogenesis of DR.8 Together, these lead to microvascular leakage and breakdown of the blood–retinal barrier, resulting in retinal haemorrhage, exudates and oedema, as well as the development of macular oedema. In addition, microvascular occlusion and ischaemia give rise to ‘cotton wool’ spots, capillary changes, arteriovenous shunts, and neovascularisation. An increase in the level of vascular endothelial growth factor (VEGF) is probably one of the major angiogenic factors implicated in the pathogenesis of DR.9
Management priorities
Early identification and treatment are key priorities for reducing the morbidity of diabetic eye disease. However, although evidence supports the benefit of laser therapy, such treatment is not completely effective.10 Medical management of risk factors, specifically intensive control of glycaemia and blood pressure, is important in the prevention of DR. There is evidence to support intensive control from major prospective studies, such as the United Kingdom Prospective Diabetes Study (UKPDS).11, 12 In the UKPDS, the risk of microvascular complications in type 2 diabetes was shown to be associated, independently, and additively, with hyperglycaemia and hypertension, with risk reductions of 37% per 1% decrement in glycated haemoglobin (HbA1C) and 11% per 10 mm Hg decrease in systolic blood pressure. Angiotensin-converting enzyme blockade (ACE inhibition) has been specifically studied with the basic premise that ACE inhibition has additional benefits on diabetic retinopathy specific to this group of drugs that are independent of blood pressure effects. In the DIRECT study (reviewed in Wright and Dodson13) 5 years of candesartan treatment in type 1 diabetes reduced the incidence of retinopathy by two or more steps (EDTRS) in severity by 18% and, in a post-hoc analysis, reduced the incidence of retinopathy by three step progression by 35%. In type 1 diabetes patients, there was no effect on progression of established retinopathy. In contrast, in type 2 diabetes, 5 years of candesartan treatment resulted in 34% regression of retinopathy. Importantly, an overall significant change towards less-severe retinopathy was noted in both type 1 and 2 diabetes.
Whether further improvement and tighter control of proven risk factors provide greater benefit is controversial, and has been addressed by The Action to Control Cardiovascular Risk in Diabetes (ACCORD) and ADVANCE studies described later. Consensus based on the available evidence is that achievement of recommended targets for HbA1c and blood pressure ameliorate but do not eliminate the risk of diabetic retinopathy, suggesting the need to target other potential risk factors that may be implicated in the pathogenesis of diabetic retinopathy. It is therefore vital that other therapeutic targets are considered for potential benefit in the treatment and prevention of diabetic retinopathy.
More recent developments include the use of intravitreal injection of VEGF inhibitors, such as ranibizumab (Lucentis, Novartis Pharmaceuticals UK Ltd, Camberley, UK ) and pegaptanib (Macugen, Pfizer Ltd, Tadworth, UK). Ranibizumab has shown extensive trial data of benefit in diabetic macular oedema for example in the large DRCR.net14 and bevacizumab, unlicensed for ocular use, showed improved outcomes in patients with macular oedema compared with laser therapy in the smaller BOLT study.15 Other trials of new medical therapies have focused on blockade of the protein kinase C pathway (ruboxistaurin) showing an effect with reduction of laser treatment and visual loss in patients with diabetes with maculopathy,16 such that this agent has an approvable letter from the US FDA while further trial data are completed.
Do lipids have a role?
Patients with combined dyslipidemia, but not familial hypercholesterolaemia, have an increased incidence of retinal abnormalities. This suggests that elevated cholesterol and triglycerides may be implicated in the development of retinovascular lesions occurring in diabetic retinopathy (for example, haemorrhage and cotton-wool spots).17 Evidence from observational studies has also supported a link between serum lipids and diabetic eye disease. Elevated total and low-density lipoprotein (LDL) cholesterol levels, and triglycerides were associated with progression of retinopathy, proliferative retinopathy,18, 19 and the development of macular oedema.20 Besides, a high total to high-density lipoprotein (HDL) cholesterol ratio and elevated LDL cholesterol were each associated with the development of clinically significant macular oedema.21 Furthermore, measurement of lipoprotein subclass using nuclear magnetic resonance showed positive associations between the severity of retinopathy and triglyceride levels, and LDL particle concentration and apolipoprotein B levels (a constituent lipoprotein of very-low density, intermediate-density lipoproteins, and LDL), and a negative association with HDL cholesterol.22
Statins and fibrates
Lipid lowering may be another approach to reduce diabetic retinopathy endpoints,23 particularly for macula oedema and exudation. The possibility of an effect of statins has been investigated over the last 10 years with early encouraging results in small studies of macular oedema and exudates.24 Larger studies of statins for example CARDS,25 which included 2838 patients over a median follow-up of 3.9 years, showed that atorvostatin 10 mg daily resulted in a trend to reduction of laser therapy compared with placebo, but no influence on diabetic retinopathy progression. Thus, the influence of statins on diabetic retinopathy continues to be debated and better evidence on the effects of larger doses of statins are required but, if there is an effect of statins, it is likely to be small.26
Similarly early clinical studies showed a benefit using fibrates in patients with diabetic maculopathy, with a reduction in retinal and macular exudation.27, 28, 29 Two randomised controlled trials of fenofibrate have confirmed benefit in established retinopathy (Table 3).
FIELD study
In the important Fenofibrate Intervention and Event Lowering in Diabetes (FIELD)30 study fenofibrate reduced the requirements for laser therapy in patients with pre-existing retinopathy (numbers need to treat (NNT) to avoid first laser 17) and prevented disease progression (NNT 9) in patients with pre-existing retinopathy. These benefits did not seem to be related to changes in lipids, as there were no reported clinically relevant differences in mean plasma HDL cholesterol or triglyceride concentrations in those lowered or not. This study with its methodological issues, conclusions, and clinical implications has been previously reviewed for this journal.23
ACCORD EYE studies—glycaemic control, blood pressure and lipid lowering
Further evidence is now available on the value of the management of dyslipidaemia on diabetic retinopathy from the ACCORD Eye study.31 This was a subgroup of 2856 patients within the main study of the ACCORD32, 33 study of patients with type 2 diabetes selected for increased cardiovascular risk. In this study, the effects on cardiovascular outcomes of
-
1)
Intensive glycaemic control (target HbA1c <42 mmol/mol) was compared with standard control (target HbA1c 53–63 mmol/l) using metformin, sulphonylurea or meglitinides, rosiglitazone, acarbose, and insulin.
-
2)
Intensive blood pressure control, systolic blood pressure <120 mm Hg, was compared with standard control <140 mm Hg in the context of good glycaemic control, using all the standard hypotensive medications.
-
3)
Lipid management in the context of good glycaemic control using simvastatin (20 mg daily for primary prevention and 40 mg daily for secondary prevention) in all patients with the addition of fenofibrate or placebo. Fenofibrate 160 mg daily was used, if GFR was ≥50 ml/min and 54 mg daily and 30–<50 ml/min and was discontinued, if GFR fell to <30 ml/min.
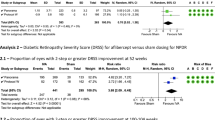
The subgroup had seven-field retinal photographs at baseline and at 4 years. In summary, at the end of the study the rates of progression of diabetic retinopathy were significantly reduced in the intensive glycaemic control group and in the fenofibrate group, but not in the intensive blood pressure control group (Tables 1 and 2 ).
Glycaemia and blood pressure in ACCORD
Attempts to achieve normal plasma glucose concentrations and blood pressure levels are logical conclusions of much of the trial evidence showing benefits of reducing glucose and blood pressure. However, the safety of pursuing such intensive therapy for glycaemic control has been questioned,34 not from an ophthalmic point of view, but from increased hypoglycaemia and cardiovascular events. In the ACCORD study hypoglycaemia requiring third party assistance was increased from 3.5–10.5% (P<0.001), and there was an increased rate of death from any cause (4.0 vs 5.0%). The main glycaemia trial was therefore stopped early after a mean 3.5 years follow-up, potentially underestimating the reported effect of glycaemia treatment on diabetic retinopathy. It was of interest that it was the median times from the onset of severe hypoglycaemia to the first major macrovascular event, the first major microvascular event and death that were significant different in the intensively treated group, with no relationship being found between repeated episodes of severe hypoglycaemia and vascular outcomes and death. It should be noted that thiazolidinediones were widely prescribed in the ACCORD study (92% in the intensive-therapy group vs 58% in the standard therapy group). Similar findings were noted in the ADVANCE study35 of intensive glycaemic therapy in type 2 diabetes based on sulphonylureas with less than 20% use of thiozolidinediones, in which a mean glycated haemoglobin level of 48 mmol/mol (6.5%) was achieved in the intensive-control group compared with 56 mmol/mol (7.3%) in the standard-control group. Severe hypoglycaemia, although uncommon, was more common in the intensive-control group (2.7, vs 1.5% in the standard-control group; hazard ratio, 1.86; 95% CI, 1.42 to 2.40; P<0.001). The incidence of combined major macrovascular and microvascular events (18.1, vs 20.0% with standard control) was reduced. Good glycaemic control remains an important aim, but these results have modified current advice on glycaemic control in those with established cardiovascular disease and in older subjects where less strict targets should be set.
A surprising result of the ACCORD Eye study was the failure to demonstrate a significant effect of intensive blood pressure control on the progression of retinopathy. It is possible that the median systolic pressure of 133 mm Hg in the non-intensive treatment group was an effective level for preventing progression or that the duration of follow-up was insufficient.
Lipids in ACCORD Eye study
The important finding of the ACCORD Eye study with regard to diabetic retinopathy confirms the new therapeutic approach of lipid-lowering therapy with fenofibrate in combination with a statin, as had been suggested in the previous FIELD study.
An impressive 40% reduction in the odds of having progression of retinopathy over 4 years conveyed by fenofibrate (160 mg formulation/day), compared with simvastatin alone, is an important finding. This occurred with an increase in HDL-cholesterol and a decrease in the serum triglyceride level in the fenofibrate group, as compared with the placebo group, being noted in the first year of treatment and maintained through to the end of the study. In ACCORD Eye the effect of fenofibrate was independent of glycaemia. No data are available to indicate which features of retinopathy progressed and whether any evidence of regression was noted, which is important in clinical practice to guide which patients may be specifically benefited. The ACCORD Eye trial results are in agreement with the FIELD study that previously reported a protective effect of fenofibrate, with significant reduction of laser treatment of 40% for both diabetic retinopathy or maculopathy. In earlier trials with clofibrate and gemfibrozil there were concerns about rhabdomyolysis, and a retrospective cohort study showed an incidence rates ratio of rhabdomyolysis of 3.75 for combination therapy compared with statin alone,36 but importantly in both the FIELD and ACCORD Eye studies, prescription of fenofibrate with a statin was safe and rhabdomyolysis was not increased. Fenofibrate reduced albuminuria and slowed eGFR loss in the FIELD trial, despite and initial, reversible rise of plasma creatinine of 10.0 mol/l.
In interpreting these two studies and their clinical implication, it must be noted that DR was not the primary endpoint by design in either study, a tertiary endpoint in FIELD, and DR endpoints recorded in a substudy cohort of the ACCORD study population. Nevertheless, a suitable number of patients were studied over a reasonable length of time.
Mechanism of function of fenofibrate
The mechanism of function of fenofibrate in reducing progression of diabetic retinopathy is unclear. Fibric-acid derivatives, which are peroxisome proliferator-activated receptor a (PPARa) agonists, have beneficial effects on lipid profiles, including lowering triglycerides and increasing HDL-cholesterol. PPARa has become a therapeutic target in diabetic vascular damage.37 Fenofibrate has been shown to improve endothelial dysfunction in patients with type 2 diabetes with dyslipidemia.38 Fenofibrate probably has direct anti-inflammatory effects including the modulation of the expression of several cytokines and adhesion molecules and anti-atherosclerotic effects.39 Fenofibrate has been shown to potently induce a sustained activation of AMP-activated protein kinase (AMPK) and vascular endothelial growth factor (VEGF) mRNA expression in human retinal endothelial cells in vitro. In the experiment compound C, a specific AMPK inhibitor, almost completely blocked the fenofibrate-induced survival effect, as well as VEGF mRNA expression. These results suggest that fenofibrate prevents apoptotic cell death induced by serum deprivation through PPARa-independent, but AMPK-dependent pathway resulting in a novel therapeutic property that may control unwanted cell death found in diabetic retinopathy.40, 41 The trial data do not clarify which mechanism is important clinically. In particular the FIELD study suggested that it may be independent of lipid lowering as there was no difference in the lipid levels of those requiring laser or not, although this was in contrast to the ACCORD Eye data that did show a difference in triglyceride levels.
Conclusion
A systematic review of the literature as recent as 200742 concluded that evidence was insufficient for the efficacy or safety of medical interventions including lipid-lowering therapy and antivascular endothelial growth factors on the incidence or progression of DR, but recent trials are changing these negative conclusions. Indeed trial planners are now faced with reducing numbers of retinopathy endpoints because of better overall medical management. The therapeutic approach of all ophthalmologists, diabetologists, and general practitioners seeing patients with diabetic retinopathy should be that good control of blood glucose, blood pressure, and plasma lipids are all essential components of modern medical management. Patients should be given appropriate advice not only at the time of diagnosis of diabetes, but also as soon as retinopathy is first diagnosed. Better outcomes follow good glycaemic control early in the course of the diabetes,43 but it is rarely too late to show benefit from improved control. Care should be taken to avoid over-zealous glycaemic and blood pressure control in older patients and in those with established cardiovascular disease.
Fibrates would seem to have an important beneficial effect on diabetic retinopathy (Table 3 ). A specific study of fenofibrate in a small diabetic maculopathy trial with primary OCT endpoints is underway. In the meantime clinicians must appraise the two randomised controlled trials of fenofibrate and be aware of the safety and considerable potential benefit of this simple treatment as a secondary prevention strategy.44 We believe fenofibrate is effective in preventing progression of established diabetic retinopathy in type 2 diabetes and adoption of fenofibrate will have widespread prescription and cost implications as about 40% of diabetic patients have retinopathy. The cost of fenofibrate is relatively low considering the impressive NNT in clinical trials, and in the United Kingdom varies between ∼£7 and £22 per 28 days depending on the dose and preparation. In our clinical practice, we recommend and use fenofibrate for patients with pre-proliferative diabetic retinopathy and/or diabetic maculopathy, particularly in patients with macular oedema requiring laser. Experience has also suggested that fenofibrate should be used when there is early diabetic retinopathy in the only or best eye, and in those with maculopathy with poor or limited response to laser therapy or where laser therapy cannot be undertaken with lesions too close to the fovea. Optimising the medical management of diabetic retinopathy should address the control of glycaemia, blood pressure, and lipids, and based on recent trials, specific therapies using fenofibrate with a statin and candesartan should be considered (Table 4 ).
References
Fong DS, Aiello AP, Ferris FL, Klein R . Diabetic retinopathy. Diabetes Care 2004; 27: 2540–2553.
Candrilli SD, Davis KL, Kan HJ, Lucero MA, Rousculp MD . Prevalence and the associated burden of illness of symptoms of diabetic peripheral neuropathy and diabetic retinopathy. J Diabetes Complications 2007; 21: 306–314.
Diabetes UK. Diabetes and blindness: a focus on action. A report from Diabetes UK. June 2005. Available from www.diabetes.org.uk.
Emanuele N, Sacks J, Klein R, Reda D, Anderson R, Duckworth W et al. Ethnicity, race and baseline retinopathy correlates in the Veterans Affairs Diabetes Trial. Diabetes Care 2005; 28: 1954–1958.
Harris PD, Klein R, Cowie CC, Rowland M, Byrd-Holt DD . Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? Diabetes Care 1998; 21: 1230–1235.
The Eye Disease Prevalence Research Group. The prevalence of diabetic retinopathy among adults of the United States. Arch Ophthalmol 2004; 122: 552–563.
Day C . The rising tide of type 2 diabetes. Br J Diabetes Vasc Dis 2001; 414: 813–820.
Brownlee M . Banting Lecture 2004. The pathobiology of diabetic complications. A unifying mechanism. Diabetes 2005; 54: 1615–1625.
Nguyen QD, Tatlipinar S, Shah SM, Haller JA, Quinlan E, Sung J et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol 2006; 142: 961–969.
Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology 1991; 98: 766–785.
The UKPDS Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. UKPDS 33. Lancet 1998; 352: 837–853.
The UKPDS Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998; 317: 703–713.
Wright AD, Dodson PM . Diabetic retinopathy and blockade of renin-angiotensin system: new data from the DIRECT study programme. Eye 2010; 24: 1–6.
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular oedema. Ophthalmology 2010; 117: 1064–1077.
Michaelides M, Kaines A, Hamilton RD, Fraser-Bell S, Rajendram R, Quhill F et al. A prospective, randomised trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular oedema (BOLT study) 12 month data; report 2. Ophthalmology 2010; 117: 1078–1086.
The PKC-DRS Study Group. The effect of ruboxistaurin on visual loss in patients with moderately severe to very severe non-proliferative diabetic retinopathy. Initial results of the protein kinase C beta inhibitor retinopathy study (PKC-DRS) multicntre randomised clinical trial. Diabetes 2005; 54: 2188–2197.
Dodson PM, Galton DJ, Winder AF . Retinal vascular abnormalities in the hyperlipidemias. Trans Ophthalmol Soc UK 1981; 101: 17–21.
Orchard TJ, Dorman JS, Maser RE, Becker DJ, Ellis D, LaPorte RE et al. Factors associated with avoidance of severe complications after 25 yr of IDDMC. Pittsburgh Epidemiology of Diabetes Complications Study I. Diabetes Care 1990; 13: 741–747.
Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss. Early Treatment Diabetic Retinopathy Study Report 18. Invest Ophthalmol Vis Sci 1998; 39: 233–252.
Ucgun NI, Yildirim Z, Kilic N, Gursel E . The importance of serum lipids in exudative diabetic macular edema in type 2 diabetic patients. Ann NY Acad Sci 2007; 1100: 213–217.
Miljanovic B, Glynn RJ, Nathan DM, Manson JE, Schaumberg DA . A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes. Diabetes 2004; 53: 2883–2892.
Lyons TJ, Jenkins AJ, Zheng D, Lackland DT, McGee D, Garvey WT et al. Diabetic retinopathy and serum lipoprotein subclasses in the DCCT/EDIC cohort. Invest Ophthalmol Vis Sci 2004; 45: 910–918.
Dodson PM . Management of diabetic retinopathy: could lipid lowering be a worthwhile treatment modality? Eye 2009; 23: 997–1003.
Donaldson M, Dodson PM . Medical treatment of diabetic retinopathy. Eye 2003; 17: 550–562.
Colhoun HM, Bettridge DJ, Durrington PN, Hitman GA, Neil W, Andrew-Livingstone HA et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004; 364: 685–696.
Dodson PM . Medical treatment for diabetic retinopathy: do the FIELD microvascular study results support a role for lipid lowering? Practical Diabetes Int 2008; 25 (2): 76–79.
Duncan LJP, Cullen JF, Ireland JT, Nolan J, Clarke BF, Oliver MF . A three-year trial of atromid therapy in exudative diabetic retinopathy. Diabetes 1968; 17: 458–467.
Harrold BP, Marmion VJ, Gough KR . A double-blind controlled trial of clofibrate in the treatment of diabetic retinopathy. Diabetes 1969; 18: 285–291.
Cullen JF, Town SM, Cambell CJ . Double-blind trial of Atromid-S in exudative diabetic retinopathy. Trans Ophthalmol Soc UK 1974; 94: 554–562.
Keech AC, Mitchell P, Summanen PA, O'Day J, Davis TME, Moffitt MS et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 2007; 370: 1687–1697.
ACCORD Study Group and ACCORD Eye Study Group. Effects of medical therapies on retinopathy progression in type 2 diabetes. New Engl J Med 2010; 363: 233–244.
Cushman WC, Evans GW, Byington RP, Goff Jr DC, Grimm Jr RH, Cutler JA et al. Effects of intensive blood pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362: 1575–1585.
Ginsberg HN, Elam MB, Lovato LC, Crouse 3rd JR, Leiter LA, Linz P et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 2010; 362: 1563–1574.
Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L et al. Severe hypoglycaemia and risks of vascular events and death. N Engl J Med 2010; 363: 1410–1418.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008; 358: 2560–2572.
Enger C, Gately R, Ming EE, Niemcryk SJ, Williams L, McAfee AT . Pharmacoepidemiology safety study of fibrate and statin concomitant therapy. Am J Cardiol 2010; 106: 1594–1601.
Hiukka A, Maranghi M, Matikaimen N, Taskinen M-R . PPARa: an emerging therapeutic target in diabetic microvascular damage. Nat Rev Endocrinol 2010; 5: 454–463.
Playford DA, Watts GF, Best JD, Burke V . Effect of fenofibrate on brachial artery flow-mediated dilatation in type 2 diabetes mellitus. Am J Cardiol 2002; 90 (11): 1254–1257.
Israelian-Konaraki Z, Reaven PD . Peroxisome proliferator-activated receptor-alpha and atherosclerosis: from basic mechanisms to clinical implications. Cardiol Rev 2005; 13 (5): 240–246.
Tomizawa A, Hattori Y, Inoue T, Hattori S, Kasai K . Fenofibrate suppresses microvascular inflammation and apoptosis through adenosine monophosphate-activated protein kinase. Metabolism 2010 (E-pub ahead of print 25 June 2010; doi:10.1016/j.metabol.2010.04.020).
Kim J, Ahn J-H, Kim J-H, Yu Y-S, Kim H-S, Ha J et al. Fenofibrate regulates retinal endothelial cell survival through the AMPK signal transduction pathway. Exp Eye Res 2007; 84: 886–893.
Quresh M, Mark CG, Tien Y W . Management of diabetic retinopathy: a systematic review. JAMA 2007; 298 (8): 902–916.
White NH, Sun W, Cleary PA, Tamborlane WV, Danis RP, Hainsworth DP et al. Effect of Prior Intensive Therapy in Type 1 Diabetes on 10-Year Progression of Retinopathy in the DCCT/EDIC: Comparison of Adults and Adolescents. Diabetes 2010; 59: 1244–1253.
Klein BEK . Reduction in risk of progression of diabetic retinopathy. New Engl J Med 2010; 363: 287–288.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
ADW obtained consultative fee from Novartis and educational grant from Novo Nordisk, and PMD has served on advisory boards of Solvay, Takeda, and Novartis, and is principal investigator for the Protein Kinase C research programme for the UK.
Rights and permissions
About this article
Cite this article
Wright, A., Dodson, P. Medical management of diabetic retinopathy: fenofibrate and ACCORD Eye studies. Eye 25, 843–849 (2011). https://doi.org/10.1038/eye.2011.62
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.62
Keywords
This article is cited by
-
Cholesterol crystal formation is a unifying pathogenic mechanism in the development of diabetic retinopathy
Diabetologia (2023)
-
Current epidemiology of diabetic retinopathy in patients with type 1 diabetes: a national multicenter study in Brazil
BMC Public Health (2018)
-
Incidence of diabetes retinopathy and determinants of time to diabetes retinopathy among diabetes patients at Tikur Anbessa Hospital, Ethiopia: a retrospective follow up study
BMC Research Notes (2018)
-
Palmitic Acid Induces Müller Cell Inflammation that is Potentiated by Co-treatment with Glucose
Scientific Reports (2018)
-
Abnormal islet sphingolipid metabolism in type 1 diabetes
Diabetologia (2018)