Abstract
Objective
To evaluate the anatomical success and impact on visual acuity of 23-gauge, sutureless, phacovitrectomy, and intraocular gas tamponade for idiopathic macular hole surgery without face down posturing.
Methods
This was a non-randomised, observational, retrospective trial during the period from September 2007 to September 2008 with data collection of 40 eyes from 39 consecutive patients who underwent transconjunctival, sutureless, 23-gauge vitrectomy (TSV 23G), phacoemulsification, internal limiting membrane (ILM) peel, and intraocular gas tamponade (16% C2F6) for stage 3 and 4 idiopathic macular holes. Patients were instructed to neither posture face down nor supine post-operatively. All procedures were performed by a senior, single surgeon (RR).
Outcome measures
The primary outcome measure was anatomical closure rate of the macular hole. Secondary outcome measure was improvement in visual acuity.
Results
Macular holes were flat closed in 37 (92.5%) eyes at the first attempt. The remainder were eventually closed with Oxane HD tamponade without the need for face down posturing. Post-operatively, 22 out of 40 (55%) patients achieved >2 lines improvement in Snellen, visual acuity; 12 out of 40 (30%) patients achieved a 1 line improvement in Snellen, visual acuity; and 5 out of 40 (12.5%) patients’ visual acuities remained stable. One patient experienced a 1 line reduction in Snellen acuity owing to co-existing ocular surface disease.
Conclusion
Given the well-known advantages of sutureless, vitrectomy and paucity of post-operative hypotony and endophthalmitis, we feel that the 23-gauge instrumentarium is the method of choice when combined with phacoemulsification for non-posturing, macular hole surgery.
Similar content being viewed by others
Introduction
In 1991, Kelly and Wendel1 outlined their technique in repairing macular holes. This was the first reported, successful vitrectomy in ameliorating the signs associated with this ocular malady. The technique involved removal of the adherent cortical vitreous by a 20-gauge pars plana vitrectomy, followed by a gas fluid interchange with sulphur hexafluoride (SF6). To maintain adequate endotamponade, the authors advocated prone posturing for at least 1 week. Since then, numerous reports pervade the ophthalmic literature, questioning the need for such posturing.2, 3, 4, 5, 6, 7
In this paper, we present the results of patients who underwent combined, sutureless vitrectomy, phacoemulsification, internal limiting membrane (ILM) peeling, and gas tamponade to ameliorate the signs and symptoms of idiopathic macular hole.
Methods
This was a non-randomized, observational, retrospective trial during the period of September 2007 to September 2008, with data collection of consecutive patients who underwent transconjunctival, sutureless, 23-gauge vitrectomy (TSV 23G), phacoemulsification (with intraocular lens implantation), ILM peel, and C2F6 for idiopathic macular holes. Pre-operative data included gender, stage of hole, LogMAR visual acuity, crystalline lens status, and intraocular pressure (IOP). All patients received a comprehensive assessment pre-operatively that included both slitlamp and dilated fundus examination, in addition to ocular coherence tomographic assessment of their maculae. Grading of macular holes was in accordance with Gass’ classification.8
Surgical technique and procedure
The trocars and cannulas used were synergetics (M.I.S.S Ophthalmics Ltd, Corby, UK). The Bausch&Lomb Millenium vitrectomy system (Bausch & Lomb, Kingston-upon-Thames, UK), along with the Advanced Vitrectomy Enhancer from Midlabs (San Leandro, CA, USA), was used for all cases. The procedure included insertion of transconjunctival cannulas through the pars plana in the inferotemporal, superotemporal, and superonasal quadrants, respectively. The technique involved the insertion of a cannula using a bevelled trocar, as a single-step procedure. The conjunctiva was first displaced laterally, followed by an angled incision at 30–40 degrees to the corneo-scleral limbus, then turned perpendicular and inserted fully until the microcannula was in place. The inferotemporal port was inserted 3.5 mm from the limbus and the trocar was removed. The infusion line was connected to the cannula and started before inserting the superonasal and superotemporal cannulas. The cannulas were temporarily closed with plugs and infusion was clamped, while a superior bimanual corneal phacoemulsification was performed. After removing the cortex, the anterior chamber and the capsular bag were filled with viscoelastic. The plugs were then removed from the superior channels, and the infusion was restarted before vitrectomy. Pars plana vitrectomy using the 23-gauge high-speed vitrector (Millenium system) with a cut rate of 2400/min and an aspiration rate of 550 mm was performed. We used the Millenium, posterior vitrectomy system and the Adaptable Vitrectomy Enhancer AVE (Midlabs) and the BIOM system (Oculus GMBH, Wetzlar, Germany). Complete removal of the posterior vitreous and extensive removal of peripheral vitreous up to the vitreous base were achieved in all cases. The ILM was then stained with Trypan blue and peeled from the retina around the macular hole. A fluid/air exchange was then performed and the air line was clamped before the insertion of a foldable acrylic intraocular lens (SN60WF) into the capsular bag. Viscoelastic was aspirated from the anterior chamber and the air line was then unclamped before endotamponade with 16% perfluouroethane (C2F6) was performed.
All patients received a standard protocol of post-operative, topical antibiotic and anti-inflammatory agents. Both face down and supine posturing were actively discouraged.
All patients were reviewed on the first post-operative day by the same surgeon (RR). The gas fill was deemed adequate clinically as gas-retina contact below the inferior arcade, with the patient adopting an upright position in accordance with other clinicians.5
Results
During the study period, the outcomes of 40 eyes from 39 consecutive patients were analysed. Of these, 62.5% were female. The greater number of females represented here is in keeping with those observed in prevalence studies of the disease. All patients assessed on the first post-operative day were deemed to have sufficient endotamponade, as judged by the aforementioned clinical technique. Thus, face down posturing was not advocated in any of the patients. The follow-up period varied between 2 and 12 months (mean 7 months, SD±4.09). After the first post-operative day, all patients were assessed 2 and 6 weeks later. Both fundus biomicroscopy and ocular coherence tomography (OCT) were performed in all cases at each post-operative consultation.
Primary outcome
Macular holes were graded as stage 3 and 4 in 33 (82.5%) and 7 (17.5%) patients, respectively. Macular holes were flat closed (closed without foveal neurosensory retinal defect) in 37 (92.5%) eyes. The remainder required a second procedure using Oxane HD as the tamponade in order to achieve the primary outcome measure. Once again, this was achieved without the need for prone posturing.
Secondary outcome
Snellen, visual acuities were transcribed to the logarithm of the minimal angle of resolution (LogMAR) for statistical analysis. Thus, the LogMAR result was calculated by the following formula: log10 (1/Snellen fraction). Thus, a patient achieving a Snellen acuity of 6/6 post-operatively was equated to a LogMAR visual acuity of 0 (log10 (1/1). The pre-operative LogMAR visual acuity ranged from 0.3 to 1.9 (mean=0.81, SD±0.33). Post-operative LogMAR visual acuities ranged from 0 to 0.78 (mean=0.44, SD±0.24). Post-operatively, 55% (22 out of 40) of eyes achieved >2 lines improvement in Snellen acuity, 30% (12 out of 40) of eyes achieved a 1 line improvement in Snellen visual acuity, and 12.5% (5 out of 40) of eyes remained stable visually (see Figure 1). One patient experienced a single line reduction in Snellen visual acuity and this was attributed to co-existing ocular surface disease.
Complications
There were no intra-operative complications. The only post-operative complication detected was posterior capsular opacification, which occurred in 12.5% (5 out of 40) of eyes. All received uneventful Neodymium/ytrrium aluminium garnet (Nd/YAG) laser capsulotomies. Notably, there were no ocular, hypertensive, or hypotensive events post-operatively.
Discussion
After the introduction of macular hole surgery, prone posturing was considered to be an essential component for the successful closure of such pathology. The difficulty in adopting such a posture was highlighted by Verma et al,9 who uncovered that such positioning was only maintained in an average of 38% of patients in their study group without adversely affecting visual and anatomical outcomes. More importantly, prone posturing itself is not without its complications. Both ulnar neuropathies10 and acute IOP spikes11 have been reported. It also has a deleterious effect on the patient's quality of life and, as such, often precludes some patients from undergoing surgery.
Proponents of Tornambe's ‘hydration hypothesis’,12 whereby the reduction in intramacular fluid through the retinal pigment epithelial pump is an essential component for successful anatomical closure, support the notion that the endotomaponade should be large enough so as to ensure dessication of the macular area. Failure to prevent the newly formed post-vitrectomy aqueous humour to come in contact during a critical post-operative contact period may interfere with the reparative process. It is for this reason, in addition to the supposition that the perpendicular forces may either displace subretinal fluid away from the macula and provide counter pressure to the tractional force,13 that face down or prone posturing has been advocated for many years. The latter concept is often referred to as the ‘floatation force effect’.
It is worthy of note that the ‘floatation force effect’ may be present only if the gas bubble is immersed in fluid. Furthermore, a bubble that is above a fluid level exerts no buoyancy force.14 The main forces present are those at the gas-retina interface, which are not dependent on posture.
Table 1 summarizes the results of studies analysing macular hole closure rates without face down posturing using different instrumentaria and endotamponade agents, with and without combined phacoemulsification. Our primary closure rate of 92.5% compares favourably with others and adds further support to the notion that face down posturing is not a prerequisite to successful macular hole surgery.
Although there are numerous studies demonstrating comparable hole closure rates with no prone posturing in patients receiving both 20-gauge sutured vitrectomy and its smaller, sutureless 25-gauge counterpart, the surgeon elected to use the 23-gauge system as originally described by Eckardt.15 Sutureless surgery affords distinct benefits to both the patient and the surgeon. Benefits to the patient include a reduction in inflammation with shortened recovery time, together with a reduced likelihood of post-operative, suture-related astigmatism. A reduction in operative time may be achieved using this technique, thus benefiting the surgeon. This study is one of the first in a large series on 23-gauge surgery for macular hole repair in literature.
Although the 25-gauge system has been used in non-posturing macular hole surgery, proponents of the 23-gauge system argue that, owing to the higher flow rates and greater tensile strength, a faster vitrectomy may be achieved with the larger system. Furthermore, the greater tensile strength of the 23-gauge system is associated with a reduced risk of instrument breakage during ocular movements compared with its 25-gauge counterpart.16 Thus, the 23-gauge instrumentarium offers the advantages of sutureless surgery in combination with the advantages of the 20-gauge system. Peripheral gel trimming up to the vitreous base was performed without any compromise on the extent of vitrectomy compared with 20-gauge vitrectomy. This is essential in non-posturing macular hole surgery to achieve a larger gas bubble in the vitreous cavity, which may be tedious with the currently available 25-gauge systems.
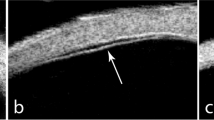
When using the 23-gauge vitrectomy system, we used an angled, transconjunctival sclerostomy incision. Concerns have been raised regarding the increased risk of post-operative endophthalmitis associated with sutureless vitrectomy. One study demonstrated a significant increase in the post-operative endophthalmitis rate in patients who underwent vitrectomy using the 25-gauge system compared with its 20-gauge counterpart.17 This has been reported by other authors.18 Notwithstanding, Shimada et al19 revealed no statistical difference in post-operative endophthalmitis rates between their patients who underwent 20- and 25-gauge vitrectomies in their cohort. The authors emphasized the importance of performing angled incisions in keeping the risk of acquiring this devastating complication to a minimum. Moreover, an ocular coherence tomographic and histopathological study demonstrated that angled incisions offer superior wound apposition under dynamic IOP conditions.20 In addition, anterior segment OCT has demonstrated, in vivo, adequate wound apposition on the first post-operative day with oblique 23-gauge sclerostomy incisions.21 It is noteworthy that, in keeping with our results, there are no published studies demonstrating an increased risk of endophthalmitis associated with the 23-gauge system.
Hypotony is a well-documented complication of 25-gauge transconjunctival sutureless vitrectomy.18 In a recent retrospective review of risk factors associated with sclerostomy leakage and post-operative hypotony in patients receiving vitrectomy with the 23-gauge system, Woo et al22 uncovered the following risk factors: age <50 years, vitreous base dissection, and previous vitrectomy. The authors conjectured that the increased scleral rigidity of older eyes reduces the risk of post-operative leakage. Patients who have their vitreous base dissection may be more prone to leakage either because of the lack of tamponade effect at the sclerostomy site or the increased manipulation of the wound through the microcannula when attempting to reach the base. The same authors noted the post-operative hypotony rate at day 1 to be 3.8% on the first post-operative day, with IOPs returning to baseline levels in all cases by the end of the first post-operative week. No post-operative hypotony was revealed in our cohort. No inadvertent loss of gas endotamponade through leakage from the sclerostomy sites was noted, as evidenced by the adequate gas endotamponade fill on the first post-operative day, together with the lack of post-operative hypotony. These findings may be attributed to angled sclerostomies.
Peeling of the ILM was performed in all cases and its implementation has been advocated as an essential step leading to successful closure of macular holes23 and as a preventative measure for the reopening of holes.24 Notwithstanding, the exact mechanism underlying the success remains equivocal. Some investigators argue that it is because of a reduction in vitreoretinal tangential traction;23 others support the notion that glial proliferation is stimulated, resulting in an increased macular hole closure rate.25 Its inclusion may be more important when treating stage 3 or 4 holes without face down posturing, as demonstrated by our cohort.
Cataract is the most common post-operative complication of macular hole surgery.26 Indeed, this fact was highlighted in the study by Thompson et al27 in which 71% of eyes that underwent such surgery required cataract extraction within the first 2 years after their initial procedure. It is also noteworthy that the incidence of posterior subcapsular lens opacities was higher in those patients who did not posture compared with those who did, following macular hole surgery in the study by Tranos et al.4 Two further points regarding cataract surgery performed as a separate procedure merit discussion. First, because of a paucity of vitreous support in a vitrectomized eye, there is an increased risk of zonular or posterior capsular insult. Second, there are numerous studies that highlight the increased re-opening rate of macular holes following separate cataract extraction.28 It is for these reasons, together with the added convenience of a one-step procedure to the patient, that macular hole repair was combined with phacoemulsification in all cases.
The posterior, capsular opacification rate within 3 months of the procedure in our cohort was 12.5% (5 out of the 40 eyes). Simcock and Scalia3 noted their rate to be slightly higher (32%). Others have found lower rates.5 It has been purported that the underlying mechanism is related to the extended time that the gas is allowed to make contact with the posterior capsule.
Eckardt29 has recently demonstrated that macular holes remain closed after 24 h of short-acting endotamponades such as gas. Although further studies are warranted, the use of short-acting agents may reduce the rate of posterior capsular opacification. The reduced anterior segment inflammation associated with phacoemulsification, combined with transconjunctival, microincisional surgery, may have contributed to the lower incidence of posterior capsular opacification.
We recognize that the lack of a posture control group and retrospective nature of the study are the main limitations of our study. However, this study provides further support to the abolition of face down posturing in patients undergoing macular hole surgery. Importantly, as more centres adopt a non-posturing post-operative regimen with successful results, it may be unethical to perform a randomized control trial.11 Furthermore, this is the first study to show that sutureless, 23-gauge vitrectomy combined with phacoemulsification, ILM peeling, and C2F6 endotamponade achieves excellent results that are, at least, comparable to those achieved with conventional techniques without prone posturing. We have demonstrated that by implementing angled sclerostomies, one is able to retain an adequate gas endotamponade, obviating the need for prone posturing following surgery, in addition to negating the risks of post-operative endophthalmitis or hypotony.
Finally, although posterior, capsular opacification was observed in a small but significant number, we believe that the relative low complication rate associated with Nd/YAG laser capsulotomy and the relative ease of performing the technique not only offset the greater complication risk associated with phacoemulsification performed in a vitrectomized eye but also resulted in a more expedient visual rehabilitation time in these patients.
We therefore advocate the use of combining phacoemusification with 23-gauge vitrectomy in all patients undergoing macular hole surgery.

Conflict of interest
The authors declare no conflict of interest.
References
Kelly NE, Wendel RT . Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 1991; 109 (5): 654–659.
Tornambe PE, Poliner LS, Grote K . Macular hole surgery without face-down positioning. A pilot study. Retina 1997; 17: 179–185.
Simcock PR, Scalia S . Phacovitrectomy without prone posture for full thickness macular holes. Br J Ophthalmol 2001; 85: 1316–1319.
Tranos PG, Peter NM, Nath R, Singh M, Dimitrakos S, Charteris D et al. Macular hole surgery without prone posturing. Eye 2007; 21: 802–806.
Dhawahir-Scala FE, Maino A, Saha K, Mokashi AA, McLauchlan R, Charles S . To posture of not to posture after macular hole surgery. Retina 2008; 28: 60–65.
Carvounis PE, Kopel AC, Kuhl DP, Heffez J, Pepple K, Holz ER . 25 Gauge vitrectomy using sulfur hexafluoride and no prone positioning for repair of macular holes. Retina 2008; 28: 1188–1192.
Madgula IM, Costen M . Functional outcome and patient preferences following combined phaco-vitrectomy for macular hole without prone posturing. Eye 2008; 22: 1050–1053.
Gass JDM . Reappraisal of biomicroscopic classification of stages of development of macular hole. Am J Ophthalmol 1995; 119: 752–759.
Verma D, Jalabi MW, Watts WG, Naylor G . Evaluation of posturing in macular hole surgery. Eye 2002; 16: 701–704.
Holekamp NM, Meredith TA, Landers MB, Snyder WB, Thompson JT, Berman AJ et al. Ulnar neuropathy as a complication of macular hole surgery. Arch Ophthalmol 1999; 17 (12): 1607–1610.
Gupta D . Face-down posturing after macular hole surgery: a review. Retina 2009; 29 (4): 430–443.
Tornambe PE . Macular hole genesis: the hydration theory. Retina 2003; 23 (3): 421–424.
Berger JW, Brucker AJ . The magnitude of the bubble buoyant pressure: implications for macular hole surgery. Retina 1998; 18 (1): 84–86; author reply 86–88.
Stopa M, Lincoff A, Lincoff H . Analysis of forces acting upon submacular hemorrhage in pneumatic displacement. Retina 2007; 27 (3): 370–374.
Eckardt C . Transconjunctival sutureless 23-gauge vitrectomy. Retina 2005; 25: 208–211.
Lott MN, Manning MH, Singh J, Zhang H, Singh H, Marcus DM . 23 Gauge Vitrectomy in 100 eyes: short term visual outcomes and complications. Retina 2008; 28: 1193–1200.
Scott IU, Flynn Jr HW, Dev S, Shaikh S, Mittra RA, Arevalo JF et al. Endophthalimitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina 2008; 28 (1): 138–142.
Chen E . 25—Gauge transconjunctival sutureless vitrectomy. Curr Opin Ophthalmol 2007; 18: 188–193.
Shimada H, Nakashizuka H, Hattori T, Mori R, Mizutani Y, Yuzawa M . Incidence of endophthalmitis after 20- and 25-gauge vitrectomy causes and prevention. Ophthalmology 2008; 115 (12): 2215–2220.
Taban M, Ventura AA, Sharma S, Kaiser PK . Dynamic evaluation of sutureless vitrectomy wounds: an optical coherence tomography and histopathology study. Ophthalmology 2008; 115 (12): 2221–2228.
Taban M, Sharma S, Ventura AA, Kaiser PK . Evaluation of wound closure in oblique 23-gauge sutureless sclerotomies with visante optical coherence tomography. Am J Ophthalmol 2009; 147 (1): 101–107.
Woo SJ, Park KH, Hwang JM, Kim JH, Yu YS, Chung H . Risk factors associated with sclerotomy leakage and postoperative hypotony after 23 gauge transconjunctival sutureless vitrectomy. Retina 2009; 29: 456–463.
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R et al. Internal limiting membrane removal during macular surgery: results of a multicenter retrospective study. Ophthalmology 2006; 113: 1401–1410.
Kumagi K, Furukawa M, Ogino N, Uemura A, Demizu S, Larson E . Vitreous surgery with and without internal limiting membrane peeling for macular hole repair. Retina 2004; 24: 721–727.
Uemoto R, Yamamoto S, Takeuchi S . Epimacular proliferative response following internal limiting membrane peeling for idiopathic macular holes. Graefes Arch Clin Exp Ophth 2004; 242: 1777–1780.
Ellis JD, Malik TY, Lambert MA, Barr A, Baines PS . Surgery for full thickness macular holes with short duration prone posturing: results of a pilot study. Eye 2000; 14: 307–312.
Thompson JT, Glaser BM, Sjaarda RN, Murphy RP . Progression of nuclear sclerosis and long term visual results of vitrectomy with transforming growth factor beta-2 for macular holes. Am J Ophthalmol 1995; 119: 48–54.
Duker JS, Wendel R, Patel AC, Puliafito CA . Late re-opening of macular holes after initially successful treatment with vitreous surgery. Ophthalmology 1994; 101: 1373–1378.
Eckardt C, Eckert T, Eckardt U, Porkert U, Gesser C . Macular hole surgery with air tamponade and optical coherence tomography-based duration of face-down posturing. Retina 2008; 28: 1087–1096.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heath, G., Rahman, R. Combined 23-gauge, sutureless transconjunctival vitrectomy with phacoemulsification without face down posturing for the repair of idiopathic macular holes. Eye 24, 214–221 (2010). https://doi.org/10.1038/eye.2009.292
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.292
Keywords
This article is cited by
-
Outcome of 2 cc pure sulfur hexafluoride gas tamponade for macular hole surgery
BMC Ophthalmology (2016)
-
Pilot randomised controlled trial of face-down posturing following phacovitrectomy for macular hole
Eye (2012)
-
Femtosecond laser assisted cataract surgery in phacovitrectomy
Graefe's Archive for Clinical and Experimental Ophthalmology (2012)