Abstract
Purpose
To evaluate the results of bilateral paediatric cataract surgery in the same session with a focus on patient selection criteria, operative guidelines, and controversial issues.
Setting
Departments of Ophthalmology, İnönü University Turgut Özal Medical Center (Malatya) and Fatih University Hospital (Ankara, Turkey).
Methods
This retrospective noncomparative case series comprised 39 children (78 eyes), who underwent bilateral cataract surgery and/or primary or secondary IOL implantation in one sitting. Ten patients had bilateral lensectomy-primary posterior capsulotomy-anterior vitrectomy, and the remaining 29 patients had bilateral IOL implantation either primarily (20 cases) at the time of cataract extraction or secondarily for aphakic correction (9 cases). Both eyes were treated as two separate but consecutive surgeries in the same session. Maximum possible care was taken to ensure surgical asepsis.
Results
Age at surgery ranged from 2 months to 17 years. Average follow-up was 12 months. No serious intraoperative or postoperative complications occurred leading to permanent vision loss. During the last follow-up, 91% of eyes tested had a visual acuity of 20/40 or better.
Conclusion
Bilateral paediatric cataract surgery in one session may be a safe and useful approach alternative to sequential surgery in selected patients, if operative guidelines and surgical asepsis are strictly followed.
Similar content being viewed by others
Introduction
Majority of childhood cataracts occur in both eyes,1 and estimated prevalence of childhood blindness from bilateral cataract is probably increasing particularly in the developing world due to higher birth rate and lower availability of health resources.2, 3
However, there has still been a paucity of reports (only four small series4, 5, 6, 7 reporting a total of 63 cases) on bilateral paediatric cataract surgery (BPCS) in the same session,8 whereas it is more common in adult cataracts.9 This is mainly because of the more challenging nature of paediatric cataract surgery, along with the fear of bilateral involvement of catastrophic complications, particularly endophthalmitis. BPCS in one session still remains a controversial approach, despite the significant reduction of complications with the improvement in surgical equipment, disposables, and refinements in the surgical technique.8 Conversely, as there is no risk-free surgical procedure, any ophthalmic surgical approach should require balancing the relevant risks and benefits in each step. Therefore, an ophthalmic surgeon encountering a visually significant bilateral paediatric cataract should weigh the potency of relevant risks against the advantages of the so-called bilateral simultaneous approach in light of evidences in the literature and his personal experiences.
Therefore, we retrospectively evaluated the results of BPCS in the same session, and aimed to discuss the relevant topics, including patient selection criteria, operative guidelines, and controversies regarding this issue.
Patients and methods
Medical records of paediatric patients who underwent BPCS in the same session between 2000 and 2007 were reviewed retrospectively. Data recorded included age at the time of cataract surgery; etiology of the cataract; presence of associated ocular and systemic pathologies; details of the surgical technique with intraoperative complications; IOL type and power; postoperative examination findings, including visual acuity and refraction, along with postoperative complications, such as fibrinoid reaction, posterior capsule opacification (PCO), glaucoma, nystagmus, and strabismus. IOL power calculation was based on the SRK II formula with a target under-correction modified by the patient's age.10
Since BPCS in a single session is not a routine procedure, the study adhered to the tenets of the Declaration of Helsinki, and the parents received a detailed explanation of the possible risks and advantages of the procedure and were an integral part of the decision to perform this approach.
Before the surgery, paediatric patients at increased risk of postoperative complications, particularly endophthalmitis, were excluded to increase safety and satisfaction.8 Thus, children with relevant risk factors, including infections of ocular surface and adnexia (eg, blepharitis, conjunctivitis, nasolacrimal duct obstruction, and upper respiratory tract infection) and immunosuppression, were not operated to minimize the risk of endophthalmitis. As a main requirement for BPCS in the same session, strict surgical aseptic guidelines were followed during the operation on both eyes, and each eye was treated as a completely separated procedure. Briefly, eyes were prepared with meticulous aseptic technique, the operative staff rescrubbed and used fresh gowns and gloves, and a fresh set of solution with a new or re-sterilized set of surgical instruments was used in the second eye.
All surgeries were performed by anterior segment approach, most often through scleral tunnel incision and, less frequently, through limbal or clear corneal incisions along with can-opener capsulotomy, manual continuous curvilinear capsulorhexis (CCC), or anterior vitrectorhexis. Anterior chamber maintainer is also used, when required. The cataracts were aspirated using irrigation–aspiration handpiece, phacoemulsification, or an ocutome probe. Primary or secondary IOL implantation in the capsular bag, if possible, or ciliary sulcus was performed in children over 1 year of age. In younger children, primary posterior capsulotomy (PPC) alone or combined with anterior vitrectomy was also carried out before IOL placement. A neodymium:YAG (Nd:YAG) laser posterior capsulotomy, when required, was performed postoperatively in older children.
The incisions were closed with 10/0 monofilament nylon or 8/0 vicryl sutures. The operations were completed with subconjunctival dexamethasone and gentamicin injections separately. Eyes were closed with a patch and eye shield. They were postoperatively maintained on a combination of antibiotic, steroid, and mydriatic eye drops (when necessary). Patients were also managed with optical rehabilitation by spectacles, if required.
Results
Data from 78 eyes of 39 paediatric patients who underwent bilateral cataract surgery and/or IOL implantation in the same session are summarized in Tables 1, 2, 3, 4. The presented group of patients constitutes the majority (about 70%) of BPCSs performed in the same period of time.
Table 1 shows the characteristics of the patients. The mean age at the time of cataract surgery was 6 years (range, 2 months–17 years). Of the total patients, 14 (36%) were less than or equal to 2 years of age, and 13 (33%) were older than 7 years.
In the group of 30 cases who underwent bilateral cataract extraction with or without primary IOL implantation, 11 (37%) had nuclear or complete cataracts in both eyes. Majority of the remaining 19 cases (63%) comprised lamellar (10 patients) or cortical (3 patients) cataracts.
Preoperative conditions associated with bilateral cataract or aphakia included strabismus in 12 eyes of 10 cases (26%) and nystagmus in 7 cases (18%). Patients with preoperative strabismus or nystagmus had either dense congenital or developmental cataracts operated on between 5 months and 11 years or underwent secondary IOL implantation at an average age of 7 years after cataract extraction in the first year of life. Postoperatively, strabismus markedly resolved in both eyes of two patients and nystagmus in one case, all with dense congenital cataracts, spontaneously. Two patients had systemic diagnosis of cerebral palcy and were operated on for bilateral complete cataracts at the age of 6 months and 6 years, respectively.
Ten patients with a mean age of 6 months (range, 2–18 months) underwent bilateral lensectomy-PPC-anterior vitrectomy, and were optically corrected with aphakic spectacles. The remaining 29 patients had bilateral IOL implantation either primarily at the time of cataract extraction (20 cases) or secondarily for aphakic correction (9 cases) (Table 2) The mean age at the time of IOL implantation was 7 years for primary IOLs (range, 18 months–15 years) and 9 years for secondary IOLs (range, 2–17 years). Among those with secondary implantation, the average elapsed time since cataract surgery was 6 years (range, 1–13 years). In those with primary IOL implantation, PPC was performed bilaterally in 10 cases with accompanied anterior vitrectomy in 5 of them. Overall, PMMA IOLs were used in 21 eyes of 14 patients implanted primarily and in 18 eyes of 9 patients implanted secondarily. Acrylic foldable lenses were used in 19 eyes of 13 patients with primary implantations. Seven eyes of seven patients receiving primary IOLs had PMMA IOLs in the ciliary sulcus because of inadequate capsular support. IOL powers ranged from +14 to +30 D (diopters).
Data for the last refractions available (in spherical equivalents) in the pseudophakic patients revealed an average postoperative refraction of −0.56±2.35 D (range, −4 to +6 D) at an average follow-up period of 11±10 months (3–54) (Table 2). In 72% eyes, the refraction was within ±2 D of the goal. There were a few patients (8 eyes of 5 patients) in whom major deviations from the goal occurred, up to −4.00 D. The mean anisometropia between the fellow eyes was 1.01±0.82 D (maximum 2.50 D). In 86% of the pseudophakic patients, anisometropia was equal or less than 2 D.
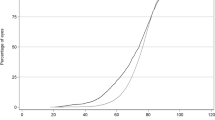
Visual results were generally satisfactory (Table 3). Of the 23 patients with measurable vision, 42 eyes (91%) had 20/40 vision or better at last follow-up. Other younger patients unable to cooperate with formal vision testing had bilateral central, steady, and maintained (CSM) vision or could fix and follow (FF) bilaterally by the fixation method.
There was no major postoperative complication observed with a resultant permanent visual loss, including retinal detachment and endophthalmitis (Table 4). However, three eyes required additional surgical procedures using vitrectomy system with ocutome probe due to severe fibrinoid reactions and hyphema leading to optic capture plus IOL decentralization, obscuration of the visual axis, and pupillary block glaucoma in the early postoperative period. Of the 20 eyes with intact posterior capsules, only 5 eyes with PCO required YAG laser posterior capsulotomy in the late postoperative period. Other complications listed in Table 4 were successfully managed medically.
Discussion
There is still an ongoing debate on the issue of BPCS in the same session.8 In the view of literature data showing a limited number of BPCSs performed in the same sitting,8 one may readily consider it as an option that appears to be seldom used because of high risk of some catastrophic complications compared with sequential surgery. However, the major concern against BPCS in the same session is the potential risk or fear of bilateral endophthalmitis, still the foremost deterrent to this approach.3, 8 Reports on endophthalmitis after adult cataract surgery do not show an increased incidence following bilateral simultaneous approach compared with unilateral cataract surgery,9 and, overall, the incidence of endophthalmitis following modern cataract surgery has been significantly reduced with the advent of microsurgical technique, preoperative measures, and intracameral prophylactic antibiotic use.11, 12 However, there is limited data available on the prevalence of endophthalmitis after paediatric cataract surgery, estimating its incidence as 0.07–0.45 percent,13, 14 comparable to those in unilateral adult cataract surgery. Furthermore, neither has any case of endophthalmitis been previously reported after BPCS in one session, nor have we encountered any in our study population. However, this may not be considered as valid evidence because of the rarity of this problem15 and the lower prevalence of paediatric cataract surgery. Additionally, a younger child in an amblyopia-susceptible period with bilateral significant cataract should have two consecutive surgeries with the shortest possible interval such as a few days, whereas this brief period cannot guarantee for eliminating the risk of bilateral acute-onset endophthalmitis that may not be diagnosed up to 21 days postoperatively.16 Although there is no objective reason to assume an increased risk of endophthalmitis following the simultaneous approach in light of evidences, and since prophylactic intracameral antibiotic use can also markedly reduce the incidence of endophthalmitis,12 paediatric patients at a high risk of endophthalmitis (such as infections of ocular surface and adnexia, upper respiratory tract infection, and immunosuppression) should be excluded from the simultaneous bilateral cataract surgery, strict surgical aseptic guidelines should be followed in the operating room, and finally each eye should be treated as a completely separate procedure to minimize the risk of endophthalmitis. Conversely, considering the possibility of clusters of endophthalmitis cases due to contaminated operating room air, intraocular irrigation fluids, or water used to rinse instruments, BPCS in the same session should be considered in selected cases regarding the risk of general anaesthesia and amblyopia, the patient and family compliance, and reserved for modern operating theatres in case of strict surgical aseptic conditions preserved for each eye separately. Since the behaviour of the child (ie, swimming or other high-risk activities, even rubbing) and the parents (ie, poor compliance with drops) may also be another risk factor for endophthalmitis after cataract surgery, the surgeon should explain and discuss these issues adequately with the family before the operation, and should not hesitate to cancel the bilateral simultaneous surgery unless fully satisfied in this respect. Also, the intervals of postoperative visits should be shorter, if required, with additional examinations in the early postoperative period to provide more prophylactic measures against endophthalmitis risk and to control the family and the patient more closely.
Additionally, if the first eye surgery is complicated, with a major problem such as marked iris trauma with hyphema, large nuclear remnants, or dropped nucleus in to the vitreous, the fellow-eye surgery should be postponed to a later time.8, 17 In the presented group of paediatric patients, no serious intraoperative complications occurred in the first eye that necessitated cancelling surgery in the second eye.
Another important concern against BPCS in the same session is the inability to make necessary adjustments in IOL power selection and surgical technique for the fellow eye to reduce the risk of marked anisometropia and bilateral involvement of major complications such as severe corneal oedema and fibrinous reaction occluding the visual axis. It is obvious that in sequential bilateral cataract surgery, one can change IOL power for the second eye depending on the refractive accuracy in the first operated eye.17, 18 However, in paediatric patients with bilateral cataracts, this idea should cautiously be regarded, as the refractive stability of younger eyes may take a few months postoperatively,19 implying far beyond our limitation for the interval between the surgeries on both eyes in the amblyopia susceptible period. Conversely, modern biometry machines along with current biometric formulae including SRK-II, and comprehensive IOL technology can allow us to reach the targeted refraction within an acceptable range in paediatric pseudophakic eyes,20 thereby decreasing the risk of marked anisometropia in bilateral paediatric IOL placement in the same session. In addition, ocular growth will presumably be comparable in the fellow pseudophakic eyes, and residual refractive errors can easily be compensated with spectacles. Data from the studies of simultaneous bilateral adult cataract surgery9, 21 also do not indicate a significant amount of refractive surprise in the second eye. In the present study, the degree of anisometropia was within 2 D in all but four of the pseudophakic patients, and thus could be effectively compensated by spectacle correction alone to prevent ambliopia.22 These four cases had 2.5 D of anisometropia, but no patient had anisometropic amblyopia postoperatively after spectacle overcorrection.
Due to the breakdown of the immature blood–aqueous barrier in paediatric cataract surgery, severe postoperative fibrinoid reaction may occur with resultant occlusion of visual axis, thereby impairing visual rehabilitation and aggravating amblyopia. Conversely, modern cataract surgical techniques and equipments, such as anterior chamber maintainer (ACM) and vitrectomy machines with ocutome probe, along with some pharmacological agents such as intracameral heparin, showed great promise in this concern.23 However, paediatric patients with increased risk of severe postoperative fibrinoid reaction (ie, juvenile rheumatoid arthritis, diabetes) should not be considered for the simultaneous approach. We did not observe an intense fibrinoid reaction with permanent visual obstruction in the presented group of selected patients, except in three eyes undergoing secondary surgery by modern vitrectomy system.
Since the cumulative risk of mortality and morbidity from general anaesthesia is increases with a decrease in age and repetitive anaesthesia,24, 25 BPCS in the same session should be preferred in handicapped children with higher anaesthesia risk, and may also be considered in healthy selected cases (those with no exclusion criteria) if the patient and family compliances are expected to be good and the family rejects repetitive anaesthesia after being fully informed about the risks and benefits of the simultaneous surgery. Both eyes of all children in this study, including two with cerebral palcy and one with homocystinuria, were operated on in a single session by experienced surgeons with no significant anaesthetic morbidity or mortality.
In younger children, particularly neonates and infants, early visual deprivation with dense cataracts is commonly encountered as a major obstacle to good vision. Therefore, early cataract surgery is recommended for those with no fundus visualization to reach satisfactory visual improvement.26, 27, 28 Reports of bilateral congenital cataract surgery have proposed that good visual outcomes can be achieved if the surgeries are not associated with preoperative nystagmus and are completed before 10 weeks of age with short intervals such as 2–6 days between surgeries on fellow eyes.26, 27 However, even such short intervals may not guarantee for preventing deprivation amblyopia or endophthalmitis in infants and younger children. Furthermore, bilateral congenital cataract surgery in the same session may result in a higher rate of recovery from nystagmus.7 Since we had no chance of early diagnoses, close follow-up, and thus early operation on dense congenital or developmental cataracts in our patient group, only one case with nystagmus and two with strabismus present preoperatively showed a marked improvement in the ocular alignment and nystagmus amplitude postoperatively. However, the visual results obtained in our series of paediatric patients who underwent cataract surgery on both eyes in the same sitting were generally satisfactory, as a final visual acuity of 20/40 or better was achieved in 91% patients tested, which is comparable to the previous reports of bilateral paediatric IOL implantation by sequential surgical approach.29, 30
There is no doubt that prompt optical correction of bilateral paediatric aphakia with spectacle or contact lens fitting, or primary IOL implantation, is very important for the success of visual rehabilitation, yet all these measures have both advantages and limitations.29, 30, 31 Therefore, choosing the optimal method for each patient should be made on individual basis by considering the patient's age, presence of large amplitude nystagmus, behavioural abnormalities, socioeconomical status, and compliance of the family. Despite some historical arguments against bilateral IOL implantation in younger children,32 it has really become a standard for the management of bilateral paediatric aphakia beyond infancy, and there seems to be a trend for decreasing the age limit of paediatric IOL implantation to the first year of life.29, 30, 33 In accordance with our experience, cumulative information about the family compliance, and demographic structure, we generally prefer to implant IOL as a method of optical correction in paediatric aphakia beyond 1 year of age, which we consider rather helpful for visual rehabilitation and socioeconomical aspects. For those in the first year of life, our choice of aphakic correction in bilateral cases, as in this study, is usually to advice spectacles.
In the new millennium, paediatric cataract continues to be a major cause of treatable childhood blindness throughout the world, particularly in developing countries, thus representing a common health problem with respect to the patient's morbidity, economic loss, and social burden.3, 34 Therefore, any attempt to save the light of more and more children as early as possible is obviously foremost important for controlling childhood blindness. In this regard, BPCS in the same session apparently has some advantages including visual rehabilitation of both eyes in one step, thereby reducing the working time and number of visits twofolds and increasing the effective use of surgical equipment. Although the simultaneous approach for BPCS is cost-effective, and economical prospects cannot be ignored, particularly in the developing world where medical resources are limited and ophthalmic and anaesthesiology staff are evenly distributed,3 the priority of clinical judgement for the patient selection individually should always be kept in mind, which means the issues of cost and travels should not be considered as the inclusion criteria.
Conclusion
BPCS in the same sitting should only be performed under strict aseptic surgical conditions, in modern operating rooms, and by experienced surgeons. Each eye should be treated as a completely separate procedure. The bilateral simultaneous approach, not a routine procedure, should be preferred in children with high general anaesthesia risk and no increased risk of postoperative endophthalmitis, or other visually compromising complications such as fibrinoid reaction. It should also be considered in cases of increased amblyopia risk when the family and patient compliances are expected to be good, or in cases when a compliant family rejects the repetitive general anaesthesia after being fully informed about the simultaneous approach. The surgeon should also consider each case individually to make a justified decision, and should not hesitate to cancel the operation on the second eye if the first one has a serious complication, such as marked hyphema, dropped nucleus into the vitreous, and vitreous haemorrhage.
Despite the limited number of patients and the follow-up period, these preliminary results suggest that BPCS in the same session is a safe and useful approach in carefully selected cases under good surgical conditions, yet requires larger and comparative studies with longer follow-ups.
References
Rahi JS, Dezateaux C . British Congenital Cataract Interest Group. Measuring and interpreting the incidence of congenital ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci 2001; 42 (7): 1444–1448.
Foster A, Gilbert C, Raji J . Epidemiology of cataract in childhood. A global perspective. J Cataract Refract Surg 1997; 23: 601–604.
Wilson ME, Pandey SK, Thakur J . Paediatric cataract blindness in the developing world: surgical techniques and intraocular lenses in the new millennium. Br J Ophthalmol 2003; 87: 14–19.
Guo S, Nelson LB, Calhoun J, Levin A . Simultaneous surgery for bilateral congenital cataracts. J Pediatr Ophthalmol Strabismus 1990; 27: 23–25.
Zwaan J . Simultaneous surgery for bilateral pediatric cataracts. Ophthalmic Surg Lasers 1996; 27: 15–20.
Totan Y, Bayramlar H, Cekic O, Aydin E, Erten A, Daglioglu MC . Bilateral cataract surgery in adult and pediatric patients in a single session. J Cataract Refract Surg 2000; 26: 1008–1011.
Yagasaki T, Sato M, Awaya S, Nakamura N . Changes in nystagmus after simultaneous surgery for bilateral congenital cataracts. Jpn J Ophthalmol 1993; 37: 330–338.
Totan Y . Bilateral pediatric cataract surgery in one session. In: Pandey SK, Billson FA (eds). Step by Step Pediatric Cataract Surgery. Jaypee Brothers Medical Publishers (P) Ltd: New Delhi, 2005, Chapter 5: pp 91–116.
Arshinoff SA, Strube YNJ, Yagev R . Simultaneous bilateral cataract surgery. J Cataract Refract Surg 2003; 29: 1281–1291.
Dahan E . Pediatric cataract-intraocular lens surgery: surgical techniques, complications and management. In: Pandey SK, Billson FA (eds). Step by Step Pediatric Cataract Surgery. Jaypee Brothers Medical Publishers (P) Ltd: New Delhi, 2005, Chapter 3: pp 41–68.
Aaberg TM, Flynn HW, Schiffman J, Newton J . Nasocomial acute-onset postoperative endophthalmitis survey: a 10 year review of incidence and outcomes. Ophthalmology 1998; 105: 1004–1010.
Endophthalmitis Study Group, European Society of Cataract and Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg 2007; 33 (6): 978–988.
Good WV, Hing S, Irvine AR, Hoyt CS, Taylor DSI . Postoperative endophthalmitis in children following cataract surgery. J Pediatr Ophthalmol Strabismus 1990; 27: 283–285.
Wheeler DT, Stager DR, Weakley DR . Endophthalmitis following pediatric intraocular surgery for congenital cataracts and congenital glaucoma. J Pediatr Ophthalmol Strabismus 1992; 29: 139–141.
Javitt JC . When does the failure to find a difference mean that there is none? Arch Ophthalmol 1989; 107: 1034–1040.
Miller JJ, Scott IU, Flynn HW, Smiddy WE, Newton J, Miller D . Acute-onset endophthalmitis after cataract surgery (2000–2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol 2005; 139 (6): 983–987.
Masket S . Consultation section: cataract surgical problem: under what conditions do you perform/consider bilateral simultaneous cataract extraction with intraocular lens (IOL) implantation? What special precautions do you take/advise when considering bilateral surgery? J Cataract Refract Surg 1997; 23: 1437–1441.
Ellis MF . Responses to December 1997 consultation section (Letter). J Cataract Refract Surg 1998; 24: 430.
Zwaan J, Mullaney PB, Awad A, Al-Mesfer S, Wheeler DT . Pediatric intraocular lens implantation. Surgical results and complications in more than 300 patients. Ophthalmology 1998; 105: 112–119.
Neely DE, Plager DA, Borger SM, Golub RL . Accuracy of intraocular lens calculations in infants and children undergoing cataract surgery. J AAPOS 2005; 9: 160–165.
Kontkanen M, Kaipiainen S . Simultaneous bilateral cataract extraction: a positive view. J Cataract Refract Surg 2002; 28: 2060–2061.
Steele AL, Bradfield YS, Kushner BJ, France TD, Struck MC, Gangnon RE . Successful treatment of anisometropic amblyopia with spectacles alone. J AAPOS 2006; 10: 37–43.
Bayramlar H, Totan Y, Borazan M . Heparin in the intraocular irrigating solution in pediatric cataract surgery. J Cataract Refract Surg 2004; 30: 2163–2169.
Saint Maurice C . Paediatric anaesthesia. Curr Opin Anaesth 1994; 7: 249–250.
Fleisher LA . Risk of anesthesia. In: Miller RD (ed). Anesthesia, 5th edn. Churchill Livingstone: New York, USA, 2000, 1(22) pp 795–823.
Gelbart SS, Hoyt CS, Jastrebski G, Marg E . Long term visual results in bilateral congenital cataracts. Am J Ophthalmol 1982; 93: 615–621.
Lamberu SR, Lynn MJ, Reeves R, Plager DA, Buckley EG, Wilson ME . Is there a latent period for the surgical treatment of children with dense bilateral congenital cataracts? J AAPOS 2006; 10 (1): 30–36.
Chak M, Wade A, Rahi JS . British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Invest Ophthalmol Vis Sci 2006; 47 (10): 4262–4269.
Peterseim MW, Wilson ME . Bilateral intraocular lens implantation in the pediatric population. Ophthalmology 2000; 107: 1261–1266.
O’Keefe M, Mulvihill A, Yeoh PL . Visual outcome and complications of bilateral intraocular lens implantation in children. J Cataract Refract Surg 2000; 26: 1758–1764.
Ma JJ, Morad Y, Mau E, Brent HP, Barclay R, Levin AV . Contact lenses for the treatment of pediatric cataracts. Ophthalmology 2003; 110: 299–305.
Cheng KP . Treatment of pediatric cataracts. Ophthalmol Clin North Am 1996; 9 (2): 239–247.
Ledoux DM, Trivedi RH, Wilson ME, Payne JF . Pediatric cataract extraction with intraocular lens implantation: visual acuity outcome when measured at age four years and older. J AAPOS 2007; 11 (3): 218–224.
Bowman RJ, Kabiru J, Negretti G, Wood ML . Outcomes of bilateral cataract surgery in Tanzanian children. Ophthalmology 2007; 114 (12): 2287–2292.
Author information
Authors and Affiliations
Corresponding author
Additional information
No author has any proprietary or financial interest in any material or method mentioned
Rights and permissions
About this article
Cite this article
Totan, Y., Bayramlar, H. & Yılmaz, H. Bilateral paediatric cataract surgery in the same session. Eye 23, 1199–1205 (2009). https://doi.org/10.1038/eye.2008.173
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.173