Abstract
Objective
To evaluate bimatoprost/timolol fixed combination (BTFC) vs latanoprost/timolol fixed combination (LTFC) given each evening over the 12-h intraocular pressure (IOP) diurnal curve.
Methods
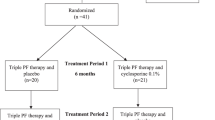
A total of 54 eyes of 54 patients (24 with primary open-angle glaucoma (POAG) and 30 with pseudoexfoliative glaucoma (PXG)) were included in this prospective, randomized, evaluator-masked single centre crossover study. Patients with an IOP of ⩾19 mmHg, under treatment with prostaglandin analogues, were randomized to BTFC or LTFC for a 12-week treatment period after a 6-week run-in period on timolol maleate 0.5% (one drop in each eye twice each day). Patients were then switched to the opposite treatment for the second period. Six 12-h IOP curves were recorded for each patient at baseline (under treatment with timolol maleate 0.5% BID), week 6 and 12 for each treatment period.
Results
The 12-h IOP (mean (SD)) values were 22.0 (1.0) mmHg at baseline, 17.7 (0.8) mmHg on BTFC, and 18.5 (0.8) mmHg on LTFC (P<0.001). At individual time points, there was a significant difference between groups at 0800, 0100, 1200, 1800, and 2000 hours with BTFC having greater ocular hypotensive effect, P<0.001. The most frequently reported adverse event in the study was conjunctival hyperaemia. Average hyperaemia scores were slightly but significantly lower in the LTFC treatment period (P=0.04).
Conclusion
This study suggests that the evening-dosed BTFC provides better IOP control than that of LTFC over 12 h. However, the IOP difference was small and may not be clinically meaningful.
Similar content being viewed by others
Introduction
Lowering intraocular pressure (IOP) reduces the risk of visual field loss in patients with glaucoma and ocular hypertension.1, 2, 3
Whenever possible, it is preferable to control IOP with a single drug rather than multiple drugs, because every drug added to the regime has side effects, and each added drug increases the costs and may reduce patient compliance.
When a single medication does not adequately reduce IOP, additional hypotensive agents are added to the therapeutic regime. In this setting, a fixed combination preparation may improve both the compliance and the quality of life.4
The fixed combination of latanoprost and timolol (LTFC; Xalacom®, Pharmacia, Kalamazoo, MI, and Pfizer, New York, NY) was the first prostaglandin analogue/beta-blocker fixed combination available in the market. Several papers have shown the IOP-lowering effect of the LTFC.5, 6, 7, 8, 9, 10, 11, 12, 13
The fixed combination bimatoprost/timolol (BTFC; Ganfort®, Allergan, Irvine, CA) is a new fixed combination antiglaucoma therapy that combines bimatoprost 0.03% and timolol 0.5%.
BTFC has been shown to be as effective as the association of its individual components.14
We recently published the results of an evaluator-masked, randomized parallel study comparing BTFC administered once daily in the evening vs once-daily evening LTFC in patients with open-angle glaucoma (OAG).15
Our study found that BTFC demonstrated a superior IOP-lowering effect than LTFC in OAG patients over a period of 4 weeks.
The purpose of this study was to evaluate the 12-h pressure curve of BTFC vs LTFC, both administered in the evening in patients with OAG.
To the best of our knowledge (after a Medline search, update December 2007), this is the first crossover study to compare 12-h diurnal IOP reduction with these two fixed combinations.
Material and methods
Study design
This was a prospective, single centre, evaluator-masked crossover study.
The study was evaluator masked because differences in patient adverse events were likely to reveal treatment assignments. Unmasked personnel were responsible for study medication distribution and collection, whereas masked personnel performed all study-related examinations.
Patients and unmasked personnel were recommended not to reveal the study assignment to the masked evaluator.
Patients
Enrolled patients were men or women of at least 40 years with a clinical diagnosis of OAG, with or without exfoliation syndrome.
The study was conducted on consecutive patients, referred or recruited, attending the outpatient service of the Glaucoma Unit, Instituto Galego de Oftalmoloxia, Santiago de Compostela, Spain, from November 2006 to March 2007 who met the inclusion and exclusion criteria.
All patients signed a written informed consent form in accordance with the tenets of the Declaration of Helsinki and with local ethical approval.
We included patients of either gender, older than 40 years, who had an IOP of ⩾19 mmHg, under treatment with prostaglandin analogues, at 0900 and 1100 hours. For entry into the study, the IOP-lowering effect of prostaglandin analogues must be higher than 20%.
Glaucoma was defined on the basis of at least two reliable achromatic automated perimetry using the 24-2 Swedish Interactive Threshold Algorithm (SITA) (Humphrey visual field analyzer, Carl Zeiss Meditec Inc., Dublin, CA) with a Glaucoma Hemifield Test outside of normal limits in the presence of a typical glaucomatous disc and an open chamber angle.
To provide baseline comparison data, all patients were placed on timolol maleate 0.5% (one drop in each eye twice each day) for a period of 6 weeks.
To be eligible for randomization, a mean diurnal IOP ⩾19 mmHg, under treatment with timolol 0.5% BID, was required at baseline.
Study visits occurred at baseline and after 6 and 12 weeks of therapy. The masked investigator performed three IOP measurements in each eye, alternating between eyes, and starting with the right eye at 0800, 1000, 1200, 1400, 1600, 1800, and 2000 hours. The mean of these three measurements at each time point was used in the statistical analyses.
Table 1 summarizes the main inclusion and exclusion criteria.
Methods
The methods of this study were similar to those described previously by our group.17 At the screening visit (visit 0), each patient underwent a standard ophthalmic examination, including a review of the medical history, best-corrected visual acuity (EDTRS scale), slit-lamp examination of the anterior segment with dilated pupils, IOP measurement at 0900 and 1100 hours using Goldmann applanation tonometry, gonioscopy, dilated funduscopic examination using a 78 dioptre lens, stereoscopic optic disc photography, central corneal thickness (CCT), and an automated perimetry using the 24-2, full threshold strategy on the Humphrey visual field analyzer (Carl Zeiss Meditec, Dublin, CA, USA). CCT was measured using an ultrasonic pachymeter (Corneo-gage plus 2, Sonogage, Cleveland, OH).
Patients potentially eligible started a 6-week run-in period under timolol maleate 0.5% (one drop in each eye twice each day). After completion of the timolol run-in period, patients reported to the clinic for baseline measurements (visit 1).
Baseline visit included medical and ophthalmic history and a complete ophthalmic examination including best-corrected visual acuity (EDTRS scale), slit-lamp examination of the anterior segment, and diurnal 12-h IOP measurement using Goldmann applanation tonometry and conjunctival hyperaemia by means of a digital camera MVC CD 400 (Sony Corporation, Tokyo, Japan).
To record the diurnal tonometric curves, the patients arrived in the morning (at 0745 hours) and stayed for the following 12 h. The same investigator (AM) measured the IOP using the same calibrated instrument (Goldmann applanation tonometer) to perform 12-h diurnal curves of IOP. The IOP measurements were recorded at 0800, 0100, 1200, 1400, 1600, 1800, and 2000 hours.
Patients who met the IOP inclusion requirements were randomly assigned, using a computer-generated randomization sequence, to receive either the bimatoprost/timolol fixed combination (BTFC) once every evening at 2200 hours or the latanoprost/timolol fixed combination (LTFC) at 2200 hours for the first 12-week treatment period.
At week 6 (visit 2), a 12-h diurnal curve was performed.
At the end of period 1, week 12, a 12-h diurnal curve was again made (visit 3). An adverse event check was performed and a pupil dilatation with slit-lamp examination of the fundus was carried out.
After the end of period 1, subjects were placed on timolol alone, and after 6 weeks they were studied for a second baseline measurement (visit 4).
Patients were then switched to the second study medicine for period 2, and a 12-h diurnal curve was performed at week 6 (visit 5) and at the end of the second 12-week treatment period (visit 6).
Conjunctival hyperaemia was assessed at baseline, visits 2–6, before starting with the IOP measurements, by means of a digital camera MVC CD 400 (Sony Corporation, Tokyo, Japan).
Conjunctival hyperaemia was rated on a 5-point scale of severity (0, none; 0.5, trace; 1.0, mild; 2, moderate; and 3, severe).
Patients were asked about adverse events and compliance, and their responses were recorded at each follow-up study visit.
Study outcomes
The primary outcomes were to compare the mean IOP reduction from baseline to week 12 and the difference in mean IOP reduction over the 12-h period, at week 12, for BTFC and LTFC.
The secondary outcome was to compare the mean IOPs of the 12-h IOP curve for BTFC and LTFC.
Statistical analysis
This study had 90% power to detect a 1.6 mmHg difference between individual time points and between mean diurnal pressures, assuming a standard deviation of 2.5 mmHg between treatments.
The numerical data sets were tested for normal distribution with the Kolmogorov–Smirnov test. For the purpose of statistical analysis, only a randomly chosen eye was included for patients with bilateral affliction by intention-to treat analyses.
The diurnal IOP (the average of the 7 time points evaluated) and the difference in IOP reduction between treatment groups were performed using a repeated measures analysis of variance (ANOVA).
IOP at individual time point, was evaluated by intragroup comparisons made between the values obtained under baseline and treatment conditions. For this purpose, a two–tailed, paired Student's t-test was used.
A Bonferroni correction was used to correct the P-value from individual time points over the 12-h diurnal IOP curve (α/7). Statistical significance was achieved with P<0.0073.
The Fisher exact test was used to evaluate differences in the proportion of patients who achieved a mean diurnal IOP lower than 18 mmHg.
Adverse events were evaluated by a McNemar test. The power of the McNemar test was 58.9% to detect the difference in proportions of adverse events of 15% if there was a proportion of an event of the 15%.
Statistical analyses were performed using MedCalc 7.3.0.1.18
Results
Patients
Of the 61 consecutive patients screened, 54 were included in the trial. Their main characteristics are shown in Table 2. All patients completed the study, and no major adverse events were recorded.
Thirty (55.6%) patients had pseudoexfoliative glaucoma (PXG). Although this was not originally planned in the protocol, there were sufficient patients to enable a post hoc subgroup analysis of efficacy in this population.
IOP
No significant differences were observed in the mean baseline IOP at any diurnal time point (Table 3).
Figure 1 shows the mean diurnal 12-h IOP at baseline (timolol treatment) and after BTFC and LTFC treatment. Both treatments significantly reduced IOP from baseline at each individual time point and for the 12-h curve (P<0.001) (Table 3).
Mean intraocular pressure (IOP) at baseline, week 6, and 12 in the overall of study population. Each point represents the mean (95% confidence interval). Bimatoprost/timolol fixed combination: solid line with solid squares. Latanoprost/timolol fixed combination: dotted line with solid triangles. The differences between study drugs are statistically significant, P<0.0001.
The mean (standard deviation) values were 22.0 (1.0) mmHg at baseline, 17.7 (0.8) mmHg on BTFC, and 18.5 (0.8) mmHg on LTFC (P<0.001).
At individual time points, there was a significant difference between groups at 0800, 1000, 1200, 1800, and 2000 hours with BTFC having greater ocular hypotensive effect, P<0.001 (Table 3).
The mean IOP fluctuation of 12-h IOP (highest minus lowest IOP reading within the 12-h pressure curve) was statistically lower with BTFC (4.8 vs 5.9, P<0.001).
In addition, IOP reduction from baseline was significantly greater with BTFC, compared with LTFC, at each time point for the 12-h curve (Table 4).
The mean diurnal IOP was < 18 mmHg in 64.8% (35/54) of patients at the end of the BTFC treatment period as compared with 29.6% (16/54) of patients at the end of the LTFC period, P<0.001.
BTFC showed a similar IOP-lowering effect in both POAG and PXG patients.
BTFC provided significantly greater IOP lowering than LTFC for the diurnal mean IOP, at each time point, in both PXG and POAG patients.
Adverse events
No serious adverse events were detected in this study. The incidence and types of adverse events were similar in both treatments (Table 5). The most frequently reported adverse event in the study was conjunctival hyperaemia, which occurred in 40.7% (22/54) of patients in the BTFC treatment period and in 35.2% (19/54) of patients in the LTFC treatment phase (P=0.66).
The mean conjunctival hyperaemia score was slightly but significantly greater with BTFC, compared with LTFC (1.5 vs 1.2, P=0.04).
The most commonly reported systemic adverse event in the study was back pain, which occurred in 29.6% (16/54) of patients in the BTFC treatment period and in 33.3% (18/54) of patients in the LTFC treatment phase (P=0.84).
There was no significant difference between the two treatments in the incidence of the other adverse events reported in the study.
Discussion
The results of this 12-week crossover study demonstrate a significantly greater IOP-lowering effect of the fixed combination of bimatoprost and timolol instilled once a day in the evening, compared with that of latanoprost and timolol administered once a day in the evening.
Although both BTFC and LTFC considerably lower IOP in patients previously treated with timolol maleate 0.5% BID, with POAG and PXG, BTFC provided greater mean IOP reductions from baseline than LTFC at every time point at every study visit, reaching statistical significance at all time points measured.
Of interest in this study was the incremental IOP-lowering effect of both treatments at week 12 as compared with that of week 6. On the basis of our results, 6 weeks could be not time enough for evaluating the IOP lowering effect of these therapies.
To the best of our knowledge, this study is the first crossover study to assess diurnal IOP reduction with these two fixed combinations in glaucoma.
It is very difficult to compare our results with those previously reported, because in our study there was a timolol run-in period, and IOP at baseline was significantly lower than reported in those studies.
These results agree with those previously published by our group,15 which reported a statistically significant mean IOP difference (0.7 mmHg) between these two fixed combinations.
Our findings support other trials that reported superior efficacy of bimatoprost relative to latanoprost. In a study by Konstas et al19 the IOP-lowering efficacy of bimatoprost and latanoprost was evaluated. In this crossover 3-month clinical study, bimatoprost provided a significantly greater IOP reduction for all time points and for the diurnal curve after 3 months of treatment.
The mean diurnal IOP difference found by Konstas et al19 (1.0 mmHg) is slightly superior to that found in our study (0.8 mmHg). The reason for the greater difference may be related with the fact that we included patients with POAG and PXG while Konstas et al19 analysed PXG patients.
However, the mean diurnal IOP difference found in our study (0.8 mmHg) was greater than that previously reported by Konstas et al20 in POAG patients (0.6 mmHg).
Konstas et al19 suggested two explanations for the different response in PXG and POAG patients: that the higher IOP in PXG allows better differentiation between the two drugs or that bimatoprost may be more effective in PXG.
Conversely, we found that the mean diurnal IOP difference between BTFC and LTFC was similar in POAG as in PXG.
In contrast, Parrish et al21 reported no significant differences between latanoprost and bimatoprost in adjusted mean IOP reductions from baseline to week 12 at all IOP time points measured. However, the difference in unadjusted mean IOP reduction was slightly greater but not significant with bimatoprost.
Similar results were reported by Orzalesi et al22 who showed, over a 24-h period, similar mean IOP-lowering effects of the prostaglandin analogues.
Nonetheless, our results differed from the Parrish et al and Orzalesi et al trials because we found a statistical difference between treatments.21, 22
This study also evaluated the mean range of IOP. Lack of variation has been shown in several studies to be important in helping to prevent visual field progression in glaucoma patients.23, 24 Conversely, the Early Manifest Glaucoma Trial (EMGT) was unable to demonstrate any effect of increased IOP fluctuation on glaucoma progression.25
In this study, LTFC provided a mean IOP fluctuation of 5.9 mmHg, and BTFC showed a significantly lower mean range of 4.8 mmHg.
These ranges of the 12-h pressure for the fixed combinations were higher than shown in past studies.13, 20, 26 These differences may be explained by the low mean IOP found in our study at 1400 hours.
This study indicates that the mean IOP reduction from baseline, for each time point and for the mean diurnal, was significantly greater with BTFC than with LTFC after 12 weeks of therapy. In addition, the mean diurnal IOP was statistically lower by 0.8 mmHg with BTFC than with LTFC. Although the clinical relevance of such difference may be questioned, the Early Manifest Glaucoma Trial suggest that for each mmHg of higher IOP, the risk of progression in early glaucoma may increase by 10% over the period of that study.27
Concerning the ocular side effects, patients treated with BTFC seemed to have more local adverse events than those treated with LTFC (Table 5), although only one of the parameters (level of conjunctival hyperaemia) reached statistical significance.
This study confirms the findings of previous comparative studies that have evaluated conjunctival hyperaemia after the use of topical prostaglandin analogues.15, 20, 21 Hyperaemia scores in patients treated with BTFC have been found to be significantly higher than those in patients treated with LTFC after 12 weeks of therapy.
Homer et al14 reported a lower proportion of hyperaemia in BTFC, compared with the association of its components, 19.3 vs 25.6%, respectively. However, we found that in the BTFC treatment period, 22 patients (40.7%) showed a higher degree of conjunctival hyperaemia at the end of the phase than at baseline. The difference may be explained by the different methods for the assessment of hyperaemia or by a possible difference based on the dosing of the different products.
These results agree with those published previously by our group using the same method for the assessment of conjunctival hyperaemia.15
We recognize the limitations of this study. First, this is a single-centre study with a limited number of patients. Second, our study was limited by its short time frame. Twelve weeks could be sufficient to evaluate changes in IOP levels and to assess the presence or absence of many potentially adverse events. However, longer follow-up periods are required to assess differences in visual function. Third, our study did not provide information about IOP during the night, and it is well known that the risk of glaucoma progression is increased, at least in some cases, by the fact that IOP may be higher during the night.28, 29, 30
Fourth, this study included a large proportion of patients with PXG (55.6%).
In conclusion, BTFC provides a significantly greater mean diurnal IOP reduction than LTFC in eyes previously treated with timolol maleate 0.5% BID, although the clinical relevance of such difference is questionable.
Although there were no significant differences in the proportion of patients with conjunctival hyperaemia, the hyperaemia scores were significantly greater with the BTFC.
Further researches are necessary to assess differences between these two fixed combination therapies.
References
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Kass MA, Heuer DK, Higginbotham EJ, Jhonson CA, Keltner JL, Miller JP et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002; 120: 1268–1279.
European Glaucoma Society. Terminology and Guidelines for Glaucoma, 2nd edn. DOGMA, Srl: Savona, Italy, 2003.
Diestelhorst M, Almegard B . Comparison of two fixed combinations of latanoprost and timolol in open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 1998; 236 (8): 577–581.
Larsson LI . Effect on intraocular pressure during 24 h after repeated administration of the fixed combination of latanoprost 0.005% and timolol 0.5% in patients with ocular hypertension. J Glaucoma 2001; 10 (2): 109–114.
Larsson LI . The effect on diurnal intraocular pressure of the fixed combination of latanoprost 0.005% and timolol 0.5% in patients with ocular hypertension. Acta Ophthalmol Scand 2001; 79 (2): 125–128.
Higginbotham EJ, Feldman R, Stiles M, Dubiner H, Fixed Combination Investigative Group. Latanoprost and timolol combination therapy vs monotherapy: one-year randomized trial. Arch Ophthalmol 2002; 120 (7): 915–922.
Pfeiffer N, European Latanoprost Fixed Combination Study Group. A comparison of the fixed combination of latanoprost and timolol with its individual components. Graefes Arch Clin Exp Ophthalmol 2002; 240 (11): 893–899.
Diestelhorst M, Larsson LI, European Latanoprost Fixed Combination Study Group. A 12 week study comparing the fixed combination of latanoprost and timolol with the concomitant use of the individual components in patients with open angle glaucoma and ocular hypertension. Br J Ophthalmol 2004; 88 (2): 199–203.
Shin DH, Feldman RM, Sheu WP, Fixed Combination Latanoprost/Timolol Study Group. Efficacy and safety of the fixed combinations latanoprost/timolol vs dorzolamide/timolol in patients with elevated intraocular pressure. Ophthalmology 2004; 111 (2): 276–282.
Diestelhorst M, Larsson LI, European-Canadian Latanoprost Fixed Combination Study Group. A 12-week, randomized, double-masked, multicenter study of the fixed combination of latanoprost and timolol in the evening vs the individual components. Ophthalmology 2006; 113: 70–76.
Konstas AGP, Lake S, Economou AI, Kaltsos K, Jenkins JN, Stewart WC . 24-h control with a latanoprost-timolol fixed combiantion vs timolol alone. Arch Ophthalmol 2006; 124: 1553–1557.
Hommer A, Ganfort Investigators Group I. A double-masked, randomized, parallel comparison of a fixed combination of bimatoprost 0.03%/timolol 0.5% with non-fixed combination use in patients with glaucoma or ocular hypertension. Eur J Ophthalmol 2007; 17: 53–62.
Martinez A, Sanchez M . A comparison of the safety and intraocular pressure lowering of bimatoprost/timolol fixed combination vs latanoprost/timolol fixed combination in patients with open-angle glaucoma. Curr Med Res Opin 2007; 23 (5): 1025–1032.
Hodapp E, Parrish R, Anderson D . Clinical Decisions in Glaucoma. Mosby-Year Book, inc: St Louis, 1993.
Martinez A, Sanchez M . Intraocular pressure lowering effect of dorzolamide/timolol fixed combination in patients with glaucoma who were unresponsive to prostaglandin analogs/prostamides. Curr Med Res Opin 2007; 23 (3): 595–599.
MedCalc (computer program). Version 7.3.0.1 Belgium: MedCalc software, 2004.
Konstas AGP, Holló G, Irkec M, Tsironi S, Durukan I, Goldenfield et al. Diurnal IOP control with bimatoprost vs latanoprost in exfoliative glaucoma: a crossover, observer-masked, three-centre study. Br J Ophthalmol 2007; 91: 757–760.
Konstas AGP, Katsimbris JM, Lallos N, Boukaras GP, Jenkins JN, Stewart WC . Latanoprost 0.005% vs bimatoprost 0.03% in primary open-angle glaucoma patients. Ophthalmology 2005; 112: 262–266.
Parrish RK, Palmberg P, Sheu WP, for the XLT study group. A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: a 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmolo 2003; 135: 688–703.
Orzalesi N, Rosseti L, Bottoli A, Fogagnolo P . Comparison of the effects of latanoprost, travoprost, and bimatoprost on circadian intraocular pressure in patients with glaucoma or ocular hypertension. Ophthalmology 2006; 113: 239–246.
Asrani S, Zeimer R, Wilensky J, Gleser D, Vitale S, Lindermuth K . Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma 2000; 9: 134–142.
Nouri-Mahdavi K, Hoffman D, Coleman AL, Liu G, Li G, Gaasterland D et al. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology 2004; 111: 1627–1635.
Bengtsson B, Leske MC, Hyman L, Heijl A, Early Manifest Glaucoma Trial Group. Fluctuation of intraocular pressure and glaucoma pregression in the Early Manifest Glaucoma Trial. Ophthalmology 2007; 114: 205–209.
Konstas AG, Boboridis K, Tzetzi D, Kallinderis K, Jenkins JN, Stewart WC . Twenty-four hour control with latanoprost-timolol-fixed combination therapy vs latanoprost therapy. Arch Ophthalmol 2005; 123: 898–902.
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E, Early Manifest Glaucoma Trial Group. Factors for glaucoma progression and the effect of treatment. The Early Manifest Glaucoma Trial. Arch Ophthalmol 2003; 121: 48–56.
Orzalesi N, Rossetti L, Bottoli A, Fumagalli E, Fogagnolo P . The effect of latanoprost, brimonidine, and a fixed combination of timolol and dorzolamide on circadian intraocular pressure in patients with glaucoma or ocular hypertension. Arch Ophthalmol 2003; 121: 453–457.
Liu JH, Zhang X, Kripke DF, Weinreb RN . Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes. Invest Ophthalmol Vis Sci 2003; 44: 1586–1590.
Wax MB, Camras CB, Fiscella RG, Girkin C, Singh K, Weinreb RN . Emerging perspectives in glaucoma: optimizing 24-h control of intraocular pressure. Am J Ophthalmol 2002; 133: S1–S10.
Acknowledgements
The study medications were provided by Allergan (BTFC) and by the Instituto Galego de Oftalmoloxía (LTFC). This study was supported, in part, by research Grant no. XUGA IN825B2005/4-0 from the Galician Government.
Author information
Authors and Affiliations
Corresponding author
Additional information
Antonio Martínez has received honoraria from lectures and reimbursement for attending symposia from AllerganFinancial interest: None
Rights and permissions
About this article
Cite this article
Martinez, A., Sanchez, M. Bimatoprost/timolol fixed combination vs latanoprost/timolol fixed combination in open-angle glaucoma patients. Eye 23, 810–818 (2009). https://doi.org/10.1038/eye.2008.148
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.148
Keywords
This article is cited by
-
Efficacy and tolerability of fixed-combination bimatoprost/timolol versus fixed-combination dorzolamide/brimonidine/timolol in patients with primary open-angle glaucoma or ocular hypertension: a multicenter, prospective, crossover study
BMC Ophthalmology (2014)
-
Focusing on glaucoma progression and the clinical importance of progression rate measurement: a review
Eye (2010)