Abstract
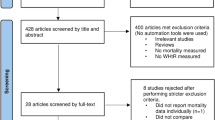
In total, 17 prospective and 35 cross-sectional studies in adults aged 18–74 years, with the aim of comparing betweenbody mass index (BMI), waist circumference (WC) and waist-to-hip ratio (WHR) in their relation to the incidence and prevalence of type II diabetes, were reviewed. Among these studies, only a few have used C-statistic, paired homogeneity test or log-likelihood ratio test for formally comparing the differences. Five prospective studies, in which formal statistic tests have been made, came out with inconsistent findings: two results were in favour of WC in Mexicans African Americanss, respectively, one result was in favour of BMI in Pima Indians, and no difference was found in the other 2 studies. Among the 11 cross-sectional studies that have formally tested the differences, most found a higher odds ratio or slightly larger area under the ROC curve (AUC) for WC than for BMI. A meta-analysis based on the individual data of the Asian cohorts using a paired homogeneity test showed, however, that there was no difference in odds ratio between BMI and WC in Chinese, Japanese, Indian, Mongolian and Filipino men. In conclusion, all studies included in this review showed that either BMI or WC (WHR) predicted or was associated with type II diabetes independently, regardless of the controversial findings on which of these obesity indicators is better.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Aekplakorn W, Kosulwat V, Suriyawongpaisal P (2006). Obesity indices and cardiovascular risk factors in Thai adults. Int J Obes (Lond) 30, 1782–1790.
al-Asfoor DH, al-Lawati JA, Mohammed AJ (1999). Body fat distribution and the risk of non-insulin-dependent diabetes mellitus in the Omani population. East Mediterr Health J 5, 14–20.
Anjana M, Sandeep S, Deepa R, Vimaleswaran KS, Farooq S, Mohan V (2004). Visceral and central abdominal fat and anthropometry in relation to diabetes in Asian Indians. Diabetes Care 27, 2948–2953.
Balkau B, Deanfield JE, Despres JP, Bassand JP, Fox KA, Smith Jr SC et al. (2007). International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168 000 primary care patients in 63 countries. Circulation 116, 1942–1951.
Berber A, Gomez-Santos R, Fanghanel G, Sanchez-Reyes L (2001). Anthropometric indexes in the prediction of type 2 diabetes mellitus, hypertension and dyslipidaemia in a Mexican population. Int J Obes Relat Metab Disord 25, 1794–1799.
Chei CL, Iso H, Yamagishi K, Tanigawa T, Cui R, Imano H et al. (2008). Body fat distribution and the risk of hypertension and diabetes among Japanese men and women. Hypertens Res 31, 851–857.
Chihaoui M, Kanoun F, Ben Rehaiem B, Ben Brahim S, Ftouhi B, Mekaouar A et al. (2001). Predictive risk factors for deterioration from normoglycemic state to type 2 diabetes mellitus or impaired glucose tolerance in a Tunisian urban population. Diabetes Metab 27, 487–495.
Chuang YC, Hsu KH, Hwang CJ, Hu PM, Lin TM, Chiou WK (2006). Waist-to-thigh ratio can also be a better indicator associated with type 2 diabetes than traditional anthropometrical measurements in Taiwan population. Ann Epidemiol 16, 321–331.
Craig P, Colaguiri S, Hussain Z, Palu T (2007). Identifying cut-points in anthropometric indexes for predicting previously undiagnosed diabetes and cardiovascular risk factors in the Tongan population. Obes Res Clin Prac 1, 17–25.
Dalton M, Cameron AJ, Zimmet PZ, Shaw JE, Jolley D, Dunstan DW et al. (2003). Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med 254, 555–563.
Diabetes Prevention Program Research Group (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346, 393–403.
Diabetes Prevention Program Research Group (2006). Relationship of body size and shape to the development of diabetes in the diabetes prevention program. Obesity (Silver Spring) 14, 2107–2117.
Diaz VA, Mainous III AG, Baker R, Carnemolla M, Majeed A (2007). How does ethnicity affect the association between obesity and diabetes? Diabet Med 24, 1199–1204.
Esmaillzadeh A, Mirmiran P, Azizi F (2004). Waist-to-hip ratio is a better screening measure for cardiovascular risk factors than other anthropometric indicators in Tehranian adult men. Int J Obes Relat Metab Disord 28, 1325–1332.
Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP et al. (2000). Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med 160, 2117–2128.
Foucan L, Hanley J, Deloumeaux J, Suissa S (2002). Body mass index (BMI) and waist circumference (WC) as screening tools for cardiovascular risk factors in Guadeloupean women. J Clin Epidemiol 55, 990–996.
Hadaegh F, Zabetian A, Harati H, Azizi F (2007). The prospective association of general and central obesity variables with incident type 2 diabetes in adults, Tehran lipid and glucose study. Diabetes Res Clin Pract 76, 449–454.
Han TS, Feskens EJ, Lean ME, Seidell JC (1998). Associations of body composition with type 2 diabetes mellitus. Diabet Med 15, 129–135.
Ho SY, Lam TH, Janus ED (2003). Waist to stature ratio is more strongly associated with cardiovascular risk factors than other simple anthropometric indices. Ann Epidemiol 13, 683–691.
Hu D, Xie J, Fu P, Zhou J, Yu D, Whelton PK et al. (2007). Central rather than overall obesity is related to diabetes in the Chinese population: the InterASIA study. Obesity (Silver Spring) 15, 2809–2816.
Huxley R, James WP, Barzi F, Patel JV, Lear SA, Suriyawongpaisal P et al. (2008). Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes Rev 9 (Suppl 1), 53–61.
Ito H, Nakasuga K, Ohshima A, Maruyama T, Kaji Y, Harada M et al. (2003). Detection of cardiovascular risk factors by indices of obesity obtained from anthropometry and dual-energy X-ray absorptiometry in Japanese individuals. Int J Obes Relat Metab Disord 27, 232–237.
Janiszewski PM, Janssen I, Ross R (2007). Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care 30, 3105–3109.
Katzmarzyk PT, Craig CL, Gauvin L (2007). Adiposity, physical fitness and incident diabetes: the physical activity longitudinal study. Diabetologia 50, 538–544.
Kaur P, Radhakrishnan E, Sankarasubbaiyan S, Rao SR, Kondalsamy-Chennakesavan S, Rao TV et al. (2008). A comparison of anthropometric indices for predicting hypertension and type 2 diabetes in a male industrial population of Chennai, South India. Ethn Dis 18, 31–36.
Ko GT, Chan JC, Cockram CS, Woo J (1999). Prediction of hypertension, diabetes, dyslipidaemia or albuminuria using simple anthropometric indexes in Hong Kong Chinese. Int J Obes Relat Metab Disord 23, 1136–1142.
Kosaka K, Noda M, Kuzuya T (2005). Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract 67, 152–162.
Krishnan S, Rosenberg L, Djousse L, Cupples LA, Palmer JR (2007). Overall and central obesity and risk of type 2 diabetes in U.S. black women. Obesity (Silver Spring) 15, 1860–1866.
Ledoux M, Lambert J, Reeder BA, Despres JP (1997). Correlation between cardiovascular disease risk factors and simple anthropometric measures. Canadian Heart Health Surveys Research Group. CMAJ 157 (Suppl 1), S46–S53.
Lee CMY, Huxley RR, Wildman RP, Woodward M (2008). Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 61, 646–653.
Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL et al. (2002). Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord 26, 1232–1238.
Lindstrom J, Tuomilehto J (2003). The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 26, 725–731.
Lorenzo C, Serrano-Rios M, Martinez-Larrad MT, Gonzalez-Villalpando C, Williams K, Gabriel R et al. (2007). Which obesity index best explains prevalence differences in type 2 diabetes mellitus? Obesity (Silver Spring) 15, 1294–1301.
Mansour AA, Al-Jazairi MI (2007). Cut-off values for anthropometric variables that confer increased risk of type 2 diabetes mellitus and hypertension in Iraq. Arch Med Res 38, 253–258.
Meisinger C, Doring A, Thorand B, Heier M, Lowel H (2006). Body fat distribution and risk of type 2 diabetes in the general population: are there differences between men and women? The MONICA/KORA Augsburg cohort study. Am J Clin Nutr 84, 483–489.
Menke A, Muntner P, Wildman RP, Reynolds K, He J (2007). Measures of adiposity and cardiovascular disease risk factors. Obesity (Silver Spring) 15, 785–795.
Mirmiran P, Esmaillzadeh A, Azizi F (2004). Detection of cardiovascular risk factors by anthropometric measures in Tehranian adults: receiver operating characteristic (ROC) curve analysis. Eur J Clin Nutr 58, 1110–1118.
Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY, Pitkaniemi J et al. (2008). BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity (Silver Spring) 16, 1622–1635.
Nyamdorj R, Qiao Q, Soderberg S, Pitkaniemi J, Zimmet P, Shaw J et al. (2009). BMI compared with central obesity indicators as a predictor of diabetes incidence in Mauritius. Obesity (Silver Spring) 17, 342–348.
Pan X, Li G, Hu Y, Wang J, Yang W, An Z et al. (1997). Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 20, 537–544.
Pua YH, Ong PH (2005). Anthropometric indices as screening tools for cardiovascular risk factors in Singaporean women. Asia Pac J Clin Nutr 14, 74–79.
Ramachandran A, Snehalatha C, Baskar AD, Mary S, Kumar CK, Selvam S et al. (2004). Temporal changes in prevalence of diabetes and impaired glucose tolerance associated with lifestyle transition occurring in the rural population in India. Diabetologia 47, 860–865.
Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V (2006). The Indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 49, 289–297.
Rolka DB, Narayan KM, Thompson TJ, Goldman D, Lindenmayer J, Alich K et al. (2001). Performance of recommended screening tests for undiagnosed diabetes and dysglycemia. Diabetes Care 24, 1899–1903.
Sanchez-Castillo CP, Velazquez-Monroy O, Berber A, Lara-Esqueda A, Tapia-Conyer R, James WP (2003). Anthropometric cutoff points for predicting chronic diseases in the Mexican National Health Survey 2000. Obes Res 11, 442–451.
Sargeant LA, Bennett FI, Forrester TE, Cooper RS, Wilks RJ (2002). Predicting incident diabetes in Jamaica: the role of anthropometry. Obes Res 10, 792–798.
Schneider HJ, Glaesmer H, Klotsche J, Bohler S, Lehnert H, Zeiher AM et al. (2007). Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. J Clin Endocrinol Metab 92, 589–594.
Schulze MB, Heidemann C, Schienkiewitz A, Bergmann MM, Hoffmann K, Boeing H (2006). Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care 29, 1921–1923.
Schulze MB, Hoffmann K, Boeing H, Linseisen J, Rohrmann S, Mohlig M et al. (2007). An accurate risk score based on anthropometric, dietary, and lifestyle factors to predict the development of type 2 diabetes. Diabetes Care 30, 510–515.
Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Kostense PJ et al. (2003). Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn study. Am J Clin Nutr 77, 1192–1197.
Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ et al. (2001). Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obes Res 9, 696–705.
Stevens J, Couper D, Pankow J, Folsom AR, Duncan BB, Nieto FJ et al. (2001). Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obesity 9, 696–705.
Stolk RP, Suriyawongpaisal P, Aekplakorn W, Woodward M, Neal B (2005). Fat distribution is strongly associated with plasma glucose levels and diabetes in Thai adults-the InterASIA study. Diabetologia 48, 657–660.
Thomas GN, Ho SY, Lam KS, Janus ED, Hedley AJ, Lam TH (2004). Impact of obesity and body fat distribution on cardiovascular risk factors in Hong Kong Chinese. Obes Res 12, 1805–1813.
Tulloch-Reid MK, Williams DE, Looker HC, Hanson RL, Knowler WC (2003). Do measures of body fat distribution provide information on the risk of type 2 diabetes in addition to measures of general obesity? Comparison of anthropometric predictors of type 2 diabetes in Pima Indians. Diabetes Care 26, 2556–2561.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344, 1343–1350.
Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB (2005). Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr 81, 555–563.
Wang Z, Hoy WE (2004). Body size measurements as predictors of type 2 diabetes in Aboriginal people. Int J Obes Relat Metab Disord 28, 1580–1584.
Wang Z, Rowley K, Wang Z, Piers L, O′Dea K (2007). Anthropometric indices and their relationship with diabetes, hypertension and dyslipidemia in Australian Aboriginal people and Torres Strait Islanders. Eur J Cardiovasc Prev Rehabil 14, 172–178.
Wei M, Gaskill SP, Haffner SM, Stern MP (1997). Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans--a 7-year prospective study. Obes Res 5, 16–23.
Wildman RP, Gu D, Reynolds K, Duan X, Wu X, He J (2005). Are waist circumference and body mass index independently associated with cardiovascular disease risk in Chinese adults? Am J Clin Nutr 82, 1195–1202.
Woo J, Ho SC, Yu AL, Sham A (2002). Is waist circumference a useful measure in predicting health outcomes in the elderly? Int J Obes Relat Metab Disord 26, 1349–1355.
World Health Organization (2008). 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Non-Communicable Disease. WHO: Geneva.
Zimmet P, Alberti KG, Shaw J (2001). Global and societal implications of the diabetes epidemic. Nature 414, 782–787.
Acknowledgements
The earlier version of this paper was prepared as a background paper for the WHO Expert Consultation on waist circumference and waist–hip ratio (Geneva, 8–11 December 2008). We owe our sincere thanks to all experts who gave comments to improve the paper. This work has been financially supported by the Academy Finland (118492).
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on European Journal of Clinical Nutrition website (http://www.nature.com/ejcn)
Supplementary information
Rights and permissions
About this article
Cite this article
Qiao, Q., Nyamdorj, R. Is the association of type II diabetes with waist circumference or waist-to-hip ratio stronger than that with body mass index?. Eur J Clin Nutr 64, 30–34 (2010). https://doi.org/10.1038/ejcn.2009.93
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2009.93
Keywords
This article is cited by
-
Association of serum level of chemerin with visceral fat obesity in type 2 diabetic patient
International Journal of Diabetes in Developing Countries (2023)
-
Älter werden vor dem Hintergrund einer traumatischen Kindheit
Die Psychotherapie (2023)
-
Relevance of body composition in phenotyping the obesities
Reviews in Endocrine and Metabolic Disorders (2023)
-
A 16-year prospective cohort study to evaluate effects of long-term fluctuations in obesity indices of prediabetics on the incidence of future diabetes
Scientific Reports (2021)
-
The effect of metformin on body mass index and metabolic parameters in non-diabetic HIV-positive patients: a meta-analysis
Journal of Diabetes & Metabolic Disorders (2021)