Abstract
Background
The association of central obesity with higher rates of mortality is not well studied. This study evaluates the association between waist-to-height ratio (WHtR), as a measure of central obesity, with mortality.
Methods
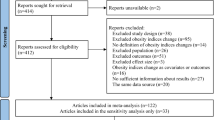
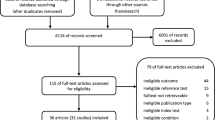
Documents were retrieved from PubMed, Web of Science, Scopus, and Google Scholar databases until May 2022. Data were extracted from cohort studies reporting effect size (hazard ratio (HR)) regarding the association between WHtR as a continuous (per 1 SD increment) or categorical (highest/lowest) measure and all-cause and cause-specific mortality. Screening of included studies was performed independently by two authors. Moreover, the quality assessment of included studies was performed based on the Newcastle-Ottawa assessment scale. Finally, random effect meta-analysis was performed to pool the data, and the outcomes’ certainty level was assess based on the GRADE criteria.
Results
Of the 815 initial studies, 20 were included in the meta-analysis. Random effect meta-analysis showed that in the general population, the all-cause mortality HRs for categorical and continuous measurements of WHtR increased significantly by 23% (HR:1.23; 95% CI: 1.04–1.41) and 16% (HR:1.16; 95% CI: 1.07–1.25), respectively. Moreover, the hazard of cardiovascular (CVD) mortality increased significantly for categorical and continuous measurements of WHtR by 39% (HR:1.39; 95% CI: 1.18–1.59) and 19% (HR:1.19; 95% CI: 1.07–1.31). The quality assessment score of all included studies was high.
Conclusions
Higher levels of WHtR, indicating central obesity, were associated with an increased hazard of CVD and all-cause mortality. This measure can be used in the clinical setting as a simple tool for predicting mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article [and its Supplementary Information files].
References
Malafaia AB, Nassif PAN, Lucas RWDC, Garcia RF, Ribeiro JGA, Proença LB. et al. Is the waist/height ratio a better parameter than bmi in determining the cardiometabolic risk profile of obese people?. Arq Bras Cir Dig. 2021;34:1–8.
Jayedi A, Soltani S, Motlagh SZT, Emadi A, Shahinfar H, Moosavi H, et al. Anthropometric and adiposity indicators and risk of type 2 diabetes: systematic review and dose-response meta-analysis of cohort studies. BMJ. 2022;376:e067516.
Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol [Internet]. 2020;49:810–23. https://doi.org/10.1093/ije/dyz273.
Chartrand DJ, Murphy-Després A, Alméras N, Lemieux I, Larose E, Després J-P. Overweight, obesity, and CVD risk: a focus on visceral/ectopic fat. Curr Atheroscler Rep [Internet]. 2022;24:185–95. https://doi.org/10.1007/s11883-022-00996-x.
Lopez-Jimenez F, Almahmeed W, Bays H, Cuevas A, Di Angelantonio E, le Roux CW, et al. Obesity and cardiovascular disease: mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur J Prev Cardiol [Internet]. 2022;29:2218–37. https://doi.org/10.1093/eurjpc/zwac187.
Hong S, Park JH, Han K, Lee CB, Kim DS, Yu SH. Association between obesity and cardiovascular disease in elderly patients with diabetes: a retrospective cohort study. J Clin Endocrinol Metab [Internet]. 2022;107:e515–27. https://doi.org/10.1210/clinem/dgab714.
Bakhtiyari M, Kazemian E, Kabir K, Hadaegh F, Aghajanian S, Mardi P, et al. Contribution of obesity and cardiometabolic risk factors in developing cardiovascular disease: a population-based cohort study. Sci Rep [Internet]. 2022;12:1544. https://doi.org/10.1038/s41598-022-05536-w.
Kang NL. Association between obesity and blood pressure in common korean people. Vasc Health Risk Manag. 2021;17:371–7.
Fan H, Li X, Zheng L, Chen X, Lan Q, Wu H, et al. Abdominal obesity is strongly associated with cardiovascular disease and its risk factors in elderly and very elderly community-dwelling Chinese. Sci Rep. 2016;6:21521.
Liu J, Tse LA, Liu Z, Rangarajan S, Hu B, Yin L, et al. Predictive values of anthropometric measurements for cardiometabolic risk factors and cardiovascular diseases among 44,048 Chinese. J Am Heart Assoc. 2019;8:e010870.
Shirasawa T, Ochiai H, Yoshimoto T, Nagahama S, Kobayashi M, Ohtsu I, et al. Associations between normal weight central obesity and cardiovascular disease risk factors in Japanese middle-aged adults: a cross-sectional study. J Heal Popul Nutr. 2019;38:1–7.
Song P, Li X, Bu Y, Ding S, Zhai D, Wang E, et al. Temporal trends in normal weight central obesity and its associations with cardiometabolic risk among Chinese adults. Sci Rep [Internet]. 2019;9:1–12. https://doi.org/10.1038/s41598-019-41986-5.
Golay A, Ybarra J. Link between obesity and type 2 diabetes. Best Pract Res Clin Endocrinol Metab. 2005;19:649–63.
Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin. 2003;32:805–22.
Saxton SN, Clark BJ, Withers SB, Eringa EC, Heagerty AM. Mechanistic links between obesity, diabetes, and blood pressure: role of perivascular adipose tissue. Physiol Rev. 2019;99:1701–63.
Klein S, Gastaldelli A, Yki-Järvinen H, Scherer PE. Why does obesity cause diabetes? Cell Metab. 2022;34:11–20.
Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55:31–55.
Burton JO, Gray LJ, Webb DR, Davies MJ, Khunti K, Crasto W, et al. Association of anthropometric obesity measures with chronic kidney disease risk in a non-diabetic patient population. Nephrol Dial Transplant. 2012;27:1860–6.
Stefansson VTN, Schei J, Jenssen TG, Melsom T, Eriksen BO. Central obesity associates with renal hyperfiltration in the non-diabetic general population: a cross-sectional study. BMC Nephrol. 2016;17:10.
Chen S, Liu H, Liu X, Li Y, Li M, Liang Y, et al. Central obesity, C-reactive protein and chronic kidney disease: a community-based cross-sectional study in southern China. Kidney Blood Press Res. 2013;37:392–401.
Hosseinpour A, Daneshzad E, Dezfouli RA, Zamani S, Qorbani M. The association between antioxidants and COVID-19 outcomes: a systematic review on observational studies. Biol Trace Elem Res [Internet]. 2023;201:5098–114. https://doi.org/10.1007/s12011-023-03588-1.
Kalaitzidis RG, Siamopoulos KC. The role of obesity in kidney disease: recent findings and potential mechanisms. Int Urol Nephrol. 2011;43:771–84.
Chen N, Wang W, Huang Y, Shen P, Pei D, Yu H, et al. Community-based study on CKD subjects and the associated risk factors. Nephrol Dial Transplant. 2009;24:2117–23.
De Boer IH, Sibley SD, Kestenbaum B, Sampson JN, Young B, Cleary PA, et al. Central obesity, incident microalbuminuria, and change in creatinine clearance in the epidemiology of diabetes interventions and complications study. J Am Soc Nephrol JASN. 2007;18:235.
Rutkowski P, Klassen A, Sebekova K, Bahner U, Heidland A. Renal disease in obesity: the need for greater attention. J Ren Nutr. 2006;16:216–23.
Chang AR, Grams ME, Ballew SH, Bilo H, Correa A, Evans M, et al. Adiposity and risk of decline in glomerular filtration rate: Meta-analysis of individual participant data in a global consortium. BMJ. 2019;364:k5301.
Bagby SP. Obesity-initiated metabolic syndrome and the kidney: a recipe for chronic kidney disease? J Am Soc Nephrol. 2004;15:2775–91.
Shi S, Ni L, Tian Y, Zhang B, Xiao J, Xu W, et al. Association of obesity indices with diabetic kidney disease and diabetic retinopathy in type 2 diabetes: a real-world study. J Diabetes Res. 2023;2023:3819830.
Maric-Bilkan C. Obesity and diabetic kidney disease. Med Clin. 2013;97:59–74.
Dai D, Chang Y, Chen Y, Chen S, Yu S, Guo X, et al. Visceral adiposity index and lipid accumulation product index: two alternate body indices to identify chronic kidney disease among the rural population in Northeast China. Int J Environ Res Public Health. 2016;13:1–11.
Memarian E, Nilsson PM, Zia I, Christensson A, Engström G. The risk of chronic kidney disease in relation to anthropometric measures of obesity: a Swedish cohort study. BMC Nephrol [Internet]. 2021;22:1–10. https://doi.org/10.1186/s12882-021-02531-7.
Man REK, Gan ATL, Fenwick EK, Gupta P, Wong MYZ, Wong TY, et al. The relationship between generalized and abdominal obesity with diabetic kidney disease in type 2 diabetes: a multiethnic asian study and meta-analysis. Nutrients. 2018;10:1685.
Wosu AC, Vélez JC, Barbosa C, Andrade A, Frye M, Chen X, et al. The relationship between high risk for obstructive sleep apnea and general and central obesity: findings from a sample of Chilean college students. Int Sch Res Not. 2014;2014:871681.
Onat A, Hergenç G, Yüksel H, Can G, Ayhan E, Kaya Z, et al. Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin Nutr. 2009;28:46–51.
Lam JCM, Mak JCW, Ip MSM. Obesity, obstructive sleep apnoea and metabolic syndrome. Respirology. 2012;17:223–36.
Balat K, Pazarlı AC, Köseoğlu Hİ, Yaşayancan N, Demir O. Importance of anthropometric measurements to determine cardiometabolic diseases in obstructive sleep apnea syndrome. Turkish Thorac J. 2021;22:11–7.
Cai X, Luo D, Liu S, Li R, Lu Y, Li M, et al. Four-year changes in central fatness, risk of diabetes, and metabolic control in older adults: a cohort study with mediation analysis. Korean J Intern Med. 2022;37:230–40.
Xu T, Liu J, Liu J, Zhu G, Han S. Relation between metabolic syndrome and body compositions among Chinese adolescents and adults from a large-scale population survey. BMC Public Health. 2017;17:1–8.
Zhang J, Zhu W, Qiu L, Huang L, Fang L. Sex- and age-specific optimal anthropometric indices as screening tools for metabolic syndrome in Chinese adults. Int J Endocrinol. 2018;2018:1067603.
Widjaja NA, Prihaningtyas RA, Hanindita MH, Irawan R, Ugrasena IDG, Handajani R. Adiponectin, anthropometric measurements and insulin resistance in adolescence with obesity. Malays J Nutr. 2020;26:165–72.
Liu PJ, Ma F, Lou HP, Zhu YN. Normal-weight central obesity is associated with metabolic disorders in Chinese postmenopausal women. Asia Pac J Clin Nutr. 2017;26:692–7.
Ferreira-Hermosillo A, Ramírez-Rentería C, Mendoza-Zubieta V, Molina-Ayala MA. Utility of the waist-to-height ratio, waist circumference and body mass index in the screening of metabolic syndrome in adult patients with type 1 diabetes mellitus. Diabetol Metab Syndr. 2014;6:1–7.
Lampignano L, Zupo R, Donghia R, Guerra V, Castellana F, Murro I, et al. Cross-sectional relationship among different anthropometric parameters and cardiometabolic risk factors in a cohort of patients with overweight or obesity. PLoS One [Internet]. 2020;15:1–12. https://doi.org/10.1371/journal.pone.0241841.
Li J, Zhu L, Wei Y, Lv J, Guo Y, Bian Z, et al. Association between adiposity measures and COPD risk in Chinese adults. Eur Respir J [Internet]. 2020;55. Available from: https://doi.org/10.1183/13993003.01899-2019.
Pang Y, Kartsonaki C, Guo Y, Chen Y, Yang L, Bian Z, et al. Central adiposity in relation to risk of liver cancer in Chinese adults: a prospective study of 0.5 million people. Int J Cancer. 2019;145:1245–53.
Jackson SS, Van Dyke AL, Zhu B, Pfeiffer RM, Petrick JL, Adami HO, et al. Anthropometric risk factors for cancers of the biliary tract in the biliary tract cancers pooling project. Cancer Res. 2019;79:3973–82.
Chandramouli C, Tay WT, Bamadhaj NS, Tromp J, Teng THK, Yap JJL, et al. Association of obesity with heart failure outcomes in 11 Asian regions: a cohort study. PLoS Med. 2019;16:1–17.
Tokushige A, Ueda S, Tomiyama H, Ohishi M, Kohro T, Higashi Y, et al. Association between waist-to-height ratio and endothelial dysfunction in patients with morbidity ― a report from the FMD-J study. Circ J. 2017;81:1911–8.
Parente EB, Harjutsalo V, Forsblom C, Groop PH. The impact of central obesity on the risk of hospitalization or death due to heart failure in type 1 diabetes: a 16-year cohort study. Cardiovasc Diabetol [Internet]. 2021;20:1–9. https://doi.org/10.1186/s12933-021-01340-4.
Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. Eur J Clin Nutr. 2007;61:1373–9.
Ioannou GN, Weiss NS, Boyko EJ, Kowdley KV, Kahn SE, Carithers RL Jr, et al. Is central obesity associated with cirrhosis-related death or hospitalization? A population-based, cohort study. Clin Gastroenterol Hepatol. 2005;3:67–74.
Carmienke S, Freitag MH, Pischon T, Schlattmann P, Fankhaenel T, Goebel H, et al. General and abdominal obesity parameters and their combination in relation to mortality: a systematic review and meta-regression analysis. Eur J Clin Nutr. 2013;67:573–85.
Chang SH, Beason TS, Hunleth JM, Colditz GA. A systematic review of body fat distribution and mortality in older people. Maturitas [Internet]. 2012;72:175–91. https://doi.org/10.1016/j.maturitas.2012.04.004.
Hajian K, Abdi Dezfouli R, Darvishi A, Radmanesh R, Heshmat R. Tenecteplase in managing acute ischemic stroke: a long-term cost–utility analysis in Iran. Expert Rev Pharmacoecon Outcomes Res [Internet]. 2023;23:123–33. Available from: https://doi.org/10.1080/14737167.2023.2152008.
Ashwell M, Mayhew L, Richardson J, Rickayzen B. Waist-to-height ratio is more predictive of years of life lost than body mass index. PLoS One. 2014;9:e103483.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Sommer I, Teufer B, Szelag M, Nussbaumer-Streit B, Titscher V, Klerings I, et al. The performance of anthropometric tools to determine obesity: a systematic review and meta-analysis. Sci Rep [Internet]. 2020;10:1–12. https://doi.org/10.1038/s41598-020-69498-7.
Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53.
Parente EB, Mutter S, Harjutsalo V, Ahola AJ, Forsblom C, Groop PH. Waist-height ratio and waist are the best estimators of visceral fat in type 1 diabetes. Sci Rep [Internet]. 2020;10:1–10. https://doi.org/10.1038/s41598-020-75667-5.
Schneider HJ, Friedrich N, Klotsche J, Pieper L, Nauck M, John U, et al. The predictive value of different measures of obesity for incident cardiovascular events and mortality. J Clin Endocrinol Metab. 2010;95:1777–85.
Dybala MP, Brady MJ, Hara M. Disparity in adiposity among adults with normal body mass index and waist-to-height ratio. iScience [Internet]. 2019;21:612–23. https://doi.org/10.1016/j.isci.2019.10.062.
Cameron AJ, Magliano DJ, Söderberg S. A systematic review of the impact of including both waist and hip circumference in risk models for cardiovascular diseases, diabetes and mortality. Obes Rev. 2013;14:86–94.
Bohr AD, Laurson K, McQueen MB. A novel cutoff for the waist-to-height ratio predicting metabolic syndrome in young American adults. BMC Public Health [Internet]. 2016;16:1–9. https://doi.org/10.1186/s12889-016-2964-6.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ. 2020;370:m3324.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ [Internet]. 2009;339:332–6. https://doi.org/10.1136/bmj.b2535.
Beller EM, Glasziou PP, Altman DG, Hopewell S, Bastian H, Chalmers I, et al. PRISMA for abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10:e1001419.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924 LP–926.
Bevilacqua MR, Gimeno SGA. Abdominal obesity in Japanese-Brazilians: which measure is best for predicting all-cause and cardiovascular mortality? TT - Obesidade abdominal em nipo-brasileiros: que medida antropométrica tem maior capacidade de predizer a mortalidade geral e por doen. Cad Saúde Pública [Internet]. 2011;27:1986–96. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2011001000012.
Luksiene D, Tamosiunas A, Virviciute D, Bernotiene G, Peasey A. Anthropometric trends and the risk of cardiovascular disease mortality in a Lithuanian urban population aged 45–64 years. Scand J Public Health. 2015;43:882–9.
Moazzeni SS, Tamehri Zadeh SS, Asgari S, Azizi F, Hadaegh F. Anthropometric indices and the risk of incident sudden cardiac death among adults with and without diabetes: over 15 years of follow-up in the Tehran Lipid and Glucose Study. Diabetol Metab Syndr [Internet]. 2021;13:1–12. https://doi.org/10.1186/s13098-021-00701-z.
Nascimento-Souza MA, De Melo, Mambrini JV, Peixoto SV, Lima-Costa MF. Association between “a body shape index” and mortality: Bambuí cohort study of aging, brazil. Cad Saude Publica. 2021;37:1–12.
Petursson H, Sigurdsson JA, Bengtsson C, Nilsen TIL, Getz L. Body configuration as a predictor of mortality: comparison of five anthropometric measures in a 12 year follow-up of the norwegian HUNT 2 study. PLoS One. 2011;6:e26621.
Schneider HJ, Wallaschofski H, Völzke H, Markus MR, Doerr M, Felix SB, Nauck M, Friedrich N. Incremental effects of endocrine and metabolic biomarkers and abdominal obesity on cardiovascular mortality prediction. PLoS One. 2012;7:1–7.
Sluik D, Boeing H, Montonen J, Pischon T, Kaaks R, Teucher B, et al. Associations between general and abdominal adiposity and mortality in individuals with diabetes mellitus. Am J Epidemiol. 2011;174:22–34.
Song X, Tabák AG, Zethelius B, Yudkin JS, Söderberg S, Laatikainen T, et al. Obesity attenuates gender differences in cardiovascular mortality. Cardiovasc Diabetol. 2014;13:1–10.
Song X, Jousilahti P, Stehouwer CDA, Söderberg S, Onat A, Laatikainen T, et al. Cardiovascular and all-cause mortality in relation to various anthropometric measures of obesity in Europeans. Nutr Metab Cardiovasc Dis. 2015;25:295–304.
Lo K, Huang YQ, Shen G, Huang JY, Liu L, Yu YL, et al. Effects of waist to height ratio, waist circumference, body mass index on the risk of chronic diseases, all-cause, cardiovascular and cancer mortality. Postgrad Med J. 2021;97:306–11.
Yu P, Pan Y, Zheng H, Wang X, Yan H, Tong X, et al. Association of high waist-to-height ratio with functional outcomes in patients with acute ischemic stroke: a report from the ACROSS-China study. Med (United States). 2017;96:e6520.
Chen J, Li M, Hao B, Cai Y, Li H, Zhou W, et al. Waist to height ratio is associated with an increased risk of mortality in Chinese patients with heart failure with preserved ejection fraction. BMC Cardiovasc Disord [Internet]. 2021;21:1–11. https://doi.org/10.1186/s12872-021-02080-9.
David CN, de Mello RB, Bruscato NM, Moriguchi EH. Overweight and abdominal obesity association with all-cause and cardiovascular mortality in the elderly aged 80 and over: a cohort study. J Nutr Heal Aging. 2017;21:597–603.
Dhana K, Kavousi M, Ikram MA, Tiemeier HW, Hofman A, Franco OH. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health. 2015;70:90–6.
Farrell SW, Barlow CE, Willis BL, Leonard D, Pavlovic A, Defina LF, et al. Cardiorespiratory fitness, different measures of adiposity, and cardiovascular disease mortality risk in women. J Women’s Heal. 2020;29:319–26.
Gnatiuc L, Tapia-Conyer R, Wade R, Ramirez-Reyes R, Aguilar-Ramirez D, Herrington W, et al. Abdominal and gluteo-femoral markers of adiposity and risk of vascular-metabolic mortality in a prospective study of 150,000 Mexican adults. Eur J Prev Cardiol. 2022;29:730–8.
De Hollander EL, Bemelmans WJE, De Groot LCPGM. Associations between changes in anthropometric measures and mortality in old age: a role for mid-upper arm circumference? J Am Med Dir Assoc [Internet]. 2013;14:187–93. https://doi.org/10.1016/j.jamda.2012.09.023.
Howell CR, Mehta T, Ejima K, Ness KK, Cherrington A, Fontaine KR. Body composition and mortality in Mexican American adults: results from the national health and nutrition examination survey. Obesity. 2018;26:1372–80.
Huai P, Liu J, Ye X, Li W-Q. Association of central obesity with all cause and cause-specific mortality in US adults: a prospective cohort study. Front Cardiovasc Med. 2022;9:1–12.
National Institute for Health and Care Excellence (NICE). Nidentification and classification of overweight and obesity (update)o Title [Internet]. 2022. Available from: https://www.nice.org.uk/guidance/cg189.
Ammar KA, Redfield MM, Mahoney DW, Johnson M, Jacobsen SJ, Rodeheffer RJ. Central obesity: association with left ventricular dysfunction and mortality in the community. Am Heart J. 2008;156:975–81.
Coutinho T, Goel K, Corrêa De Sá D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of “normal weight central obesity.”. J Am Coll Cardiol [Internet]. 2013;61:553–60. https://doi.org/10.1016/j.jacc.2012.10.035.
Darvishi A, Mousavi M, Abdi Dezfouli R, Shirazikhah M, Alizadeh Zarei M, Hendi H, et al. Cost-benefit analysis of stroke rehabilitation in Iran. Expert Rev Pharmacoecon Outcomes Res [Internet]. 2023;23:1–11. https://doi.org/10.1080/14737167.2023.2200938.
Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F. The concept of normal weight obesity. Prog Cardiovasc Dis [Internet]. 2014;56:426–33. https://doi.org/10.1016/j.pcad.2013.10.003.
Sahakyan KR, Somers VK, Rodriguez-Escudero JP, Hodge DO, Carter RE, Sochor O, et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. 2015;163:827–35.
Zhu Q, Shen F, Ye T, Zhou Q, Deng H, Gu X. Waist-to-height ratio is an appropriate index for identifying cardiometabolic risk in Chinese individuals with normal body mass index and waist circumference. J Diabetes. 2014;6:527–34.
Yoo EG. Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk. Korean J Pediatr. 2016;59:425–31.
Sharma S, Batsis JA, Coutinho T, Somers VK, Hodge DO, Carter RE, et al. Normal-weight central obesity and mortality risk in older adults with coronary artery disease. Mayo Clin Proc [Internet]. 2016;91:343–51. https://doi.org/10.1016/j.mayocp.2015.12.007.
Ma J, Xiao L. Association of general and central obesity and atopic and nonatopic asthma in US adults. J Asthma. 2013;50:395–402.
Harvie M, Hooper L, Howell AH. Central obesity and breast cancer risk: a systematic review. Obes Rev. 2003;4:157–73.
Abdi Dezfouli R, Hosseinpour A, Qorbani M, Daneshzad E. The efficacy of topical aminophylline in local fat reduction: a systematic review [Internet]. Vol. 14, Frontiers in Endocrinology. 2023. Available from: https://www.frontiersin.org/articles/10.3389/fendo.2023.1087614.
Papoutsakis C, Chondronikola M, Antonogeorgos G, Papadakou E, Matziou V, Drakouli M, et al. Associations between central obesity and asthma in children and adolescents: a case-control study. J Asthma. 2015;52:128–34.
Nevill AM, Stewart AD, Olds T, Duncan MJ. A new waist-to-height ratio predicts abdominal adiposity in adults. Res Sport Med [Internet]. 2020;28:15–26. https://doi.org/10.1080/15438627.2018.1502183.
Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56:303–7.
Ejtahed HS, Kelishadi R, Qorbani M, Motlagh ME, Hasani-Ranjbar S, Angoorani P, et al. Utility of waist circumference-to-height ratio as a screening tool for generalized and central obesity among Iranian children and adolescents: the CASPIAN-V study. Pediatr Diabetes. 2019;20:530–7.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 05 could be a suitable global boundary value. Nutr Res Rev. 2010;23:247–69.
Funding
This study was funded by Alborz University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
RA & AH conducted the primary search and the screening stages and wrote the manuscript. SA created tables. NMK performed the analytical procedures. Finally, HE and MQ checked the data and monitored the correctness of the work process.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Alborz University of Medical Sciences.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41366_2023_1388_MOESM1_ESM.docx
Supplementary table 1 (S1). The score of Newcastle-Ottawa assessment scale for the retrieved studies. Supplementary table 2. GRADE evidence profile: The association between central obesity and mo
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdi Dezfouli, R., Mohammadian Khonsari, N., Hosseinpour, A. et al. Waist to height ratio as a simple tool for predicting mortality: a systematic review and meta-analysis. Int J Obes 47, 1286–1301 (2023). https://doi.org/10.1038/s41366-023-01388-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01388-0