Nearly 30 years ago — more than a decade after HIV/AIDS was first identified — a group of scientists in the United States and France reported impressive results from a clinical trial. Pregnant women living with HIV could reduce the risk of transmitting the virus to their newborn child by around 67% if they took a drug called zidovudine during pregnancy and their infant took it for the first six weeks of life1. Five years later, a similar finding was reported in Africa2 where, at the time, the prevalence of HIV among pregnant women exceeded 35% in several regions.
These studies, and subsequent ones that elucidated how effectively antiretroviral therapy could block parent-to-child transmission of HIV, augured an era of tremendous progress — both towards eliminating such transmission and scaling up access to life-saving treatments for children and adults living with HIV.
Since these landmark studies, 5.5 million children of mothers living with HIV have been born free of the disease. This is due in large part to a programme called the US President’s Emergency Plan for AIDS Relief (PEPFAR), created under former US president George W. Bush. Since its inception, PEPFAR, which one of us (J. N.) now leads, has ensured crucial access to life-saving treatment for more than 20 million people in at least 50 countries.
Twenty years after the programme was created, we now have the tools and knowledge to end the HIV/AIDS pandemic as a threat to public health — and to do so by 2030. According to the United Nations Programme on HIV/AIDS (UNAIDS), this would mean reaching the ‘95-95-95’ targets: at least 95% of people living with HIV should know their status; at least 95% of those people should be on life-saving antiretroviral therapy; and at least 95% of those people should have an undetectable viral load3. The crucial question is how do we support countries to achieve these goals?
Early efforts to combat HIV/AIDS focused on systems-level changes — the procurement of drugs, training of health workers and the provision of clinics — that were needed to ensure that effective interventions were made available to millions of people. The global health community should continue to ensure sustained investment in these systems-level strategies. But we also have an opportunity to use behavioural-science approaches to reach populations that are most in need. Making people, rather than systems, the core focus of our response is the solution to finally ending the pandemic.
Uphill battle
Botswana offers an important model for other countries (see ‘Building on success’). In 2008, 1 in 3 pregnant women aged 15–49 in Botswana were living with HIV4. By 2022, prevalence among women aged 15–49 had dropped to around 24%5, largely thanks to the government partnering with PEPFAR and other organizations, including civil society and faith-based groups. And in 2021, the World Health Organization (WHO) declared Botswana to be the first high-burden country, in which more than 2% of pregnant women are living with the virus, to be on track to eliminating new HIV infections among children.
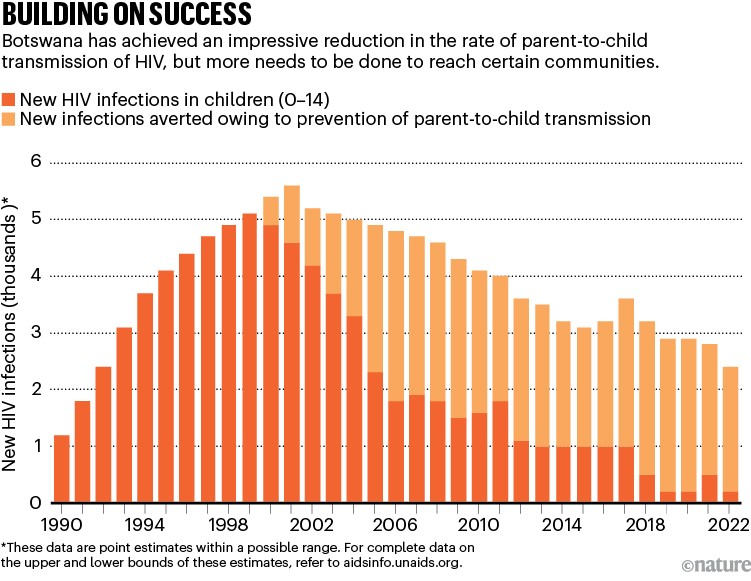
Source: UNAIDS
Botswana’s achievements stem mainly from efforts to ensure that people living with HIV — and those at greatest risk of contracting the infection — can access life-saving interventions. These include drugs that eliminate the risk of parent-to-child transmission; antiretroviral therapy, which by suppressing the virus, both protects the infected person from severe illness and death, and blocks further transmission; condoms; voluntary male circumcision; and pre-exposure prophylaxis therapy (PrEP), all of which reduce people’s chances of contracting the virus.
But as infection becomes less common globally, it is becoming more challenging to reach the individuals and communities that continue to be severely affected by HIV/AIDS.
Hope rises that a vaccine can shield people with HIV from a deadly threat
Testing is crucial — both to link people to treatment, and to raise awareness about the possible preventive measures available to them and their partners. (Globally, an estimated 5.5 million people are living with HIV but are unaware of their status.) There is also compelling evidence that beginning antiretroviral therapy quickly — ideally on the same day as getting a diagnosis — increases the likelihood of a person taking the therapy, and of continuing to take it throughout their lives6.
Numerous barriers, however, prevent people — particularly those who might not be able to access care in current health-care systems — from getting tested and from receiving timely antiretroviral therapy7. These include anticipated or encountered stigma and discrimination, both in clinics and in the broader community; the logistical challenges of getting access to care or collecting medication; and the possibility of inciting anger and mistrust in partners or family members. Similarly, those who are most likely to benefit from various prevention strategies often feel the least empowered to access them.
No community left behind
For any one community, one strategy might work better or be more feasible at scale than another. But helping countries to achieve the 95-95-95 targets will require empowering health ministries, clinicians, community health workers and HIV activists to participate in the design of programmes that ensure everyone has access to life-long HIV care that is centred around the needs of individuals.
Most new infections occur in adolescents and young adults. So efforts should prioritize young people — specifically, girls and women aged 15–24 and men aged 25–35. Young people, aged 15–24, account for around 27% of new HIV infections globally. Yet in eastern and southern Africa — the region of the world most severely affected by HIV — only 25% of girls and 17% of boys between the ages of 15 and 19 underwent HIV testing in the past year.
Efforts should also continue to prioritize those who would benefit most from preventive treatments such as PrEP, including girls and women, sex workers and members of the LGBT+ community (people from sexual and gender minorities). These people might not be aware that they are at high risk of contracting HIV, or realize the degree to which PrEP could protect them8.

A youth-run HIV/AIDS centre provides counselling and testing in Bongor, Chad.Credit: Micah Albert/Redux/eyevine
Several studies over the past decade have indicated that young people, and others at greater risk of fearing and experiencing stigmatization and discrimination, benefit from having choices. They need to be able to select the combination of prevention or treatment interventions, the medication pick-up location and the frequency with which they take the drugs that work best for them9. But establishing youth-friendly health services can also help with this. This might entail training and supporting staff to better understand the decision-making processes, sensitivities and perspectives of young people — or providing services that are easy for young people to access while juggling school, employment, family responsibilities and so on10.
In a study published earlier this year, for example, researchers offered girls and women aged 18–25 information to help them with decision-making in a primary health clinic in Johannesburg, South Africa. The information package included youth-friendly information and images of various prevention interventions. The uptake of PrEP among this group was more than 90%, and after one month, twice as many people were continuing to take it, compared with the group who received standard counselling11.
Third patient free of HIV after receiving virus-resistant cells
Evidence-based strategies to reduce stigma are also crucial — especially for those experiencing discrimination on multiple fronts, for instance because of their age, gender, sexuality, HIV status or ethnicity. At the community and individual level, these strategies can involve using social networks to spread messages about interventions or recruiting people who have experienced their own challenges while living with HIV to talk to and motivate others. Independent monitoring of the quality of care received by those living with HIV is also key to improving services and lessening stigma and discrimination12.
As new prevention tools, such as the drug cabotegravir — which protects people from HIV infection for up to two months after being injected into the body — become more widely available, health-care schemes must be designed so that those who are most likely to benefit from an intervention can access it.
Changing behaviour
Whether in relation to testing, antiretroviral therapy or PrEP and other prevention interventions, incorporating behavioural and social science into the design of health-care programmes — and making this incorporation mainstream — will be essential.
A good example of the importance of behavioural interventions comes from South Africa, where men are significantly less likely than women to seek HIV testing or engage in care, and health and social-welfare systems have failed to achieve the UNAIDS 95-95-95 goals for men13. In 2020, researchers provided 500 men in Cape Town with a card containing information about how antiretroviral therapy can prevent an infected person from passing HIV to their partner or family and inviting them to get HIV testing at a mobile clinic. The messaging strategy almost doubled the number of men who came to the mobile clinic for free HIV testing14.
A meta-analysis by another group, which included data from 47 studies conducted around the world13, showed that leveraging social networks to improve case finding (the discovery of new cases and the determination of who is at risk) is a useful and cost-effective way to reach adolescents and youth. Leveraging social networks involves identifying certain people as being important in a social network, and then encouraging them to motivate sexual partners or those in their social networks, who might benefit from testing, to test for HIV. Partly because of the results of the meta-analysis, the WHO now recommends that countries increase their use of testing approaches that utilize social networks.
Several mutually reinforcing interventions that support people to change their behaviour can help to reduce the time between diagnosis and a person starting antiretroviral treatment. These approaches include providing people who have tested positive for HIV with text messages and other reminders to make appointments at their local clinic; ensuring that people can get to the clinic by public transport; and providing incentives, such as monetary rewards, for starting treatment15.
Future focus
Investing in innovative strategies that meet the needs of individuals won’t just be key to ending the HIV/AIDS pandemic by 2030. It will also help to ensure that global health systems are resilient and dynamic in the face of future public-health threats. And it will help to shift the focus of global health, so that solutions to problems for tackling disease increasingly come from the individuals and communities that are most affected, and less from high-income countries.


 Hope rises that a vaccine can shield people with HIV from a deadly threat
Hope rises that a vaccine can shield people with HIV from a deadly threat
 Third patient free of HIV after receiving virus-resistant cells
Third patient free of HIV after receiving virus-resistant cells







