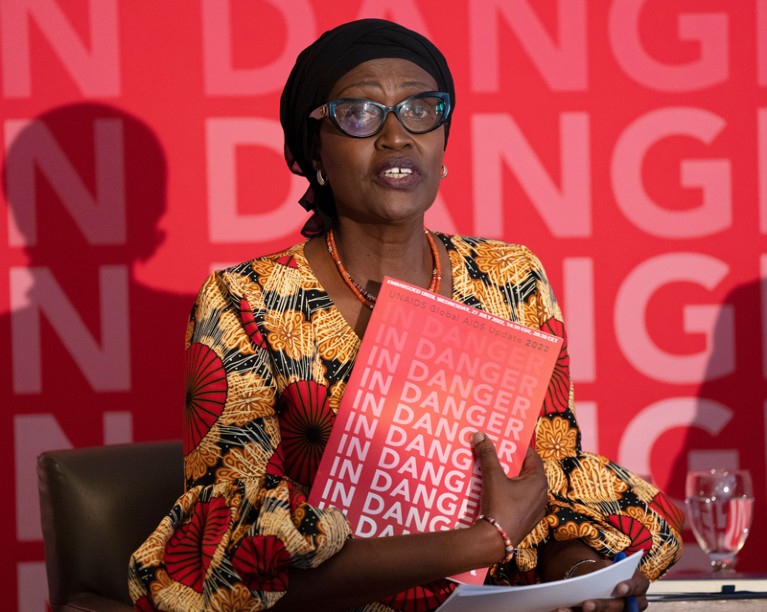
Winnie Byanyima, the head of the United Nations AIDS programme, is calling on ViiV Healthcare to price cabotegravir as close as possible to $10 per dose.Credit: Canadian Press/Shutterstock
Every year, around 1.5 million people are infected with HIV. This number is falling, although not fast enough to reach a United Nations target of fewer than 370,000 new infections a year by 2025. Last month’s decision by the World Health Organization (WHO) to recommend a new drug that protects people against HIV infection is a promising development.
The results of a randomized clinical trial showed that the drug cabotegravir (Apretude), taken as an injection six times a year, is more effective at preventing infection than is the standard means of pre-exposure prophylaxis — a daily oral dose of tenofovir disoproxil fumarate and emtricitabine — that is in use around the world (S. Delany-Moretlwe et al. Lancet 399, 1779–1789; 2022).
The WHO’s recommendation, that cabotegravir is a “safe and highly effective HIV prevention tool”, opens the way to including it in HIV-prevention programmes. Cabotegravir’s manufacturer, ViiV Healthcare in London, has pledged to charge a not-for-profit price for public programmes in the lowest-income countries. Chief executive Deborah Waterhouse calls it a “game-changing moment in HIV prevention”.
Long-lasting HIV prevention drug could be game changer — but who will pay?
Whether this turns out to be the case depends on whether the drug can be rolled out to those most in need, in particular girls and women aged 15 to 24 in the lowest-income countries. Last year, some 250,000 women and girls in this age group were infected with HIV, more than 80% of them in sub-Saharan Africa. Success will require cabotegravir to be offered at the lowest price possible. For this to happen, transparency over how the price is calculated is essential.
Drug companies don’t usually disclose such calculations, partly because of the need for commercial confidentiality. Governments expect to be provided with data for audit and benchmarking purposes, but they don’t publish what they know, either — as Members of the European Parliament (MEPs) discovered during the COVID-19 pandemic. Although European Union member countries have spent tens of billions on COVID-19 vaccines and therapies, the suppliers and contracting governments have not explained the basis for their pricing when asked to do so by MEPs.
In the United States, the commercial price for cabotegravir has been set at $3,700 per dose (equivalent to an annual price of $22,200 per person). The not-for-profit price is yet to be made public, but it could be substantially less.
David Ripin, chief scientific officer at the Clinton Health Access Initiative, a philanthropic organization based in Boston, Massachusetts, has calculated that generics companies could make cabotegravir for $23 per person, per year; this could fall to $16 if scale-up is achieved. These figures are based on adding up the cost of the active ingredient, the cost of making it into an injectable substance and the cost of sterilizing the resulting product. A summary of Ripin’s calculations has been published online (see go.nature.com/3bdoa8x).
Unseating big pharma: the radical plan for vaccine equity
A 74-strong coalition of campaigners, public officials and researchers that includes Winnie Byanyima, the head of the Joint United Nations Programme on HIV/AIDS (UNAIDS), is urging Waterhouse to price cabotegravir as close as possible to $60 per person per year. This is equivalent to the amount governments and philanthropic funders are currently paying for oral pre-exposure prophylactic drugs.
ViiV Healthcare has told Nature it cannot match this price, but that it is committed to allowing cabotegravir to be copied by generics manufacturers so that the drug can be made and distributed quickly, and that it will charge a not-for-profit price. These are welcome steps. But the company could go one better: let the world know what the price will be and provide a breakdown of how it was calculated.
In the meantime, more researchers could make their own estimates, which would help to provide governments and other funders with a benchmark figure for their discussions on what to pay. The outlook for extra domestic and international funding for HIV/AIDS isn’t good, according to the latest update from UNAIDS, published last month (see go.nature.com/3zkhaix). If cabotegravir cannot be offered at a price comparable to or, ideally, lower than existing oral treatments, nations could face some difficult decisions. Members of the public deserve to know what their governments are paying — and why.

 Long-lasting HIV prevention drug could be game changer — but who will pay?
Long-lasting HIV prevention drug could be game changer — but who will pay?
 Unseating big pharma: the radical plan for vaccine equity
Unseating big pharma: the radical plan for vaccine equity
 Small payments to low-income people lead to big drops in HIV deaths
Small payments to low-income people lead to big drops in HIV deaths
 New polio vaccine poised to get emergency WHO approval
New polio vaccine poised to get emergency WHO approval
 How COVID spurred Africa to plot a vaccines revolution
How COVID spurred Africa to plot a vaccines revolution






