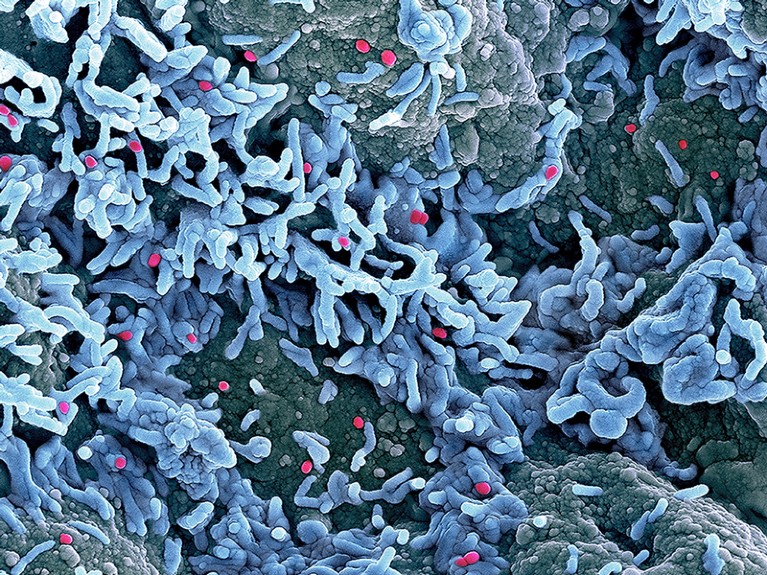
Monkeypox particles (red) on the surface of infected cells.Credit: NIH/SPL
Cases of monkeypox continue to rise. A month ago, when the World Health Organization (WHO) decided against declaring the global outbreak of the viral disease a public health emergency of international concern (PHEIC), some 3,000 cases had been confirmed in more than 50 countries since the start of May. By 23 July, that number stood at more than 16,000 cases across 75 countries and territories, according to the WHO.
The WHO’s expert advisers met again at the end of last week, and although the majority didn’t support declaring a PHEIC, on 23 July the organization decided to go ahead. Now that a declaration has been made, nations must work together to tackle the outbreak and ensure that sufficient resources are provided to low- and middle-income countries (LMICs), where the disease has historically been most prevalent. Mistakes made over COVID-19 must not be repeated.
For example, no one benefits when there is competition for vaccines during an emergency — a widespread problem in many nations’ COVID-19 responses. Smallpox vaccines are effective against monkeypox, but in LMICs both vaccine supply and diagnostic capacity are patchy. Vaccine donors need to collaborate with researchers and health officials to determine what each country requires to scale up its ability to respond to this infectious disease.
Monkeypox declared a global emergency: will it help contain the outbreaks?
When a PHEIC is declared, the WHO recommends that nations commit to ramping up the manufacture and supply of diagnostic testing, medicines and vaccines. Research also tends to get a boost from governments, universities and industry — as happened with COVID-19.
The advisers opposed to declaring a PHEIC argued that the disease is treatable through targeted interventions. At present, the burden of disease is overwhelmingly being felt among men who have sex with men, in Europe and North America, and interventions could focus on vaccination in that community. But those supporting declaring a PHEIC argued that the necessary criteria have been met: the outbreak is an extraordinary event and the disease is a global public-health risk that requires a coordinated response.
Until this year, most cases of monkeypox were seen in people in Central and West Africa. In the current outbreak, all of the known fatalities (at least 70 suspected deaths so far) have been in African countries, where studies have shown that young children, older people and those with low immunity have a higher risk of developing severe disease.
The Democratic Republic of the Congo has experienced thousands of suspected cases during the past decade, and in that time hundreds of people have died from a virulent strain that has a mortality rate of around 10% (Z. Jezek et al. Trop. Geogr. Med. 40, 73–83; 1988). But the true figures are not known — and could be higher than estimates suggest.
Monkeypox in Africa: the science the world ignored
In an all-too-common scenario, it has taken a health emergency in Europe and North America for the world to take notice of a disease. As Emmanuel Alakunle and Malachy Okeke at the American University of Nigeria in Yola write in a comment article in Nature Reviews Microbiology, the monkeypox outbreak should serve as “a wake-up call” that “highlights how little-to-no attention has been paid to the spread of the virus within endemic areas” (E. F. Alakunle and M. I. Okeke Nature Rev. Microbiol. https://doi.org/h5v8; 2022).
Last month, Adesola Yinka-Ogunleye, an epidemiologist at the Nigeria Centre for Disease Control in Abuja, told Nature that epidemiologists have been warning for some years that monkeypox is spreading. “The world is paying the price for not having responded adequately,” she said.
The PHEIC declaration presents an opportunity to right this wrong. High-income countries in particular must learn from mistakes made over COVID-19. In an emergency it is senseless to compete for vaccine doses and treatments. Instead, diagnostics and vaccines should be shared and targeted to where they are most needed.
In an interview with US National Public Radio earlier this month, Atul Gawande, the official responsible for global health at the US Agency for International Development (USAID) in Washington DC, said that the lowest-income countries tend to be the last to get vaccines. This is an important acknowledgement coming from a senior official at USAID, a major source of vaccines and treatments. There is little doubt that the world’s poorest and most vulnerable were failed during the response to COVID-19. Vaccines that offer protection against monkeypox exist and they need to be used for the benefit of all. Wealthy countries must not make the same mistake twice.

 Monkeypox declared a global emergency: will it help contain the outbreaks?
Monkeypox declared a global emergency: will it help contain the outbreaks?
 Monkeypox in Africa: the science the world ignored
Monkeypox in Africa: the science the world ignored








