Worldwide, almost half of women who are of reproductive age use contraception1. Another 171 million women — around 1 in 11 aged between 15 and 49 — do not use it, yet want to avoid pregnancy1. Several factors contribute to this unmet need. New, effective and more-desirable contraceptive options are urgently needed. Family planning is a key aspect to meeting United Nations Sustainable Development Goals 3 and 5.
Many women and men are highly dissatisfied with the contraceptives available2. Male condoms fail too often — in the first year of condom use, about 13% of women become pregnant3 — and women must rely on men. Implants and intra-uterine devices (IUDs) require medical procedures and can be invasive; pills have to be taken every day. Hormonal methods and non-hormonal IUDs can have side effects, including irregular or unpredictable menstrual bleeding, headaches, acne and weight gain, as well as depression and other mood changes4. For many women worldwide, contraception has been difficult to obtain or afford, even before the COVID-19 pandemic.
All of this has serious consequences. Around 40% of pregnancies globally are unintended, and about half of those end in induced abortion5. A high proportion of unintended pregnancies occur even where contraception is relatively accessible and cultural stigma against it is generally low, for example in North America (48%) and Europe (43%)5. Those pregnancies can happen because women aren’t using contraception, because their method failed or because it was used incorrectly. Nearly 25% of unintended pregnancies in low- and middle-income countries (LMICs) occur in women who were using modern forms of contraception6, and globally it’s an even higher share (see ‘Needs gap’).
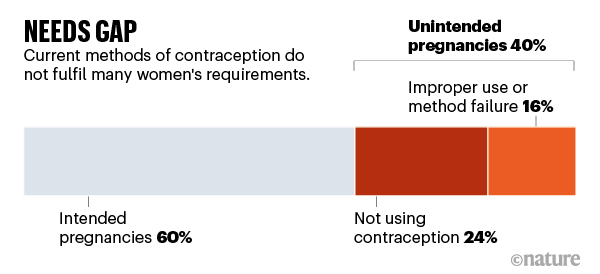
Source: Internal analysis by Avenir Health using multiple sources of global pregnancy data; funded by the Bill & Melinda Gates Foundation.
Unintended pregnancies can have lasting effects on women, children, families and society. The direct health-care costs in LMICs amounted to US$10 billion6 in 2019 alone; the indirect, longer-term economic costs could be 40 times that7. Estimates suggest that US unplanned births resulted in $21 billion in publicly funded medical costs in 20108. Progress in contraceptives research and development (R&D) has been slow in recent decades. Pharmaceutical companies typically spend around 20% of their sales revenue on R&D for new products9. For contraception, that figure is just 2%. We estimate that most of this spending has focused on incremental improvements to classes of hormonal contraceptive compound that have been in use for decades.
Encouragingly, there are now more opportunities than ever for innovation. Many scientific advances of the past decade can now be applied to developing non-hormonal drugs that target the egg, sperm or processes along the journey to conception. Such products could have fewer and less-severe side effects than current ones. And alongside daily oral pills, to meet the needs of women who want contraception for different lengths of time, various non-hormonal products with months or years of action could be delivered — through injections, implants, IUDs and other user-responsive systems that are currently in development.
At the same time, the COVID-19 pandemic is changing health-care services, possibly forever. Many of today’s contraceptives, such as implants and IUDs, require an in-person appointment10. New methods could be delivered remotely, directly to users.
A coalition of innovators, researchers, biopharmaceutical firms, donors and investors needs to come together now to produce better contraception for women. Many of the steps needed might catalyse innovation in male contraception, too.
Lack of satisfaction
The contraceptives available do not fully meet many women’s changing needs and preferences through their reproductive lives. Among women in LMICs who do not want to get pregnant but are not using modern contraceptives, more than one-quarter cite side effects as the main reason11. And the same types of side effect accompany many different products. Globally, about one-third of women discontinue their hormonal method of contraception in the first year of use, many citing side effects or health concerns as the main reason4.
Large-scale, detailed data are extremely sparse, especially from women who continue to use a method of contraception despite being dissatisfied with it. More than 100,000 women from nearly 200 countries completed a survey on contraceptive preferences within 1 month of its opening. (The survey was released through the reproductive-health app Clue and online at http://shapefuturect.org; it was developed by Avenir Health, where M.W. works, and funded by the Bill & Melinda Gates Foundation in Seattle, Washington, with S.E.G. as program officer). Early analysis suggests that a range of side effects would lead respondents to stop using a method, especially changes to mood, physical changes such as acne, weight gains of 2–4.5 kilograms, loss of hair and lowered sex drive. These findings echo others (go.nature.com/35hgqsm). A 2018 review showed that changes to heaviness or frequency of menstrual bleeding have all been associated with reported dissatisfaction with contraceptives12.
All of this probably helps to explain the enthusiastic responses to product launches over the past decade. For example, the Mirena family of products, a hormone-releasing intra-uterine system made by Bayer in Leverkusen, Germany, has maintained blockbuster sales of more than $1 billion for each of the past 5 years. An oral contraceptive introduced in 2011, Lo Loestrin, which offers the lowest amount of daily oestrogen available (with the potential for fewer side effects than for those of related products), captured a significant share of the market9 and net revenues have seen double-digit growth over time. In 2018, an app called Natural Cycles was approved as a contraceptive, and relies on body temperature to inform users when they are fertile. Earlier this year, Evofem launched Phexxi — a first-in-class vaginal pH modulator that works as a non-hormonal contraceptive. The impact of these two latest products will become clear over the next few years.

A women’s clinic in Cairo.Credit: Tara Todras-Whitehill/NYT/Redux/eyevine
Yet there are few truly innovative and highly effective contraceptive products in development. According to ClinicalTrials.gov, there have been 20–25 industry-funded clinical trials between 2017 and 2020. The majority focus on incremental revisions to existing hormonal products. By comparison, in 2019 there were about 3,100 trials for cancer drugs, 600 for cardiovascular drugs and 140 for treatments for eye disorders13.
Funding of R&D for female contraception comes from just a handful of players. These include the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Rockville, Maryland, the Bill & Melinda Gates Foundation (where K.M.V. works and S.E.G. recently worked) and the US Agency for International Development. Over the past few years, other organizations have funded or invested in specific non-hormonal technologies, including the BioInnovation Institute in Copenhagen and US-based RHIA Ventures and Adjuvant Capital. There’s room for many more.
Cycle of neglect
Why are funding and R&D so limited for female contraceptives? One reason is that they are given to healthy women of reproductive age, so the safety requirements for regulatory approval are (appropriately) very high: serious or severe adverse effects are not acceptable. Efficacy requirements are also extremely stringent. These regulations act as commercial disincentives for trying something new.
In addition, there are unique liability concerns for new products in reproductive health — especially in the United States, which is a litigious market. There have been a number of high-profile cases against leading contraceptive manufacturers, resulting in multimillion-dollar settlements (see go.nature.com/3ncb7jv). Vaccines are one of the only other product classes that are administered to a healthy population. However, in the United States, vaccine manufacturers are protected from liability under the National Childhood Vaccine Injury Act, established by an Act of Congress in 1986. This is unlikely to happen for contraception.
Another problem is that,from a business perspective, the contraceptive market seems to be healthy and growing. It was valued at $24 billion in 201814. Yet the demand from women for transformational change is not reflected as a reduction in sales. Furthermore, women’s health issues, and their preferences, are simply under-studied and under-funded, and unmet needs are ignored and misunderstood by those who could work to address these issues.
Six decades of struggle over the pill
These barriers — tight regulations, high liability risk and the lack of a strong market signal — fuel a false perception of low return on investment in contraceptive R&D. So, over the past 20 years, many global biopharma companies have sold off, reduced or closed divisions that were developing non-hormonal contraceptives and other women’s health products, such as those to support menopause. Companies have instead focused on therapeutic areas that are evidently fast-growing, such as oncology.
When drug firms step away from a field, it can start a cycle of neglect. Venture capitalists become wary of supporting technologies with unclear opportunities for exit strategies. Academics become cautious about pursuing an area with reduced commercial outlets and financial support. Private companies have few promising avenues to explore, and potential funders cannot easily identify where to invest.
For contraception, this has led to missed opportunities, because the scientific tools for R&D have mushroomed. Public-sector funding has been one of the key reasons the field has dodged dormancy (see ‘Funding gap’).
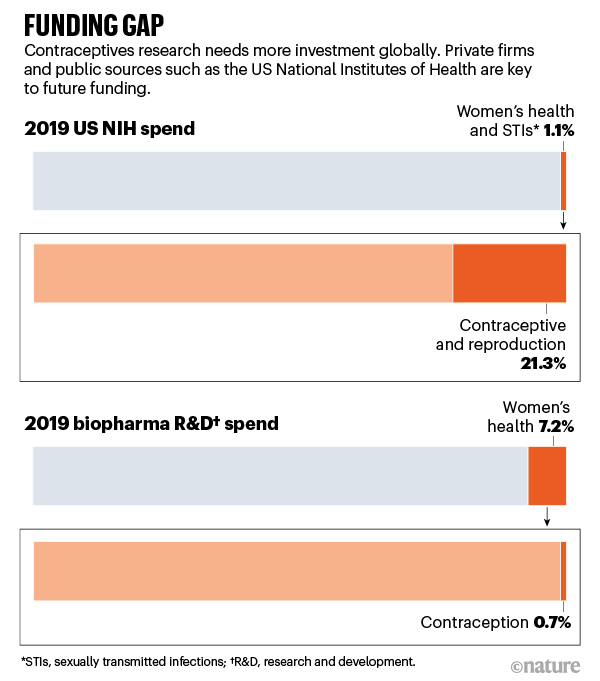
Sources: NIH/EvaluatePharma/BCG Analysis
Prime time
For the first time in a generation, a coalition of stakeholders could revolutionize the sector. For example, it is now possible to use genomics tools in a way that was not available 20 years ago. Operating costs have plummeted, and analytical methods and data sets have rapidly expanded in sophistication and size. Biostatisticians can comb for genes or proteins key to egg or follicle maturation, fertilization or gamete function. This can isolate targets for non-hormonal pharmaceutical interventions in a way that is much more efficient than previous, failed approaches.
The neighbouring fields of gynaecological oncology and infertility have seen industry funding increase over the past decade. Advances in those fields could help contraceptive R&D. For example, progress in understanding the mechanisms underpinning ovulation could help to identify potential drugs that could temporarily affect the same biological pathways.
Online tools also offer opportunities. Between 2015 and 2018, investors ploughed more than $1 billion into digital and diagnostic products and services that aid family planning, including menstruation and fertility-tracking apps (go.nature.com/2toj2vp). The sector is expected to be worth $50 billion by 2025 (go.nature.com/3pcswpt). Other apps and social media could help to create large-scale data sets articulating women’s needs, as long as privacy can be protected.
Key collaborations
Public–private partnerships will be key. The best innovation models in oncology, immunology and applied genomics, for example, engage industry in early stages. Such collaboration focuses research on saleable products targeted at consumer need. It also increases reproducibility of results, breaks down silos and brings in diverse perspectives to improve robustness. Without early buy-in, innovation efforts typically fall outside biopharma’s tolerance for risk.
Fresh thinking will also be needed to ensure that the latest contraceptive products get to those who need them most. For example, new non-hormonal contraceptives might require new manufacturing processes and are therefore likely to be priced higher than existing products. Revenue from high-income markets could subsidize affordable prices in LMICs15.
Women are most affected by pandemics — lessons from past outbreaks
Vaccine development is a good example of collaboration on product development that enables access by LMICs. Research communities such as the Collaboration for AIDS Vaccine Discovery focus on discovery. These bring the best scientists together, prioritize high-impact research and support the development of assays and model systems. To aggregate public, private and philanthropic funding, product-development partnerships have come together, such as the International AIDS Vaccine Initiative, the International Vaccine Institute and PATH Center for Vaccine Innovation and Access. These mechanisms drive innovation and significantly reduce the financial risk of early-stage investment. This type of infrastructure and collaboration has been crucial to the fast pace of innovation and development for COVID-19 vaccines and therapeutics.
Regulators, too, can help to lower the barriers to innovation. For example, once contraceptive drugs are well studied for safety and efficacy, developers might be allowed to use modelling, alongside clinical-trial data, in support of future products using the same drug16. Regulators might also need to consider how they assess effectiveness. A new non-hormonal product might have lower efficacy in clinical settings but have fewer side effects than some existing products, leading to higher acceptance and use, for example.
New funding is crucial to catalyse innovation in any sector. Venture funds, biopharma, biotechnology firms and universities should assess opportunities to apply their technologies and expertise to contraception, which could accelerate and increase innovations in R&D across multiple fields.
The public needs to speak up about its desires and demands, so that we can move from methods that women tolerate to those that actually satisfy their needs.
Success stories of new, reliable contraceptives with fewer side effects will create a virtuous cycle, spurring more funding and research and better options for consumers. A thriving contraceptive R&D ecosystem might also catalyse innovation in other sectors of women’s health: infertility, endometriosis and sexually transmitted infections, to name a few. What are we waiting for?


 Women are most affected by pandemics — lessons from past outbreaks
Women are most affected by pandemics — lessons from past outbreaks
 Six decades of struggle over the pill
Six decades of struggle over the pill